Education, Certification, Compliance: A Day in the Life of a Patient Advocate and Observer
By Robert P. Lee
This article originally appeared in the March 2024 issue of Healthcare Hygiene magazine.
Recently, I visited a seriously ill, hospitalized friend and colleague. He and I have collaborated on numerous projects in our careers and both of us knew the dangers of spending too much time in a hospital bed. The hand hygiene observed during my 48-hour visit seems all too common and acceptable at many hospitals. The medical staff was very professional, and I admired their responsiveness, care and empathy.
In this discussion, I will focus on the staff hand hygiene and its execution I observed during my visit. Of note, this hospital has an A rating from the Leapfrog Group.
Environment:
• Hand hygiene gel dispensers were deployed outside each room
• A second hand-hygiene gel dispenser was deployed just inside the doorway
• Soap dispenser but no gel dispenser at the sink
• No gel dispenser in the bathroom
Observations:
• Could not validate that each healthcare worker sanitized upon entry
• Some healthcare personnel sanitized upon exit
o Nursing often did “fly-bys,” attempting to sanitize but not properly activating the dispenser
o Physicians were not observed sanitizing upon exit
• Healthcare workers often touched IV station, workstations, etc., but no consequent hand hygiene prior to patient contact
• No hand hygiene prior to donning gloves or after gloves were removed
• Gloved healthcare personnel touched IV station, workstations, etc., without changing gloves prior to touching the patient
• No healthcare personnel used soap/water at the sink
• No environmental services (EVS) visits to perform a room cleaning or a cleaning of high-touch surfaces
• Nursing did not perform a high-touch cleaning
• High-touch cleaning was performed by family and the patient advocate
• Advised by nursing staff that this unit was one of the highest performing regarding hand hygiene.
Clearly, my observations suggested issues with compliance as well as with education and training. It was my impression that the staff were not reluctant to perform hand hygiene, and even welcomed their recognition as a high performing unit. However, as noted above, there appeared to be significant gaps in the staff members’ understanding of appropriate hand hygiene. What education and training could address the observed deficits? Here are some suggestions:
1. Establish and reinforce where and when hand hygiene is required during patient care:
a. WHO 5 Moments (entry/exit is inadequate)
b. Environmental contact prior to patient contact requires hand hygiene, even if hand hygiene occurred at room entry, and much like requirements in the operating room (OR), glove contamination requires re-gloving.
c. Develop a planned workflow: If you touch parts of the environment before patient contact, realize that this will require repeat hand hygiene.
i. Am I going in to adjust the IV pumps?
ii. Am I going to log into the electronic health record (HER)?
iii. Am I going directly to the patient?
iv. Will I be gloving?
2. Establish a high-touch surfaces protocol:
a. High-touch cleaning is required daily.
b. Define who will perform this cleanse, the healthcare worker or EVS personnel
Training/Education/Certification
Clearly, education and training is critical, and the best way to learn is through observation, where errors become valuable teaching opportunities, whether in a simulation center (if available) or observation and training at the bedside. Requiring each staff member to demonstrate knowledge and competence in appropriate hand hygiene during patient care via a practicum each year and consequent certification would assure a well informed and competent staff regarding hand hygiene. Technology can provide significant assistance with observation real time, with electronic monitoring and/or videotaping patient encounters to provide feedback and education as noted above.
Additionally, I would hope that the Leapfrog Group would enhance their survey to include EVS and high-touch surface protocols, just as they enhanced their hand hygiene protocols and guidance over the years.
Exceptional hand hygiene does not just happen and requires investment to support training that results in the outcome we all strive for, reduction in healthcare-acquired infections (HAIs).
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX- The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs. Lee may be reached at: medicaldatamanagement@gmail.com
Why is Exceptional Hand Hygiene Compliance Not More Effective in Reducing HAIs?
By Robert Lee
This article originally appeared in the February 2024 issue of Healthcare Hygiene magazine.
Your facility reports hand hygiene compliance of greater than 90 percent, ranked as one of the best by your state for environmental services (EVS), and your Leapfrog Group grades are all As. If this is your integrated delivery network (IDN) or hospital, one might ask why patients continue to acquire an infection during and after their visit to your hospital. The Centers for Disease Control and Prevention (CDC) reports, “Each day, approximately 1 in 31 U.S. patients and 1 in 43 nursing home residents contracts at least one infection in association with their healthcare, underscoring the need for improvements in patient care practices in U.S. healthcare facilities. While much progress has been made, more needs to be done to prevent healthcare-associated infections in a variety of settings.”1
Fast forward to 2023 and the post-COVID era, where rather than a decrease, there was an increase in HAIs last year despite our intense focus on universal precautions. Is hand hygiene compliance, environmental cleaning, and other interventions ineffective or is reporting inaccurate?
Focusing on hand hygiene compliance, the CDC reported that the average hand hygiene compliance in the U.S. is less than 40 percent.2 The goal of hand hygiene is to eliminate or greatly decrease microorganisms on hands and thereby prevent or significantly decrease the transmission of these potential pathogens to patients. If hand hygiene is performed before entering a patient’s room and soon after there is hand contact with a cell phone, tablet, bedrails, etc., hands can become colonized with microorganisms present on those other surfaces, and, of course, potentially spread those organisms to the patient if no hand hygiene is performed in the interval before patient contact.
Clack, et al. (2017) found that hospital personnel contaminated their hands by touching surfaces in the patients’ room within 4.5 seconds post entry.3 Therefore, even though compliant with hand hygiene prior to room entry, contamination occurred during non-patient environmental contact prior to patient contact. Returning to the preceding discussion, if your institution’s hand hygiene compliance score is 99 percent but you have environmental contact soon after entering the room before patient contact, what is the efficacy of such exceptional compliance in infection prevention? Consider behavior in the operating room; if anyone on the surgical team contaminates their gloved hands, an immediate glove change is required before any further contact with the patient, sterile instruments, or the surgical field. In surgery, hand hygiene guidelines are strictly enforced even after entering the patient’s space, in contrast to the behavior that often occurs in other patient-care areas.
What steps can be taken to adjust to this data and prevent hand contamination prior to patient contact? One obvious consideration in measuring hand hygiene compliance at the point of care (POC) rather than the doorway. Adding dispensers inside the room and improving training to change behavior to be more consistent with what occurs in the operating room where any break in technique requires re-gloving at a minimum would be a start. A torn or damaged glove in the OR requires repeat hand cleansing and re-gloving; the same approach to regular patient care would move us closer to more effective hand hygiene where it really matters (POC) and potentially enhance the outcome of all these efforts, a decrease in HAIs and improved patient outcomes and care.
Of course, this is not the only intervention or factor impacting HAI, but one of the factors within our control. Other considerations to enhance infection prevention include high compliance with environmental cleaning and disinfection, visitor and patient hand hygiene compliance, and controlling antibiotic use, etc. No single intervention alone is appropriate but rather, as noted by the Society for Healthcare Epidemiology of America (SHEA), a global and “horizontal” approach to the infection prevention interventions is within our control to achieve the ultimate outcome, reducing HAI.4
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs. Lee may be reached at: medicaldatamanagement@gmail.com
References:
1. CDC HAI Progress Report. 2022. https://www.cdc.gov/hai/data/portal/progress-report.html
2. CDC Hand Hygiene Core Guidelines. https://www.cdc.gov/handhygiene/download/hand_hygiene_core.pdf
3. Clack L, Scotoni M, Wolfensberger A, Sax H. "First-person view" of pathogen transmission and hand hygiene - use of a new head-mounted video capture and coding tool. Antimicrob Resist Infect Control. 2017 Oct 30;6:108. doi: 10.1186/s13756-017-0267-z. PMID: 29093812; PMCID: PMC5661930.
4. Septimus E, MD, Weinstein RA, Perl TM, Goldmann DA and Yokoe DS. Commentary: Approaches for Preventing Healthcare-Associated Infections: Go Long or Go Wide? Infection Control and Hospital Epidemiol. Vol. 35, No. 7, July 2014.
How Important is Hand Hygiene in the Use of Gloves, Masks, Surgical Drapes and Gowns, and other Medical Devices?
By Robert Lee
This article originally appeared in the January 2024 issue of Healthcare Hygiene magazine.
Infection prevention is not a singular intervention; as Septimus, et al. (2014) note, multiple interventions implemented simultaneously is recommended. And as Wohrley and Bartlett (2018) observe, “Horizontal strategies seek to broadly reduce the burden of common healthcare-associated pathogens including S. aureus, Enterococcus, gram-negative bacteria, and Candida through interventions such as hand hygiene and environmental cleaning.”
As a result, it is very difficult to determine the cause and effect of each intervention. We know that hand hygiene is a key component, but high levels of hand hygiene compliance do not always result in infection rate reduction. Why?
In this article, I consider the relationship between hand hygiene and medical devices such as gloves, masks, surgical drapes/gowns, etc., as well as explore how this relationship reduces or accelerates the risk of infection transmission.
Gloves
Why do you wear gloves and when do you perform hand hygiene? According to the Food and Drug Administration (FDA), “Use medical gloves when your hands may touch someone else's body fluids (such as blood, respiratory secretions, vomit, urine, or feces), certain hazardous drugs or some potentially contaminated items. Hand hygiene should be performed prior to and after removing gloves. Unfortunately, gloving has been used as a substitute for hand hygiene. Gloving protects the wearer, but improper glove use can result in pathogen transmission from patient to patient, patient to surfaces, etc. When reminding staff on how to use this medical device, many acknowledge and are appreciative, but an alarming number demonstrate that their only concern is their own protection.”
Masks
So, did you know that masking can both help prevent transmission of microorganisms or can accelerate the transmission of such organisms? You must ask which microorganism/pathogens you are trying to address. Is it viral or bacterial? Most masks are designed for bacterial not viral protection. Unless you are using a sheet of plastic, viruses will permeate your mask. Bacteria and viruses use vehicles such as liquid, moisture, particulate matter, blood, bodily fluids, even airborne dust, as well as hand contact, etc. So, if you are trying to prevent viral transmission, as in SARS-COV-2, and you are not sanitizing your hands, touching your face, your cell phone, and your mask, then you may be risking viral contamination. We are told to wear masks, but we are not told how to use this medical device properly. Thus, this can contribute to increased transmission. You must ask yourself, why are we not being told how to properly use masks if they are so effective in reducing the risk of catching and spreading a viral pathogen?
Evidence-based studies show the average individual touches his or her face 23 times per hour (Kwok, et al., 2015). Tajouri, et al, (2021) showed that 45 percent of cell phones carried SARS-CoV-2 during the pandemic. Do you think that individuals performed proper hand hygiene each time they touched their faces or handled their cell phone? Of course not. Think of a couple of common scenarios. How about your children at school who were required to mask, usually with a single mask worn all day. How about members of the public in a grocery store wearing masks and gloves, touching everything in sight and never doing hand hygiene? Watch television and you’ll see public officials or other personalities who are wearing and touching their masks but never doing hand hygiene.
Drapes and Gowns
Over the past 30 years, surgery has demonstrated the importance of barrier material and the science of sterile technique. The same principles as articulated above apply, but the difference in the operating room (OR) is that OR personnel revisit these principles during each case. They also hold each other accountable for maintaining proper technique. Surgical drapes and gowns are manufactured with the knowledge that fluid, blood, particulate matter, and touch are all vehicles for pathogen transmission. Drape and gown technology is focused on fluid penetration barrier performance while balancing comfort and drapeability. Materials are either permeable or impermeable; performance is matched to the expected opportunity for them to encounter blood, fluid, or particulate matter, as well as taking into consideration the length of case, risk of foreign bodies, etc. Even with all this technology, hand hygiene and hand hygiene science are important parts of the sterile process. Should hands become contaminated (usually gloved), rescrubbing may be required and/or re-gloving. Nevertheless, in the OR the hands play a pivotal role in the infection prevention chain.
So, considering the above scenarios, what should we take away from this article?
1. Use your critical thinking skills. Consider both sides of the equation, what is said and what is not said.
2. Understand the science and follow the science. Understand microorganisms and their mode of transmission.
3. Use your common-sense logic.
4. Audit your personal behavior and apply these principles of science and logic.
5. Come to your own conclusions. Don’t blindly accept what is pushed on you by the media.
I ask the question that if hand hygiene is the No. 1 way to reduce the risk of infection, why do we not get the correct guidance on how and, most importantly, when to perform hand hygiene? Additionally, with so many vehicles and modes of transmission of pathogens (cell phones, masks, etc.) with hands at the center, why are we not educated and made aware of how, when, and why hand hygiene is as important, if not more important, than using this medical device (masks, gloves, etc.)?
I am not against the use of any of these medical devices if they are used properly, training and education is provided (how to use and how not to use) and are supported by evidence-based research. Anything short of this I view as medical malpractice. We have been seriously uninformed for whatever reason and, as individuals, we have not assumed our responsibility to use our critical thinking skills to arrive at the proper conclusions. This lack of critical thinking has resulted in the loss of thousands of lives; many who might have been our own loved ones. So, put on your thinking cap and let the science, data and common sense set you free and maybe save your life.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX- The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs. He may be reached at: medicaldatamanagement@gmail.com
References:
Septimus E, Weinstein RA, Perl TM, Goldmann DA, Yokoe DS. Approaches for preventing healthcare-associated infections: go long or go wide? Infect Control Hosp Epidemiol. 2014 Sep:35 Suppl 2:S10-4. doi: 10.1017/s0899823x00193808.
Wohrley JD and Bartlett AH. Healthcare-Associated Infections in Children. Springer Nature. Published online July 16, 2018; 17-36. doi: 10.1007/978-3-319-98122-2_2
Kwok YLA, Gralton J, McLaws M-L, et al. Face touching: a frequent habit that has implications for hand hygiene. Am J Infect Control. 2015 Feb;43(2):112-4. doi: 10.1016/j.ajic.2014.10.015.
Tajouri L, Campos M, Olsen M, et al. The role of mobile phones as a possible pathway for pathogen movement, a cross-sectional microbial analysis. Travel Med Infect Dis. 2021 Sep-Oct;43:102095. doi: 10.1016/j.tmaid.2021.102095. Epub 2021 Jun 9. PMID: 34116242.
Integrated Delivery Networks and Hand Hygiene Compliance
By Robert Lee
This article originally appeared in the December 2023 issue of Healthcare Hygiene magazine.
A healthcare Integrated Delivery Network (IDN) is an assemblage of healthcare providers, including both acute (hospitals) and non-acute care sites (clinics, physician offices, surgery centers, long term care, etc). Supply chain systems and processes used in an acute-care hospital are not always effective in the non-acute care setting. Technology, workflow, supplies, information technology, data and skillsets of personnel can differ significantly. Two things are common to both sides of this equation, however: cost and quality/safety (infection prevention).
A question to consider is why? Within an IDN (and even within individual hospitals) are there various tiers of acuity and compliance with hand hygiene compliance? Why are rules, or at least compliance with accepted standards, different for downstream (non-acute care) and upstream sites (acute-care sites)? Even within an acute care setting, rules and/or compliance may vary among different departments, such as the OR, OB, MedSurg and ICU. Assessing the differences in these individual departments would be an interesting exercise as, if infection prevention is everyone’s responsibility, one would expect the entire IDN to be consistent across all departments regarding infection prevention.
Observations during several consulting engagements assessing hand hygiene compliance provided some insight into these issues. In one setting, the staff was observed working during patient care, both from different sites on the ward as well as during patient-to-patient care. Gloves were commonly employed but often there was no hand hygiene performed during glove changes and often less-than-ideal hand hygiene compliance. At a second major IDN in the central United States, physician, staff and patient-care workflow were assessed in an ambulatory setting. Hand hygiene technology was employed to track workflow during patient care for seven days, employing smart dispensers and smart ID badges to track hand hygiene compliance. The engagement resulted in restructuring of patient-care flow, but hand hygiene compliance for this 25-exam room physician clinic was less than 10 percent. At a large teaching hospital in the Southeast, our team measured hand hygiene compliance in the perioperative space. Despite the unit’s location contiguous to the OR, where hand hygiene and sterile technique are maximized, hand hygiene compliance was less than 17 percent. Finally, at a large IDN in the Southeast, consultation was requested to identify gaps in quality, focused on improving hand hygiene compliance and Leapfrog Group scores. The initial assessment suggested that this IDN would spend $100 million over the next five years to service their infections.
Returning to the question posed previously, why do the rules and compliance seem to differ upstream, downstream and inter-departmentally? To decrease healthcare-associated infection (HAI), there should be consistency in hand hygiene goals, performance and outcome (compliance) to decrease the morbidity, mortality and cost associated with HAIs. To reach these metrics there must be careful assessment of the differences upstream and downstream, as well as within individual departments in a single site. With this data, to enhance outcomes, there must be consideration of how we train, educate, and maintain appropriate and maximized hand hygiene compliance. Are our current rules and guidance sufficiently rigorous? One consideration is to develop a training program where all personnel are certified each year via classroom, on the job and, where available, simulation training, the last approach the most effective mode to demonstrate in actual practice the skills critical to effective hand hygiene, to protect both patients and personnel and decrease HAI. Finally, IDNs need to standardize both upstream and downstream infection control guidelines and expected, as well as appropriately assessed and documented, compliance in this important patient and staff safety protocol.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Are Supply Chain Executives Missing an Opportunity to Impact Patient and Staff Safety and Efficiencies?
By Robert Lee
This article originally appeared in the November 2023 issue of Healthcare Hygiene magazine.
When I meet with supply chain executives and their staff, I often receive questions such as, “Can you save us some money?” “Can you do some analysis on our current product mix and show us lower cost alternatives?” The answers to these questions are “Yes” and “Yes.” However, members of the supply chain must have a broader scope of cost reduction. Supply chain is the gateway to ideas, just as the emergency room and operating room are the gateways to initial patient interactions with that institution.
Is this your supply chain?

Model A

Model B
The modern supply chain organization has to be structured like Model B and led by executives who understand the holistic approach to this important resource. At the core of this model are the three C’s: Collaboration, Communication, and Creativity. We all know that collaboration and communication are key to a matrixed workflow, but why creativity? The supply chain executive must lead by example and encourage out-of-the box thinking and ideas on value to the organization and not just be focused on price. The evolution of the supply chain executive goes well beyond cost savings from contract analysis and implementation of more cost-effective contract options. The opportunity is being the organizational leader who finds, evaluates, and presents pragmatic solutions to senior executives that go well past product conversion and implementation.
The role requires a holistic approach that views the patient’s and the organization’s continuum of care. The view should be that what is best for the patient is congruent with what is best for the organization. For example, if there is a new surgical device that cost more but results in better outcomes (such as reduced length of stay, reduced number of infections, reduced procedure time, etc.), instead of the singular focus on the cost of the device; instead, the total impact of the device’s use presents a patient and financial benefit. To get at the overall analysis for the organization, it will require engagement with the various stakeholders in establishing metrics, tracking outcomes, and making sure results are validated. It requires assuming the role of the leader who presents to the organization opportunities that have been formulated with the key stakeholders, who will also be part of the initiative’s success.
So, let me present an idea that supply chain executives and their teams should investigate and why. The topic is systemwide hand hygiene compliance and surface decontamination. Current evidence-based studies (proprietary) indicate a 50 percent reduction in infections when an automated hand hygiene compliance technology is implemented. Additionally, evidence-based studies (yet to be published) around surface/room decontamination indicate almost a 99.9 percent reduction in contamination. Do you know what your facility infection rate is and the cost to service these? Working with data from the Centers for Medicare and Medicaid Services (CMS) and from the Centers for Disease Control and Prevention (CDC), and an integrated delivery network (IDN), it was determined that this IDN would spend $100 million over the next five years to service their current infections. By the way, the CMS data is only what has been reported, and this number could be higher.
So, here are some takeaways:
1. Are supply chains focused on the appropriate metrics?
2. Are supply chains structured to support other issues beyond cost alone?
3. How does your supply chain approach value analysis?
Is your supply chain just a purchasing group or is it a strategic resource that impacts both top-line revenue and bottom-line expense, while improving quality and safety for staff and patients?
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Prevention as Our First Line of Defense With Hand Hygiene as a Top Priority
By Robert P. Lee
This article originally appeared in the October 2023 issue of Healthcare Hygiene magazine.
With 99,000 deaths in the acute-care space annually and 400,000 deaths in non-acute space according to the Centers for Disease Control and Prevention (CDC), one would think that with all the interventions employed during the COVID-19 pandemic that we might see the needle move on these metrics.
We are under assault each day as organisms continue to evolve and adapt; some friendly and some not so friendly (pathogenic). We have become such a pill-focused society that much of our focus has been on pharmaceuticals and vaccines. So, why are our priorities reversed? Granted, prevention is not sexy, easy, and as profitable as a new drug (usually +95 percent margins), but prevention is unique in that it is universal to all microorganisms, non-specific, broad in scope, effective against all microbes (viral or bacterial), no side effects, and no profit margins or incentives except patient and staff safety.
One of the major reasons why prevention takes a back seat to pills is that it is a complicated, collaborative process. In speaking with infection preventionists they say, “It’s like herding cats.” I like to make the comparison of the job of infection prevention, particularly prevention, to going to the moon and to that famous quotation: “We choose to go to the moon in this decade and do the other things, not because they are easy, but because they are hard.” (JFK Library.org)
So, how do we prioritize prevention as the first line of defense and our top priority?
- Understand and align goals with the organization
- If patient and staff safety is a top priority, you will need to align and convince the powers that “prevention is the first line of defense”
- Research the tools /solutions that will help you accomplish your mission and accommodate your organization’s needs
- Understand tools you will need and what you want to measure
- This will require researching the commercial landscape of vendors and providers
- Put together a short list of your choices
- Remember not all technologies, platforms, etc. are created equal
- Do your homework: ROI, performance indicators (KPIs), metrics
- Preparing a strategy, both financial and operational, with measurable and achievable metrics.
- You need to measure what you plan to manage.
- Value proposition: Roadmap of how you going to get there
- Gather all your data, documentation, studies, etc. and organize into your narrative
- Make sure you support with current “evidenced based” studies for many studies lack credibility due to age.
- Prepare your presentation/pitch deck
- Pick your team of collaborators; what is in it for them?
- You want to surround yourself with Teammates that are passionate about your mission
- What’s in it for each one? Is there both a personal and Team gain?
- Make sure you surround yourself with good communicators that can articulate the goals and process.
- Seek an administrative sponsor/coach
- Find your executive sponsor.
- Generally, the chief quality officer, chief nursing officer, chief financial officer, chief information officer, etc.
If you have done all the above, you are now ready to execute on your plan. You will want to seek the help of your healthcare value analysis department or supply chain team to assist you in the RFP/bid/procurement process.
We will not cover the implementation portion here, for the intent of this article was to help you to prioritize prevention as the first line of defense in your infection prevention strategy. If you have any questions or needs, you can always reach out to me directly at: medicaldatamanagement@gmail.com.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Hand Hygiene Data, Analytics and AI: What is Your Strategy?
By Robert P. Lee
This article originally appeared in the September 2023 issue of Healthcare Hygiene magazine.
As hockey legend Wayne Gretzky says, “I don’t skate where the puck is, I skate to where the puck is going to be.” Knowing where the puck is going to be takes a bit of calculation, direction, speed, relative movement, weight of the puck, condition of the ice, etc. These are all data points that when processed provide an expected proximity and location for the puck. Bad data, tardy information, and lack of robustness will lead us in the wrong direction.
What role does analytics and near real-time data play in allowing us to target key activities that we know have a real effect on quality, safety and can impact healthcare-acquired infections (HAIs)? And how is this data presented and used by your management team to help to improve performance?
Before you get to the analytics and reporting, it is important to have a robust, accurate, and efficient “data capture” solution. The adage, “Garbage in garbage out” is so true. Typically, the gathering of hand hygiene compliance data can be manually collected on a clipboard. Some will use an iPad. Nevertheless, a manual input of data is required, which can open the door to errors and inefficiencies. Additionally, the scope of data is very limited to this human resource. The Leapfrog Group recommends that at least 200 events be captured to meet their survey requirements per unit.
One way to multiply your data gathering task is to use hand hygiene technology. This standardizes and accelerates the data-gathering process and can provide more accurate results in a fraction of the time. Some technologies require permanent installation, while others are “portable” and can be installed, de-installed, and re-deployed in a few hours, moving from unit to unit. Additionally, The Leapfrog Group recommends that you validate the performance of your tool via audit each time you install/de-install.
So, once you are comfortable with your data-gathering process, it is time to put the data to work and into the analytics platform, which organizes, sorts and prepares the data for reporting.
So, how do you want your management team and end users to receive their reports? Should it be via email, text message, or through a dashboard? Should it be delivered weekly, daily, or near real-time? How do you want to use this reporting functionality? To track performance, for training and education purposes, to document operational and clinical health of the team, or to track as it relates to infection rates?
As far as analytics, determining trends and relationships is an important function used to become more predictive versus retrospective. We want our data to move faster than the process itself so that we can anticipate appropriate interventions and take preventive measures. We might want to know the relationship in hand hygiene between nurses and doctors, other clinical service staff such as environmental services or dietary, and others such as visitors. This might include different shifts, weekends versus weekdays, duration of shifts, etc.
What is artificial intelligence (AI) and how does it apply to hand hygiene? AI is simply taking all this good data and analytics and providing additional direction as an output. It’s called machine learning. The information is stored and managed in such a way that it allows the AI platform to think ahead as to next steps and activities. It allows us to become more predictive, which is one of our goals. While in today’s healthcare setting, many clinicians are working tirelessly with fewer resources, in the old days, nurses use to work in teams called “the buddy system.” Technology is an important part of “the buddy system,” especially when there is no back-up resource to ensure quality and safety. When trying to achieve high performance and compliance with safety protocols such as hand hygiene, wouldn’t it make sense to have a technology assistant reminding you when to sanitize your hands? It might be an audible, visual, or a voice reminder.
Do you subscribe to the “command center” concept? This concept is a live/real-time dashboard of hospital health and quality. Does your compliance data feed into your electronic health record (EHR)? Every infection prevention office or department should have a real-time feed (command center), broken down by hospital, department, and unit, with drill-down capabilities to individuals.
If we are going to ask our staff to do more with less, does it not make sense to invest in assistance that makes them better? One should not fear “Big Data” or AI; it is your friend and ensures that you are doing the right things at the right time.
Epidemiology and infection prevention need and deserve the opportunity to bring practice into the 21st century. Clinicians deserve access to resources and funding to help them fight hospital infections and antibiotic resistance. Data is the new currency in the marketplace, and clinicians need to access that information efficiently, accurately, and in real-time. Administrators, please support your epidemiology and infection prevention teams when they ask for funding and resources.
Robert Lee, BA, CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX-The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Hand Hygiene: Visitor Hand Hygiene Compliance and the Infection Prevention Chain
By Robert P. Lee
This article originally appeared in the August 2023 issue of Healthcare Hygiene magazine.
A common refrain pertinent to the infection prevention chain is that each segment is only as strong as the weakest link. Pathogens spread through the hospital ecosystem via carriers, most commonly hospital personnel and patients, and hands are the most common vector of transfer. A major component of the infection prevention chain is the education and training of staff and recently the investment in technology to sustain and improve hand hygiene compliance. However, another important potential link in the infection prevention chain is the transfer of pathogens by visitors, often given inadequate consideration.
In my anecdotal experience visiting hospitals, visitor hand hygiene is seldom if ever a consistent focus of infection prevention programs. Pitts, et al. noted that staff hand hygiene compliance is generally 25 percent to 40 percent while visitor hand hygiene is usually less than 1 percent. A recent study by Kaya, et al., noted: “Of patient companions and visitors, 96.2 percent stated that they did not receive training on the importance of handwashing during their stay in the hospital.”
Several investigators have addressed some of the issues surrounding visitor hand hygiene and the challenges that result in such low hand hygiene compliance. Hobbs, et al. noted the lack of placement of hand sanitizer dispensers where visitors commonly enter the hospital, typically the front door of the hospital. Further, hand sanitizing displays in the hospital entrance alone would help raise overall visitor hand hygiene awareness and knowledge of its importance and potentially increase visitor compliance. Visitors (and often patients) receive little if any education and training in hand hygiene, such as the why, how and when.
What might be some practical options to address some of these challenges?
A common requirement for all visitors entering the hospital patient-care area is to secure an identity badge as they pass through security. What if part of this process was to require new visitors to watch a brief one-minute video addressing the importance of hand hygiene? Certainly, the COVID-19 pandemic raised the issue of the importance of prevention of pathogen transmission among members of the general public. Further, most visitors to the hospital are coming to see friends and family, and preventing infection could and should be an important aspect of such visits. It seems an unrealistic expectation of visitors to understand the importance of hand hygiene without providing appropriate information and the means to address the problem, as noted above.
They then can take this certification to security check in and receive permission to enter the hospital. If the hospital is a subscriber to hand hygiene technology, visitors could at that time receive a hand hygiene compliance ID badge. This badge will remind them when to sanitize their hands. Additionally, it will provide tracking information and contact tracing should these features be necessary.
This process is a start, an opportunity to address one weakness in the chain of infection prevention, seldom currently a high priority at most hospitals. It is an opportunity to both provide visitors with the knowledge of the importance of hand hygiene in infection prevention and hopefully easy access to hand hygiene before visitation. If current visitor compliance is truly less than 1 percent, there is really only one way to go.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Moving Hand Hygiene-Product Dispensers Closer to the Point-of-Care
By Robert P. Lee
This article originally appeared in the July 2023 issue of Healthcare Hygiene magazine.
As we continue to work with our clients, the most common reasons noted regarding the challenge of lower-than-expected hand hygiene compliance are hand sanitizing dispensers not being available, lacking easy access, being empty, being non-functional, and not dispensing the correct amount of sanitizer. This is a universal problem that needs to be understood and addressed.
The first two dispenser-related challenges noted above question the logistics and placement of sanitizer dispensers. In terms of these issues, there is one question to consider: Is your sanitizing dispenser footprint designed on entry/exit or the World Health Organization (WHO) Five Moments protocol? Some programs are employing the Five Moments protocol, but their dispenser footprint is entry/exit, where dispensers are set at the doorway and the sink area.
A WHO 5 Moments dispenser workflow design would place dispensers at the sites indicated in blue in Figure 1 below.
Moving the dispensers closer to the point of care (POC) makes it easier for staff to sanitize hands and eliminate unnecessary steps, as 70 percent of all hand hygiene opportunities occur inside the patient room, studies have found. Consider asking your vendor to add additional dispenser sites, as these dispensers are no-charge items.
The third, fourth and fifth dispenser-related challenges mentioned earlier are a consequence of inadequate maintenance and servicing of your dispenser platform. If this is an issue, an important consideration is your method of maintaining your dispenser’s function and solution supply. One approach is manual, where hospital staff (typically environmental services personnel are the most commonly responsible professionals for this task) check each unit or, in some units, the unit team checks prior to shift change or the charge nurse is responsible for validating the sanitizer platform.
Can technology play a role? Many hospitals are beginning to employ hand hygiene technology to measure hand hygiene compliance. A byproduct of this technology is the assessment and maintenance of “smart” hand hygiene dispensers. Each dispenser records the number of times that it is activated and alerts staff when a solution refill is necessary. It also identifies dispensers that are inoperative and require attention and potentially repair. Considering the critical importance of dispenser function for effective, compliant hand hygiene, technology may be a viable solution to compliance and maintenance issues.
It’s all about the data. What kind of good data and insight can be gained? What do analytics tell us?
Firstly, you must measure the right thing. If your footprint is set up around entry/exit, that is what you are measuring. So, what happens though once you enter the room? If you set your footprint to measure the WHO 5 Moments, then your metrics and analytics will provide you with more granular data and a more exact measurement of your hand hygiene compliance, patient room health and your sanitizing station readiness.
Remember, data is the new currency in the marketplace; as W. Edwards Deming has said, “You can’t manage what you can’t measure.”
So, in this article we have addressed some ideas that will not only enhance your current hand hygiene compliance, the acceptance of your efforts to improve performance, your dispenser service and maintenance, but also to help you to convert from entry/exit to the WHO 5 Moments methodology.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX -The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Hand Hygiene and Surfaces: The Case for Big Data, Lean 6-Sigma and Improved Standardized Training and Education
by Robert P. Lee
This article originally appeared in the June 2023 issue of Healthcare Hygiene magazine.
Hand hygiene is not handwashing but rather the execution of cleaning and sanitizing one’s hands properly at critical times during patient care. Unfortunately, achieving this goal at a high level of compliance has proven difficult. Sanitizing your hands upon entering a patient’s room and then using the keyboard of a workstation, handling a patient chart, or touching anything in the room prior to touching the patient can negate the impact of hand sanitization and potentially acquire a pathogen that can then be transferred to the patient during contact. Entering a room and quickly activating a dispenser but never ensuring that a proper amount of sanitizer is dispensed and that the dispensed solution is properly dispersed and spread over the surface of the hands can also negate the value of hand sanitization.
Part 1: Sanitizing Your Hands
Guidelines for appropriate hand hygiene are widely available and an important component of infection control training and reinforcement. Recently, the Society for Healthcare Epidemiology of America (SHEA) published some newer guidance focused on fingernails, polish, fingertips and maintaining healthy skin (Infection Control & Hospital Epidemiology 2023, 1-22). Because healthcare personnel average about 200 hand-hygiene opportunities per shift, compliance and proficiency are critical and challenging. Sanitizing hands this many times per shift can cause skin damage which can both impact compliance and increase colonization with potential transferable pathogens.
Part 2: When Should I Sanitize My Hands?
The question I would like to ask is, “If your child, parent, grandparent, or significant other happened to be flying on an airplane today, and you were told that airplane conformed to the minimal standards of safety and airworthiness, would you let your family fly on the aircraft?” The point I am trying to make is that the standards established by organizations are minimal standards of performance, not maximum standards.
The traditional minimal standard of timely hand hygiene sanitization is the concept of entry/exit, or sanitizing hands upon entry to or exit from a patient room. The World Health Organization (WHO) defined the minimal standard of hand hygiene centered on the 5 Moments (See illustration). This approach adds other instances requiring hand hygiene, such as contact with equipment or surfaces in the patients’ environment. The recognition of potential contamination “beyond the doorway” addresses the issue of hand contamination after hand hygiene prior to entering the room and subsequent contamination of previously sanitized hands with potential pathogens when touching surfaces in the patient rooms. Although this expands the need for hand hygiene in new situations, it also offers a more effective method to avoid transfer of potential pathogens in the patient care environment.
Part 3: Process Improvement
Pathogens don’t have legs but we give them legs, as our hands and surfaces provide mobility for pathogens. A critical component to address the issue outlined above is a performance improvement team. Enhancing your infection prevention and control program and potentially moving to the 5 Moments guidelines should precipitate engagement with Lean 6 Sigma to assist your endeavors. You should engage them to provide Lean 6 Sigma for the unit that you hope to implement your hand hygiene compliance strategies. Collect good data on current state and project your future state by applying “lean principles” to your unit (lean process) and eliminate any opportunities for error (6 Sigma).
Now you can establish the proper hand hygiene protocol for that unit. You can also train staff on what are the scenarios that require hand hygiene and when. An example might be:
1. Sanitize hands upon room entry
2. Approach the workstation and enter patient information
3. Sanitize upon leaving workstation and prior to patient contact
4. If there is patient contact, sanitize after touching the patient and before touching anything else.
5. If leaving the patient, sanitize upon exit from the room
Note: Hand hygiene is performed when interaction between surfaces and patient, patient and surfaces, and surfaces and surfaces.
Now you can train and educate staff members on that unit. With the workflow standardized to a point, one can easily teach and educate the staff on when, where and how to practice hand hygiene. You will also know exactly what you are measuring, and compliance data will be much more accurate and meaningful. Of course, there will be exceptions, as patients come first. Muscle memory and habit will improve over time when hand hygiene is defined effectively to match the standardized training and education process.
To summarize, each unit workflow is different. Before you begin to measure hand hygiene compliance, you must understand your workflow. Where do your key hand hygiene opportunities exist? Gather this data with your team and establish standardized protocols. Then overlay a compliance measuring tool. Use this data to improve performance. Remember, each unit has a unique workflow unless you standardize universally.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX- The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Hand Hygiene Compliance Monitoring Technology: Buy, Lease, Outsource, SaaS … What’s Right for You?
By Robert P. Lee
This article originally appeared in the May 2023 issue of Healthcare Hygiene magazine.
Why are infection prevention and environmental services departments the last place where hospital administrators want to spend money? Why must infection preventionists (IPs) utilize clipboards, spreadsheets, volunteers, poorly trained observers, and a manual methodology to monitor hand hygiene, the most effective method to prevent healthcare-associated infections (HAIs) and protect patients?
This discussion is designed to help IPs evaluate the technological choices available to address hand hygiene monitoring as an alternative to the manual method. Important considerations include current challenges to more effectively address the requirements of hand hygiene compliance and your institution’s situation and objectives. Choices include purchase, lease, outsource or continue your current program.
Here are some of the questions to consider:
1. What is your institution trying to accomplish and what type of help/resources are necessary to meet your goals?
2. Is your approach to create your own system or purchase a proprietary system?
3. If your goal is to create your own system, how will you design, implement and maintain it?
4. If you decide to purchase a system, will you buy, lease, outsource, or other (software as a service or SaaS)?
The Purchase Option
This is the most straightforward approach. Each system component has a cost and sell price, and, depending on the system, potentially a distribution cost. Each system will vary in price, depending on your footprint design. It is therefore critical to understand your hand hygiene compliance footprint, meaning what you want to measure and what you want to achieve. The hand hygiene compliance footprint is a designed workflow that is mapped as well as standardized to efficient workflow and hand hygiene protocols. (The choice and design of an appropriate footprint will be considered in a future column.)
Once you have itemized the parts, you need to consider other costs:
• Service costs, including parts and maintenance, warranty and customer support
• Lost, damage and theft
• Technology upgrades
• Installation and de-installation
• Additional consulting
When you choose to purchase, you own the technology and it is considered a capital expense, usually considered and procured through the capital expense process; this is usually a competitive process among different departments with the performance of a needs assessment.
Leasing Hand Hygiene Technology
Leasing is another consideration, which is essentially renting the technology for a period of time at a specific rate. Leasing can include a lease-to-buy scenario, where a portion of your lease payments are allocated to the purchase of the technology. Leasing helps to avoid the capital expense process, as leases are generally allocated to operating expense as an ongoing cost. Additionally, all the other costs noted above are operating expenses.
Leasing may be a practical choice to avoid competition for capital, lock in a fixed term of service, potentially accrue equity in the technology, and upgrade or change the technology in the future.
Outsourcing Hand Hygiene Technology
You may also consider a software as a service (SaaS) model. In this model you neither purchase nor lease the technology but choose a company to provide complete access to hand hygiene compliance services for a fee.
A SaaS model for hand hygiene technology provides all the benefits of leasing, as your firmware and software are updated automatically and seamlessly, and all the other service features of a lease agreement are included. With the current rapid development of new technology and needed software updates, SaaS agreements are the current standard. Whatever approach chosen when adding a technological approach to a hand hygiene program, a cloud-based platform is essential, as hand hygiene technology is so data intensive, it requires each individual sensor station to communicate efficiently, accurately and instantly.
In summary, depending on the size and resources of your institution, there are several business approaches to the acquisition of hand hygiene technology. A smaller hospital where the infection prevention department comprises a single person, technology enhances the ability to collect robust, performs 24/7, is a force multiplier for IPs, and may make clinical and economic sense. In large integrated delivery networks (IDNs), technology allows IP to target their influence and enhance teaching and education, rather than collecting and analyzing data that is more effectively and efficiently collected via technology.
A final consideration is to engage a vendor in a risk/share/gain agreement. Such agreements can align your goals and metrics with the supplier and provider, a means to pay for your hand hygiene technology, as well as provide an ROI and expense reduction for your system.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology and AI to reduce risk of HAIs.
Hand Hygiene and Surfaces: Are Your Education and Training Efforts Doing Enough to Move the Needle on HAIs?
By Robert P. Lee
This article originally appeared in the April 2023 issue of Healthcare Hygiene magazine.
Could your training and education be doing enough to support your integrated, collaborative approach? Let’s look at your current state first and then we can explore some ideas to consider.
In the military we always say, “You train as you fight.” In coaching, we say, “You practice like you play.” We are in a battle with pathogens, the unseen enemy, and don’t seem to apply the same principles, techniques and resources necessary to win the battle. What did we witness with COVID-19?
In a previous columns we spoke about both vertical and horizontal approaches to addressing hospital-acquired infections (HAIs). The vertical approach attempts to identify the pathogen and then to implement treatment for that pathogen. A horizontal approach addresses infection on a more broad, non-specific approach where interventions do not target a specific pathogen. Vertical is more tactical and horizontal is more strategic. With this article, we will attempt to illuminate an important horizontal approach, education and training, which is so important, but apparently severely under-resourced, in need of re-thinking and requiring your utmost attention.
In a recent survey conducted by our organization, we asked the following questions to hospital personnel:
1. How important is hand hygiene to patient safety and staff safety?
2. Do you know your current hand hygiene compliance?
3. Is it based on the WHO or CDC minimum standard?
4. What is the difference between OR sterile technique principles and your current technique?
5. What training/education did your receive on sterile technique, prior to and during your employment?
6. Do you have to demonstrate your current sterile technique in a structured controlled setting such as a simulation center?
The answers were the following:
1. Yes. 99 percent answered and recognized the importance of hand hygiene
2. No. 95 percent did not know their compliance
3. No. 97 percent did not know the methodology followed.
4. No. 95 percent said that they got training in nursing school on operating room technique but that floor nursing didn’t apply OR standards
5. No. 95 percent said no additional training in sterile technique, although occasional training on hand hygiene
6. No. 98 percent said that their competency never used a simulation center to validate.
So, are we teaching the wrong thing? Should we be teaching a higher level of performance? Are we not using our resources to best optimize performance? Are we holding ourselves accountable and training to a higher standard?
Did you ever wonder why hand hygiene compliance and sterile technique is typically higher in nurses that come from an OR background? Let me define “OR sterile technique” for the purpose of this column. OR sterile technique is the logical understanding, awareness and practice of movements by personnel to prevent the introduction and movement of pathogens within the OR space. For the purpose of this article, I shall exclude handwashing/scrub protocols for they are different for OR and floor nursing. However, once “scrubbed in,” the principles are the same. What are you doing with your hands and what are you touching -- whether un-gloved or gloved -- are vehicles for the pathogens to become mobile.
We need to raise the bar from minimum standards to evidence based standards in our education/training programs. As they also say in surgical training, “See one, do one, teach one.” Here are some suggestions:
1. Create a culture of evidence-based training/education, with minimum standards being unacceptable
2. Elevate all your techniques/protocols to the OR standard of sterile technique
3. Use technology to provide real-time data on performance improvement
4. Use scorecards, dashboards and feedback tools to reward performance and identify need for additional training/education
5. Consider using a simulation center to train, educate and monitor actual knowledge in a structured environment
6. Utilize an annual certification process in which individuals should be required to pass a written and practicum annually for hand hygiene and sterile technique proficiency
7. Reward and recognize by incentivizing individuals. An idea would be our “gold star” patient safety performance ID badge. Note: three gold stars indicate trained, certified and current performance criteria achieved.
How do you use your simulation center to assist you?
• To establish your training and education best practices as a collaboration
• Every staff member must pass through and demonstrate proficiency within the practicum
• Certification and re-certification for all nursing, physicians, and other healthcare personnel
• Remedial education/training/re-training
• New hires, temps, and administrative personnel must be certified
• If compliance technology used, the technology should be installed in the simulation center.
In summary, we need to do more. We need to raise the bar. We need to be aggressive and creative in our approach to fighting pathogens. Pathogens have no rules.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Hand Hygiene and Surfaces: How a Performance Improvement Team and Lean 6 Sigma Methodology Helped to Improve Hand Hygiene Compliance and Eliminate Practice Errors
By Robert P. Lee
This article originally appeared in the March 2023 issue of Healthcare Hygiene magazine.
There’s a saying that pathogens don’t have legs, we give them legs. When we can limit their mobility, we lower the risk of infection. When the pathogen cannot reach the host, it eventually dies. So, why are we still experiencing more than 2 million infections per year and more than 100,000 deaths in the acute care setting and 400,000 deaths in the alternate-site setting, according to the Centers for Disease Control and Prevention (CDC)?
Hand hygiene is considered the No. 1 preventive methods for reducing the risk of infection. Hand hygiene is a process of sanitizing your hands and doing this at the proper time. Within this article I would like to address and focus on the latter at the proper time.
For this exercise, we called upon our performance improvement team and their Lean 6 Sigma playbook. Lean is the performance improvement process of eliminating “waste” and redefining a correct process. When married with 6-Sigma, chances for error and mistakes are identified. The engagement begins by selecting the correct cross functional team to participate. We then begin “the current state” analysis, which is collecting data on current activities and mapping this to a workflow pictorial called a “spaghetti diagram."
Step 1
Assess the current state
Step 2
• Identify improvements in workflow eliminating wasted steps and opportunities for errors
• Standardize workflow process for all rooms
• Relocate and move assets to the same place in each room
• Align this standardized process with hand hygiene process, so that hand hygiene is performed the same for each room
• Allocate and relocate dispensers to the most efficient location
• Should a dispenser be placed at the bedside? Next to a workstation?
Step 3
• Establish metrics
• Measure results
• Repeat the process
Most hospital workflows vary so much, even from unit to unit, that it is challenging to train staff; many are temps and travelers. The purpose of the lean process is to create a standard workflow and work footprint where with minimal training and orientation, the staff does not have to adjust to variations in these workflows, creating a chance for error and non-compliance. An example of where we used this concept is the emergency department (ED). By mirroring each room as an identical reflection of best practice, ED personnel don’t have to think where items are. They are there every time. In an emergency, you don’t have time to think; your training, memory and habits take over.
By identifying the correct process and labeling when to execute proper hand hygiene for that unit, a high level of proficiency and compliance can be achieved. The pain of change in behavior no longer exists because routine and habit become natural. We must make it easy to be compliant by giving our teams the proper workflow, aligned with proper hand hygiene to be successful.
In conclusion, give your performance improvement team a call and try to engage with them in a project. It will not only be productive it will be fun.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX- The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
The Intersection of Infection, Immunity, Therapeutics, Nutrition, Prevention and Data
By Robert P. Lee
This article originally appeared in the February 2023 issue of Healthcare Hygiene magazine.
Merriam-Webster Dictionary says that infection is “the state produced by the establishment of one or more pathogenic agents (such as a bacteria, protozoans, or viruses) in or on the body of a suitable host.1 The reaction between the pathogen and a host is critical to the ultimate outcome of any infection. Indeed, it is the host response that results in the symptoms of infection. As a pathogen multiplies, the host’s immune system responds to the microorganism and its toxins with the clinical symptoms of infection, e.g., fever, chills, malaise, etc.
The healthcare community is focused on treatment, but prevention is equally, and in some instances -- such as the COVID pandemic -- more important. There is an amazing array of antimicrobial agents available to treat infections in U.S. healthcare settings. However, preventive endeavors are both more difficult and time intensive than simply administering a medication. Microorganisms can evolve quickly to antimicrobials, often becoming resistant to these agents through acquisition of genetic factors that inactivate or prevent an antimicrobial’s ability to assist the immune system and eradicate a pathogen.
An effective defensive structure against infection might be garnered from our military and their defense of high-value targets. Through the deployment of a series of rings and barriers they attempt to thwart any enemy rather than engage in battle. Is infection prevention the use of the same principles to protect patients?
The Rings of a Good Defense
Data, accurate and real time, is essential, as early intelligence is the backbone of any defense. Examples might include better public health resources, central databases and dashboards, etc. Critical information can be manipulated and limited but accurate, raw date is often critical to provide health care professionals usable and actionable information to initiate the appropriate interventions to both prevent infection and treat patients.
Nutrition can also impact the effectiveness of our immune systems to both prevent and, if prevention fails, treat patients’ infections. One of the critical components of infection prevention and response to infection is an intact immune system. Patients with immunodeficiency are much more vulnerable to infections, and hence, any intervention that improves immunocompetency can improve resistance to and hence prevention of infection.
Prevention is the third ring of defense. If a pathogen is prevented from reaching the patient, then we avoid both the necessity of treatment as well the risk of morbidity and mortality.. Two critical methods of prevention are hand hygiene and surface cleaning. Hands can provide a mode of transmission of pathogens from a surface or another patient with an infection to another, initially uninfected patient. Surfaces in the patent’s environment are often contaminated with microorganisms and may serve as a reservoir of pathogens. Proper disinfection of a surface/area reduces bioburden and consequently prevents a healthcare worker’s acquisition of that organism via hand contact with subsequent potential transmission to a new host. Proper hand hygiene is a second critical component of prevention, as it can eradicate or, minimally, reduce the numbers of microorganisms present. Of importance, these two interventions act synergistically to prevent infection.
Vaccines can also effectively prevent infection, but are only available for certain infections, such as common childhood infections such as measles and mumps, as well as other infections that may affect all age groups, such as influenza and COVID. A vaccine is antigenic material that precipitates an immune response specific to that pathogen, but does not harm the host or precipitate the actual infection, resulting in memory cells and antibodies that are available to the host’s immune system should the host encounter that specific pathogen in the future. Indeed, vaccines have had the greatest impact on disease prevention and the increasing longevity of populations.
Therapeutics, as noted above, are the antimicrobial agents used to treat established infections and in certain instances, such asd surgical prophylaxis and patients with compromised immune systems, prevent infection. These agents are critical in the treatment of infection when our preventive efforts fail.
Immunity is the immunologic and cellular responses to foreign antigens, in this example an infectious agent. This coordinated response is critical to protect the host from the foreign antigens that an individual is exposed to during their lifetime. In some cases, previous vaccination or previous infection with a pathogen results in the production of antibodies specific to that previous exposure. When re-exposed to that pathogen, memory cells are recruited that code for the production of the antibodies specific to the previously encountered pathogen. This results in the coordinated recruitment of the immune system to address and eradicate the infecting microorganism before they multiply and cause a clinically evident infection. When infected by a pathogen to which the host has no previous experience, a much more complicated immune response occurs, leading over a longer period of time to the production of antibodies as noted above.
Many individuals are more prone to infection, e.g., the very young, the very old, those with chronic disease, the immunocompromised, surgical patients with the interruption of their cutaneous protective barrier, and even presence in a hospital where antibiotics and severity of illness create an environment with resistant pathogens. Preventive efforts (the front end) become a critically important method to avoid infection, a much more effective intervention than treating an infection (the back end), often with resistant pathogens.
In summary, hopefully this discussion outlines the factors to be considered when discussing infections. Further, it also provides some insight into treatment versus infection and both the challenges and the value surrounding preventive interventions.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX- The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
Hand Hygiene and Environmental Hygiene: Making the Case for Automating and Implementing Simultaneously to Move the Needle on HAIs
By Robert P. Lee
This article originally appeared in the January 2023 issue of Healthcare Hygiene magazine.
Septimus, et al. (2014) note that “Over the last decade, the general approaches to healthcare-associated infection (HAI) prevention have taken two conceptually different paths: Vertical approaches that aim to reduce colonization, infection, and transmission of specific pathogens, largely through use of active surveillance testing (AST) to identify carriers, followed by implementation of measures aimed at preventing transmission from carriers to other patients, and horizontal approaches that aim to reduce the risk of infections due to a broad array of pathogens through implementation of standardized practices that do not depend on patient-specific conditions. Examples of horizontal infection prevention strategies include minimizing the un-necessary use of invasive medical devices, enhancing hand hygiene, improving environmental cleaning, and promoting antimicrobial stewardship. Although vertical and horizontal approaches are not mutually exclusive and are often intermixed, some experts believe that the horizontal approach under usual endemic situations may offer the best overall value given the diversity of microorganisms that can cause HAIs and the constrained resources available for infection prevention efforts. When informed by local knowledge of microbial epidemiology and ecology and supported by a strong quality improvement program, this strategy allows healthcare facilities to focus on approaches that target all rather than selected organisms in the absence of an organism-specific epidemic.”
The authors of this paper clearly understand that a single intervention will not move the needle on HAIs to the point where HAI reduction is measurable, and cause-and-effect can be assigned. As we know from Deming, “If you can’t measure, you can’t manage,” or put another way, “You can’t manage what you can’t measure.” So, what if we take two interventions and combine their attributes and link their data; these two are hand hygiene and environmental hygiene.
Let’s start with definitions. What is hand hygiene? Hand hygiene should not be confused with handwashing. Hand hygiene is the methodology, understanding and the execution of sanitizing your hands at the right time with the appropriate sanitizing agents, which might include soap/water or an approved waterless agent. The key to hand hygiene is knowing when and then executing on the proper process of how. When to do hand hygiene is very simple, you must assume that anything you touch with your hands provides a source of contamination. The hands are the transfer vehicle. Examples could include equipment, keyboards, cell phones, all surfaces. Items you should think about are items that are medical devices such as face masks and disposable gloves. All of these can harbor pathogens and with the help of your hands can transfer these pathogens to you, the patient, or other host.
What is environmental hygiene? “Environmental hygiene is maintaining a clean environment by cleaning equipment between use, disinfecting surfaces, and sterilizing medical equipment according to best practices to remove and destroy potential infectious microorganisms.” Essentially, we want to reduce the bioburden or viral load in our surroundings. The processes and tools will be discussed in future writings in this column.
So, let me tie these two interventions together and explain why they are synergistic. In simple terms, if we start with zero bioburden and maintain zero bioburden on surfaces, we reduce the risk that a microorganism will be available to transfer. Is this possible? Maybe not. We know that the hands are the major source of mobility for microorganisms, and with hand hygiene compliance within the healthcare sector averaging less than 38 percent according to the CDC and less than 25 percent when measured electronically, we should be concerned about environmental hygiene and hand hygiene together.
In a recent study completed in a Florida hospital, it was suggested to measure hand hygiene and environmental hygiene compliance simultaneously. Proprietary technology was used to gather data on nursing, physician, and hospital staff (environmental services professionals). This hospital was selected because they had just received the state of Florida award for being “best in practice” for their environmental hygiene. One of the benefits of technology is that they were able to acquire significant data in a short period of time (more than 40,000 opportunities in 10 days). The results, presented to hospital administration, were eye-opening:
• Hand hygiene compliance: Nursing,c33 percent; physicians, 29 percent; staff (EVS), 24 percent
• Environmental hygiene compliance (L&D Unit)
- 23 rooms, 17 occupied
- Rooms require three visits from EVS daily: introduction, cleaning, and revisit QA check
- Data showed of the 17 rooms occupied, that only three visits in three days made by EVS personnel, not daily
- During a 10-minute period that EVS personnel visited eight patient bathrooms, never changing gloves or performing hand hygiene
Nothing was ever heard from administration after this meeting. Key takeaways from this effort were that more accountability is needed in the hand hygiene and environmental hygiene space. Technology can help to validate and reduce time in gathering data. Data puts you in control.
As a final thought, with the help of technology, if we could create more accountability between hand hygiene and environmental hygiene, what might the optimal levels be to move the needle on HAI? Clearly, 100 percent is not achievable, but maybe 60 percent to 70 percent is.
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX - The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
References:
Septimus E, MD, Weinstein RA, Perl TM, Goldmann DA and Yokoe DS. Commentary: Approaches for Preventing Healthcare-Associated Infections: Go Long or Go Wide? Infect Control Hosp Epidemiol. Vol. 35, No. 7, July 2014.
Marschall J, Mermel LA, Fakih M, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35(7): 753-771.
Calfee DP, Salgado CD, Milstone AM, et al. Strategies to prevent methicillin-resistant Staphylococcus aureus transmission and in-fection in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(7):772-796.
Lee BR, Blais FX, Savariau E, Lee R. Poster: An Automated Assessment of Hand Hygiene and EVS Activity.
Hand Hygiene in Surgical Services: Why Not a Digital Approach?
By Robert Lee
This column originally appeared in the March 2022 issue of Healthcare Hygiene magazine.
This article is designed to catalyze some creative thinking around one of the most important areas of a hospital, the perioperative space, which includes pre-op, the operating room suite, post-op, and ancillary/support areas within the operating room (OR).
Here are some questions that need to be asked:
1. Do you measure hand hygiene (HH) compliance in the OR?
2. What methodology do you follow: CDC, WHO, or a hybrid model?
3. Is your methodology measured manually (secret shopper) or automated (technology)?
4. What is your overall HH compliance for your OR?
5. What is your HH compliance for pre-op, post-op, OR suite, and other areas?
6. Does each staff member have a HH compliance scorecard and compliance score?
7. What is included in your HH training and education? How often does it occur? Do you assess
competency?
8. Do you have a simulation center? Do you utilize it for your HH training/education?
9. Do you support LeapFrog and its HH guidelines, becoming part of the total hospital grade?
10. Do you know your LeapFrog quality grade?
These are some questions that occurred after observation and review of HH and environmental services (EVS) compliance data for the perioperative areas:
1. Why is hand HH performance different in pre-op and post-op areas versus main OR suites?
2. Is there less attention, or more lenient guidelines regarding HH in the perioperative areas?
3. Are there different standards for environmental cleaning inside and outside of the OR suite?
4. Why is sterile technique not standard of care both inside and outside the OR suite?
5. How accurate/reliable is your HH compliance and environmental services performance data?
6. Does the Hawthorne Effect contribute to your concern?
7. Have you considered a quality command center approach for your OR?
How do you begin the process? Use a Lean 6 Sigma process to define the current state/workflow. Then, with the help of technology, collect data around this workflow. With consequent accurate, robust, and actionable data, one can then measure, benchmark and report individual, group and unit performance.
How to choose a technology? There are HH technologies available for the perioperative space that can accommodate an open-architecture design and support the WHO 5 Moments methodology. Open architecture designs present a challenge because high-touch surfaces are not contained only in a room and they include stretcher bays, cubicles, incubators, etc., typically found in recovery areas, emergency departments, dialysis units, etc. Most technologies only measure HH compliance at the entry/exit to a closed architecture, typically a room with walls. Can the technology capture data between patient and high-touch areas such as keyboards, workstations, and others as indicated by the WHO 5 Moments recommendation?
As LeapFrog recommends, assess the accuracy of your HH model and method of measurement of HH compliance. Ask your vendor for peer-reviewed, validated clinical studies that define the accuracy of their technology. Additionally, self-validate using observation. Ask yourself the question, “Are we measuring the right things?” With this baseline data, you can objectively assess your HH status and consider improvement with more accurate measurement, enhanced training, and serial measurement to improve your HH performance.
Technology is key to sustainability, easing required personnel and cost of measurement while markedly improving HH observations to accurately assess compliance. When technology is removed, compliance falls below starting levels.
An often-neglected consideration in decreasing hospital infections is the importance of environmental services. Improved hand hygiene performance can be significantly compromised if surfaces and high-touch areas do not receive appropriate decontamination. Decreased bioburden on surfaces and clean hands work synergistically to prevent pathogen transmission.
The Society for Healthcare Epidemiology of America (SHEA) recommends simultaneous interventions to prevent hospital acquired infections. Similar to HH, technology can be a significant asset to monitor and enhance success in environmental decontamination.
With more than 100,000 deaths in acute-care sites and 400,000 deaths in alternate sites, hospital infections remain a serious problem that requires sustained effort to address and improve this problem. The recent pandemic has enhanced the visibility of this issue and emphasized the impact of inadequate adherence to established methods of pathogen transmission. Until we “follow the science” with accurate, robust, real-time data, there will be the continued morbidity and mortality associated with preventable hospital infections. We have the tools and the knowledge, but we have yet to apply them effectively
President John F. Kennedy highlights what our mindset should be: “We choose to go to the moon, not because it is easy, but because it is hard.” Is it time that all operating room leaders commit to “going to the moon”?
Robert Lee, BA, the CEO and founder of MD-Medical Data Quality & Safety Advisors, LLC, is the senior biologist and performance improvement consultant. MD-MDQSA is the home of The IPEX- The Infection Prevention Exchange, a digital collaboration between selected evidence-based solutions that use big data, technology, and AI to reduce risk of HAIs.
The 6 Essential Elements of Hand Hygiene™: A Refined Strategic Framework for Healthcare Organizations
By Paul Alper
This column originally appeared in the November 2021 issue of Healthcare Hygiene magazine.
About a year ago we introduced a strategic framework, The 6 Essential Elements of Hand Hygiene™, to help make hand hygiene second nature for all. Over the past year, we have refined as well as enhanced this approach and are excited to share the results this month.
Every patient, family member, visitor, staff member and volunteer who enters a healthcare facility, especially during this global pandemic, has the right to expect the highest standards for patient safety and quality. One of the most fundamental ways to achieve these standards is to create and value a culture in which hand hygiene is second nature for everyone.
Given that compliance rates, when measured accurately and reliably typically fall below 50 percent, a sound and evidence based strategic framework is essential to drive sustained improvement. Such an approach can provide a checklist of hand hygiene program elements that all work synergistically to ensure optimized hand hygiene behavior.
To that end, we have updated our framework. See the accompanying graphic and feel free to reproduce it for your infection prevention, epidemiology, patient safety and quality leadership team to use as a guide when thinking about your organization’s strategic approach to hand hygiene.
They six essential elements are:
1. Advanced products
2. Reliable delivery systems
3. Point-of-care access
4. Effective learning systems
5. Safety culture
6. Actionable feedback
Here is guidance for how to optimize each element within your organization:
Advanced Products: Select a standardized product formulary that is supported by sound science and developed for high frequency hand hygiene; ensure that staff acceptance is widespread before implementing:
• Alcohol-based hand sanitizers
• Soaps (plain and/or antibacterial)
• Alcohol-based sanitizing wipes
Reliable Delivery Systems: Align placement of product dispensers with CMS, CDC, Joint Commission and WHO guidelines:
• Wall-mounted hand sanitizer dispensers: manual and/or touch-free inside and outside of patient rooms; soap dispensers at all sinks
• Consider lotion dispensers adjacent to sinks to best maintain skin health (lotions should be latex/nitrile plus CHG compatible)
• Touch-free hand sanitizer dispensers on stands for entry ways and other open areas; place easy-to-read signs on top to encourage use
• Personal carry size hand sanitizer bottles
• Tabletop pump bottles with soap and/or sanitizer as appropriate where access to wall mounted dispensers is limited
• Alcohol based sanitizing wipes in packets and canisters
Point-of-Care Access: Position hand hygiene products close to where hand hygiene moments occur:
• Outside and inside patient rooms
• At the bedside
• Throughout the operating room (for acute-care facilities and ambulatory surgery centers)
• At nurses’ stations
• In treatment and examination rooms
• In food service, dining and food-preparation areas
• At information, reception and gift shop desks and counters
• In entryways and lobbies
• Provide personal carry size for when access to wall mounted dispensers is limited or inconvenient
Effective Learning Systems: Provide targeted education and training tools (based on behavioral science, human factors and high reliability organizational design) to make hand hygiene best practices second nature for all:
• Organizational leadership
• Staff and volunteers
• Patients, families and visitors
Ensure tools emphasize proper technique at every moment:
• Before and after touching the patient and/or their surroundings
• Before and after patient care tasks (i.e., changing dressings, inserting new lines etc.)
• Before and after personal activities such as eating, handling a cell phone or device and using the restroom
Deploy facility wide reminders (rotate them regularly to keep the motivation fresh):
• Posters
• Elevator wraps
• Tent cards in dining areas
• Patient and family informational brochures
• In-house TV hand hygiene reminders (think public service announcements)
• Notices on hospital website and/or apps
Safety Culture: Foster a safety culture that embraces:
• Leadership engagement and modeling of expected hand hygiene behaviors at all times
• Psychological safety - everyone feels safe to speak up when hand a hygiene opportunity is missed and greets such reminders with a “thank you!”
• A top-down accountability framework with a unit-based approach for barrier removal, action planning, goal setting and celebrating of gains
Actionable Feedback: Implement best practices for collecting and analyzing data and understand how to pinpoint where improvement is needed:
• Implement reliable performance measurement methods (e.g., electronic hand hygiene compliance monitoring)
• Provide timely, actionable feedback to all
• Maintain and distribute individual hand hygiene report cards to front line staff so they can be aware of and improve personal practice
We’re excited for this update and think it will go a long way in helping healthcare organizations think about hand hygiene in a systematic way that contributes to highly reliable staff performance with sustained gains in compliance. As you think about organizational goals for 2022, consider incorporating the framework as a new patient safety and healthcare quality tool.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the vice president of patient safety innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
October 15 is Global Handwashing Day: How Will Your Organization Celebrate and Accelerate?
By Paul Alper
This column originally appeared in the October 2021 issue of Healthcare Hygiene magazine.
According to its website,1 Global Handwashing Day is “an opportunity to design, test and replicate creative ways to encourage people to wash their hands with soap and water at critical times.” The theme of the day for 2021 is “Our Future is at Hand, Let’s Move Forward Together,” and it calls for collaborative action to reach the goal of universal hand hygiene.
The three aims of Global Handwashing Day are:
1. To create a culture of handwashing with soap in all societies
2. To create awareness of the state of handwashing in each country
3. To inform people about the benefits of washing with soap
In the midst of the COVID-19 pandemic, we certainly have an elevated sense of urgency to institutionalize hand hygiene as a vital element of patient and staff health and safety.
How can your organization celebrate Global Handwashing Day and use it as a driver to accelerate growth of your safety culture? It is an exciting opportunity to take a global concept and make it meaningful to your organization in a way that aligns with your own unique culture. Here is a list of three strategies to consider:
1. Create a video message to your entire community from your CEO or senior C-Suite leader (for example, your vice president of quality) reinforcing how handwashing for 20 seconds with soap and water and proper use of alcohol-based hand rub are core values for the organization. Perhaps have her/him mention that this represents how we all would want ourselves or a loved one cared for; this type of mindfulness can have a profound effect on our own behavior. To learn more about mindfulness, handwashing and overall healthcare quality, take a look at Dr. Sanjay Saint’s TEDx Talk at the University of Michigan titled “Improving Healthcare: Straight from the Heart.”2 Consider depicting your leader taking 20 seconds to demonstrate the practice while talking about it. Post this video and other messages from staff on social media, and consider a press release to your local community emphasizing the importance of the day and your organization’s commitment to ensuring proper hand hygiene is a habit for all in your community of staff, volunteers, patients, family and visitors. Encourage all staff to like and re-post.
2. Set an accelerated goal for hand hygiene compliance across all your organization’s units. Whatever each unit’s current goal is for improvement, add at least 30 percent to it for the final quarter of 2021. For example, if a particular medical unit’s current compliance is 60 percent and the goal for the end of the year is to grow to 70 percent (about a 17 percent increase), make the goal about 30 percent higher than 17 percent or 22 percent -- meaning that the end of the year goal is now about 73 percent. This may not seem like a lot, but it will mean hundreds of thousands more hand hygiene events in a 250-bed facility3 per year and significantly reduce the risk of HAIs.4 If you are still using direct observation for measurement of hand hygiene compliance, consider evaluating electronic monitoring systems as a more accurate and reliable way to measure this vital key patient safety performance indicator.
3. Amp up your approach to facility wide reminders. According to WHO, a multi-modal approach to hand hygiene is essential and one of the key elements is to have a full spectrum of reminders in the workplace.5 This is an excellent opportunity for your marketing department and Infection Control team to collaborate for high creativity. Check out the CDC website6 in addition to the WHO’s site for ideas. These should include:
- Automatic sanitizer dispensers on stands at all entrances with message signs on top
- A hand hygiene reminder screensaver for all staff computers
- WHO 5 Moments posters
- How to properly handwash with soap and water posters
- How to properly use alcohol-based handrub posters
- Patient and family engagement brochure
- Elevator door wraps with creative handwashing messages (a quick web search will bring up a few suppliers)
- Floor decals pointing to hand hygiene dispensers
- In-house TV channel reminders
October 15 is right around the corner and a great trigger event to accelerate your hand hygiene compliance growth trajectory.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Global Handwashing Day | The Global Public-Private Partnership for Handwashing
2. Improving Healthcare: Straight from the Heart - Sanjay Saint's TEDx talk at U-M (umich.edu)
3. Steed C, Kelly JW, Blackhurst DW, Boeker S, Diller T, Alper P. Hospital hand hygiene opportunities: where and when (HOW2)? The HOW2 benchmark study. (2011) Am J Infect Control;39:19-26.
4. Kelly JW, Blackhurst D, McAtee W and Steed C. Electronic Hand Hygiene Monitoring as a Tool for Reducing Health Care Associated Methicillin-Resistant Staphylococcus aureus Infection. (2016) Am J Infect Control. 44(8), 956-957.
5. WHO Guide_to_Implementation.pdf (who.int)
6. Global Handwashing Day | CDC
Is the Juice Worth the Squeeze? Studies That Support Adoption of Electronic Monitoring Systems for Hand Hygiene
By Paul Alper, BA
Editor's note: This column originally appeared in the September 2021 issue of Healthcare Hygiene magazine.
2021 may turn out to be a watershed year for hand hygiene (HH). The emergence of COVID-19 infections has created an ultra-heightened awareness of the importance of hand hygiene. Then there were the 2021 changes in the Leapfrog HH Standard1 requiring up to 200 direct observations per unit per month or the use of a validated electronic monitoring system to achieve the standard on the way to a top Leapfrog Safety Grade and eligibility for Leapfrog’s Top Hospitals Award. These events among other drivers have led many healthcare organizations to evaluate electronic hand hygiene compliance monitoring systems (EHHCMS) to accurately and reliably measure HH compliance.
Naturally, this leads to the key question being asked by C-suite leadership: “Is the juice worth the squeeze?” To answer that question, we can turn to six studies published over the past seven years. By no means is this a meta-analysis of all studies but a sound cross section of the available research. I hope they will help infection preventionists and quality leaders answer that return on investment (ROI) question when seeking funding for an EHHCMS. We all want to improve staff HH performance as we know this will reduce the risk of avoidable harm and healthcare-acquired infections (HAIs), enhance patient safety culture and eliminate incremental costs associated with HAIs. For a comprehensive look at all research in the category of EHHCMS, turn to PubMed2.
1. Srigley, et al. (2014). “Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system” 3
This interesting study demonstrated how the Hawthorne Effect confounds the accuracy of direct observation (DO) as a means to measure HH compliance. A real-time tracking system was used to determine if a healthcare worker was in the line of sight of an observer conducting HH audits. When the healthcare workers could see the observer, they were about three times more likely (90 percent compliant) to perform HH compared to when they could not see them (30 percent compliant) -- a Hawthorne effect of 300 percent. The study was conducted in Toronto where HH rates are reported publicly and this overstatement of HH compliance was reported by the Toronto Star with the headline, “Ontario hospital staff not washing hands as often as reported.”4
One of the investigators, Dr. Michael Gardam, then the Toronto University Health Network’s director of infection prevention and control, is quoted in the Toronto Star as saying, “We’re fooling ourselves. The numbers that we are getting and we are posting publicly are not real, they’re artificial.”
2. Kelly, et al. (2016). Electronic hand hygiene monitoring as a tool for reducing healthcare-associated methicillin-resistant Staphylococcus aureus infection5
Dr. William Kelly and colleagues at the Greenville Memorial Hospital in Greenville, S.C. (now part of the Prisma Health System) used an EHHCMS to demonstrate on a unit-by-unit basis that staff feedback based on data from the system was able to improve HH compliance by more than 25 percent. This was associated with a reduction in MRSA infections of more than 42 percent and a cost avoidance by eliminating 24 MRSA infections of $434,000 per year, or $670 per bed per year. Kelly further pointed out that, “We show that electronic monitoring of HH can lead to clinically important organizational change and, most importantly, improved patient safety.”
3. Bouk, et al. (2016). Use of an Electronic Hand Hygiene Compliance System to Improve Hand Hygiene, Reduce MRSA, and Improve Financial Performance6
Martha Bouk, then head of infection prevention at Riverside Medical Center in Kankakee, Ill. used an EHHMS to also achieve improvement on three metrics: HH compliance (39 percent improvement), reduced MRSA infections (by 50 percent) and improved economics (their ACA financial penalty was eliminated; multiple factors in addition to HH likely contributed to this).
4. Robinson, et al. (2014). Innovative Use of Electronic Hand Hygiene Monitoring to Control a Clostridium Difficile Cluster on a Hematopoietic Stem Cell Transplant Unit.7
Natasha Robinson, then an infection preventionist at the Greenville Memorial Health System in Greenville, S.C., used data from an EHHCMS to provide staff feedback on HH behavior in order to drive higher compliance with the facility’s protocol of washing with soap and water versus using alcohol-based hand sanitizer in the case of clostridium difficile infections (CDI). The result was an increase in HH compliance to 93.9 percent from 77.4 percent (21.3 percent increase) and a drop in the CDI rate from 7.03/10,000 patient days to 2.38/10,000 patient days -- a decline of 66 percent.
5. Banks and Phillips, 2021. Evaluating the effect of automated hand hygiene technology on compliance and C. difficile rates in a long-term acute-care hospital.8
Maureen Banks and Andrew Phillips demonstrated a significant increase in HH compliance from 89.7 percent to 97.1 percent and a reduction in CDI rates from 9.54 to 3.72 infections per 10,000 patient days (61 percent decrease) in a long-term care acute hospital using an EHHCMS.
6. Kelly et al, 2016. Use of Targeted Solutions Tool (TST) and Electronic Monitoring to Improve Hand Hygiene Compliance (2016)9
Kelly and his team demonstrated a 23.5 percent improvement in HH using the combination of an EHHCMS for measurement of HH with DO deployed for coaching and feedback along with barrier and obstacle identification. This model was further embraced by John Boyce in his 2017 paper, Electronic Monitoring in Combination with Direct Observation as a Means to Significantly Improve Hand Hygiene Compliance.10
There are various other studies supporting how an EHHCMS can play a significant role in improving HH compliance, reducing HAIs and their associated costs while positively influencing patient safety culture. 2021 may be the inflection point for this technology’s evolution into best practice standard of care, just as alcohol-based hand rubs did in the past. An EHHCMS can be a powerful and effective addition to the arsenal used to fight HAIs and eliminate risk of avoidable harm.
Disclosure: The author acts as a consultant to Medline Industries, Inc. Medline has a financial relationship with an EHHCMS manufacturer.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Leapfrog Group. (2020, April 13). Leapfrog Hospital Survey. Retrieved from https://www.leapfroggroup.org/sites/default/files/Files/2020HospitalSurvey_20200413_8.1%20%28version%201%29.pdf
2. PubMed (nih.gov)
3. Srigley JA, Furness CD, Baker GR and Gardam M. Quantification of the Hawthorne Effect in Hand Hygiene Compliance Monitoring Using an Electronic Monitoring System: a Retrospective Cohort Study. (2014) BMJ Qual Saf. 23, 974-80.
4. Ontario hospital staff not washing hands as often as reported: study | The Star
5. Kelly JW, Blackhurst D, McAtee W and Steed C. Electronic Hand Hygiene Monitoring as a Tool for Reducing Health Care Associated Methicillin-Resistant Staphylococcus aureus Infection. (2016) Am J Infect Control. 44(8), 956-957.
6. Bouk M, Mutterer M, Schor M, Alper P. (2016) Use of an Electronic Hand Hygiene Compliance System to Improve Hand Hygiene, Reduce MRSA, and Improve Financial Performance. Am J Inf Control 44(6), Supplement, S100-S101, June 02, 2016. DOI:https://doi.org/10.1016/j.ajic.2016.04.135.
7. Robinson N et al (2014) AJIC 42(6), Supplement, S150, June 01, 2014. DOI:https://doi.org/10.1016/j.ajic.2014.03.319
8. Banks, M and Phillips, A.B. (2021) AJIC 49(6): 727-732. doi: 10.1016/j.ajic.2020.10.018
9. Kelly JW, Blackhurst D, Steed C, Boeker S, McAtee W. Use of Targeted Solutions Tool (TST) and Electronic Monitoring to Improve Hand Hygiene Compliance (2016) Accepted as a Poster for presentation at the 2016 SHEA Conference.
10. Boyce JM. Electronic Monitoring in Combination with Direct Observation as a Means to Significantly Improve Hand Hygiene Compliance. (2017) Am J Infect Control. 45(5), 528-535.
Major Historical Milestones in Healthcare Hand Hygiene: A High-Level History of Our Most Important Practice for Infection Prevention
By Paul Alper
Editor's note: This column originally appeared in the August 2021 issue of Healthcare Hygiene magazine.
Reading Jane Brody’s July 12 article Why We Should Keep Washing Our Hands Post Pandemic1 and noting her references to the Jewish and Muslim roots of hand hygiene, it seemed a good idea to reflect on the key healthcare related moments in hand hygiene through the centuries. Here’s a look at 12 of them.
1. The notion that physicians should wash their hands before and after patient contact dates at least as far back as the 1100s when Moses Maimonides wrote, "I dismount my animal, wash my hands, go forth to my patients," and "Never forget to wash your hands after having touched a sick person."2
2. In April of 1847 Ignaz Philipp Semmelweis, a Hungarian physician, was working in Vienna General Hospital’s first obstetrics clinic. This clinic was used for teaching medical students who conducted autopsies as part of their training while a second clinic was only used for the training of midwives who had no contact with cadavers. Semmelweis noted that the mortality rate from puerperal or “childbed” fever was 18.3 percent when the physicians attended obstetrical patients directly after performing autopsies. The rates were much lower in the second clinic.
He proposed the practice of washing hands in a solution of chlorinated lime (calcium hypochlorite) as a way to “remove the putrid smell of infected autopsy tissue.”3 After the hand cleaning practice was put in place in May, the rates dropped 90 percent to 2.2 percent, 1.2 percent and 1.9 percent respectively in June, July and August, comparable to the second clinic.
While today Semmelweis is known as the grandfather of hand hygiene, his research was at odds with the prevailing opinions held by scientists and physicians at the time and his recommendations were rejected by the medical community at large. Some doctors took offense at the suggestion that they should wash their hands and ridiculed Semmelweis who, in 1865, experienced a nervous breakdown, was committed to an asylum and, after a beating by guards, died from an infection.
3. It was common practice until the 1970s for hand soap in healthcare facilities to be available from open-reservoir dispensers refilled from gallon jugs. These dispensers required cleaning between each fill-up that was not likely done with consistency. A start-up company from San Antonio, Texas invented “bag in a box” refills -- closed, sealed, sanitary refills of hand hygiene products that eliminated most risk of contamination. Today, virtually all healthcare facilities use hand hygiene systems based on sealed refills.
4. Alcohol-based handrubs (ABHRs) were introduced into the healthcare market in the 1980s. At first there was reluctance by infection prevention and nursing leaders to abandon soap and water hand washing. Use of ABHRs today is the standard for patient care globally and is routinely used for hand hygiene.
It is easy to see a similarity between Semmelweis and early ABHRs. As the German philosopher Arthur Schopenhauer said, “All truth passes through three stages. First, it is ridiculed. Second, it is violently opposed. Third, it is accepted as being self-evident.”4
5. Then widely used in healthcare facilities but not generally available to consumers, ABHRs or “instant hand sanitizers” as they came to be known, were first widely available to consumers through major retail outlets in 1997. The first in-store display with a tester pump bottle heralded, “Try Me! No Water, No Towel…No Germs!”
6. The 2002 CDC Guideline for Hand Hygiene in Healthcare Care Settings5 proclaimed ABHRs with 60 percent to 95 percent alcohol to be the most effective finally providing guidance on what was already well known and accepted practice, 20 years after their first use.
7. The World Health Organization (WHO) introduced the “5 moments of hand hygiene” in 2009 to reduce the risk of healthcare-associated infections or HAIs. This has become the standard for most of the world today although the U.S. still primarily uses the “in and out” standard.
8. In 2009 the Joint Commission published its monograph on compliance, “Measuring Hand Hygiene Adherence: Overcoming the Challenges.”6 While containing a great deal of information on methods to measure compliance (direct observation, product utilization measurement, patient surveys, video cameras and more) along with their relative strengths and limitations, this monograph fell short of suggesting specific best practice standards of care.
9. John Boyce, in his 2017 paper, “State of the Science Review - Electronic Monitoring in Combination With Direct Observation as a Means to Significantly Improve Hand Hygiene Compliance,”7 presented evidence to support the emerging best practice standard of care: electronic monitoring as the preferred method for measuring hand hygiene compliance with direct observation used for coaching, feedback and obstacle identification. Evidence supporting this approach was published by Kelly, et al. in 2016.8
10. Electronic hand hygiene compliance monitoring systems (EHHCMS) were first introduced in the early 2000s but the first study linking their use to improved hand hygiene behavior, reduced HAIs and positive economic impact was published in 2016 by Kelly, et al.9 The study demonstrated a 25 percent increase in compliance, a 42 percent decrease in MRSA infections and a cost avoidance of $670 per bed per year in the first year.
11. Most earlier-generation EHHCMS were based on RFID (radio frequency identification devices), RF (radio frequency) or required work flow and/or behavior changes. They were expensive and had many shortcomings, a likely reason for low adoption.
2019 saw the first commercial use of near field magnetic induction (NFMI)-based monitoring technology which could measure proximity of healthcare workers to hand hygiene dispensers and patients with centimeter level accuracy (vs. meter+ level accuracy with RFID based systems). This enabled precise measurement of multiple parameters, such as how long a healthcare worker actually washed his/her hands with soap and water, the time between entrance and engagement with a hand sanitizer or washing station, proximity to the patient bed, and more. NFMI technology offers more actionable data than any other technology platform (see my HHM column from January 2021) and appears to be the emerging breakthrough that may lead to much more widespread adoption of EHHCMS.
12. The 2021 revised Leapfrog Group Hand Hygiene Standard10 represents some of the most specific hand hygiene requirements provided by any guideline setting organization. To achieve top Leapfrog Safety Grades and qualify for the coveted Leapfrog Top Hospital Award, healthcare facilities must document up to 200 direct hand hygiene observations per unit per month for all patient care areas or alternatively, use a validated EHHCMS. By meeting the requirements of this comprehensive standard, hospitals can more readily create a safety culture that values accurate and reliable measurement of hand hygiene combined with actionable and timely staff feedback to drive sustainable improvement and reduce the risk of avoidable harm.
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share ideas that might be of interest in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC. Disclosure: The author is as a consultant to Medline Industries, Inc., which has a financial relationship with an EHHCMS manufacturer.
References:
1. Why We Should Keep Washing Our Hands Post Pandemic
2. Hand Hygiene (ecri.org)
3. Ignaz Semmelweis - Wikipedia
4. Arthur Schopenhauer - All truth passes through three...
5. 2002 CDC Guideline for Hand Hygiene
6. Joint Commission Monograph on Adherence
7. Boyce JM. Electronic Monitoring in Combination with Direct Observation as a Means to Significantly Improve Hand Hygiene Compliance. (2017) Am J Infect Control. 45(5), 528-535.
8. Kelly W, Blackhurst D, Steed C, Boeker S and McAtee W. Use of the Targeted Solutions Tool and Electronic Monitoring to Improve Hand Hygiene Compliance. Paper presented at the 2016 SHEA annual meeting.
9. Kelly JW, Blackhurst D, McAtee W and Steed C. Electronic Hand Hygiene Monitoring as a Tool for Reducing Health Care Associated Methicillin-Resistant Staphylococcus aureus Infection. (2016) Am J Infect Control. 44(8), 956-957.
10. Leapfrog Safety Grade 2021 Updates
Creating A Safety Culture: A Checklist for Hand Hygiene-Centric Success
By Paul Alper
Editor's note: This column originally appeared in the July 2021 issue of Healthcare Hygiene magazine.
Everyone who enters a healthcare facility, especially during this global pandemic, has the right to expect the highest standards of care that ensure optimized patient safety and quality. A fundamental way to achieve high levels of each is to create and continuously enhance a culture in which hand hygiene is second nature for every staff member and volunteer.
Given that hand hygiene compliance rates when measured accurately typically fall below 50 percent, an evidence-based strategic framework is essential, providing a list of hand hygiene program elements that work synergistically to ensure optimized hand hygiene behavior.
To that end, we recently created a strategic framework: “The 6 Essential Elements of Hand Hygiene,”1 which are:
• Advanced products
• Reliable delivery systems
• Point-of-care access
• Effective learning systems
• Safety culture
• Actionable feedback
In this month’s column I want to help you grow your safety culture as it relates to hand hygiene.
When it comes to building a culture of safety, one of the most important pre-conditions for success is the concept of “psychological safety”. This was first defined in 1965 as an “atmosphere where one can take chances without fear and with sufficient protection.”2
What this means practically is that healthcare workers on a team share a common value in the importance of patient and staff safety and further have a common belief that the team will not embarrass, punish, reject, isolate or otherwise seek retribution when anyone speaks up in a professional manner on any matter regarding risk of harm -- especially when interacting with one’s supervisor or a more senior ranking staff member.
Therefore, to help create positive change in today’s healthcare organization, here is a seven-step checklist to consider:
1. Empower individual units to take ownership for hand hygiene improvement and acknowledge their progress as they hit monthly/quarterly compliance growth targets.
2. Structure unit leader’s annual performance appraisals and bonuses to reward meeting your hand hygiene improvement goals.
3. Establish and implement a cycle of routinely identifying unit based obstacles and barriers to hand hygiene performance and then put in place action plans with the goal of eliminating them. Encourage input and participation at the front line staff level. Incidentally, this is probably one of the best possible uses of direct observation -- not as a measurement tool but as one focused on coaching and real-time feedback.
4. Measure hand hygiene compliance and give feedback on performance to staff on a consistent frequency (for example, weekly) using a non-biased and validated compliance monitoring system. This might be an electronic hand hygiene compliance monitoring system or direct observation using well-trained observers who are properly validated for inter-rater reliability.
5. Celebrate when monthly/quarterly goals are achieved and collaboratively identify what to do differently when they are not. When your goals are met, set a new, higher target.
6. Make psychological safety “the way we work” – anyone can speak up in a professional and appropriate fashion when there is/was risk of doing harm (such as not doing proper hand hygiene when it is indicated) without fear of embarrassment, rejection, isolation, retribution or other negative consequences.
7. Ensure that your organization’s senior leaders consistently model proper hand hygiene behavior and are authentically engaged in your hand hygiene improvement efforts.
Only when your organization is doing these seven steps robustly with a high degree of rigor and shared accountability, can hand hygiene ever be optimized. One thing is certain, as stated in “Still Not Safe” by Wears and Sutcliffe (a great read by the way) -- “unless we in patient safety change, nothing will change in patient safety.”3
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share ideas that might be of interest in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the vice president of patient safety innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Alper P. The Six Essential Elements of Hand Hygiene. Medline Industries. 2021.
2. Schein EH, Bennis WG. Personal and Organizational Change Through Group Methods: The Laboratory Approach. New York, NY: Wiley; 1965.
3. Wears RL, Sutcliffe KM. Still Not Safe. Oxford University Press. 2020.
Conducting an Objective Hand Hygiene Product Evaluation
By Paul Alper
Editor's note: This column originally appeared in the June 2021 issue of Healthcare Hygiene magazine.
A healthcare organization typically only looks at changing out hand hygiene products -- soaps, sanitizers and dispensers concurrent with their current contract, usually three to five years in duration. Many organizations make no changes for even longer periods. There are several drivers that might influence an organization’s decision to change hand hygiene products examples of which follow in this table [see the June 2021 issue of Healthcare Hygiene magazine for this table]
Here is a checklist for how to best evaluate and decide on products to which your organization might transition. Note that we are not going to discuss any predecessor request for proposal (RFP) process, only how to best evaluate which product(s) might be best suited to your staff and organization once you have decided upon final candidates. Consider using a survey tool to collect data and analyze results or any internal software or system you may already have in place to poll staff satisfaction.
Establish a Set of Evaluators
Consider a cohort of at least 10 to 15 evaluators, representing nursing and IP staff, EVS personnel, physicians, ancillary healthcare workers, food service workers, employee health, volunteers and patient advisory council members if they are present in your organization. The larger your organization, the larger the respondent cohort. Consult with any bio-statistician(s) that may be on staff for an appropriate cohort size for your organization.
Establish a Baseline
The following questions should be used to establish a baseline of satisfaction with your evaluators for both your current hand soap and hand sanitizer using a 1-5 (5 being the highest) satisfaction scale:
• In general, my level of satisfaction with the current (indicate soap or sanitizer) is________
o Explain why you gave it this rating (please include any skin issues you may experience such as drying or redness [refer any chronic issues to occupational health]):_________________________________________________________________
• Please rate your satisfaction with our current (indicate soap or sanitizer) on the following criteria:
o Feel on skin during use____
o Fragrance/odor____
o Lather (for soaps only)____
o Foam (for foaming products only)____
o Skin feeling after use ____
o Please tell us any comments you think important on any of the above_____________
• In your opinion, should we consider a change in products(s)? YES/NO
o If YES, please explain why? _____________________________________________________________________________
Evaluating Potential New Products
The goal should be to establish product acceptance rather than product superiority with any new product(s) being considered. This is because you may want to change products for economic reasons and don’t want to have the bar set that high. If possible, products should be blinded (no brand identity) to staff participating in the evaluation. Only the data analyst would know which product is which.
The following instructions should be given for use of the products:
1. For the soaps, use each product in the following manner: wet hands under running water, apply the soap topically and lather into hands, rub for at least 20 seconds, and then rinse hands under running water. Dry with a towel. In between sampling each product, either wait at least 30 minutes or wash and dry your hands.
2. For the sanitizers, use each product in the following manner: apply topically to your hands and rub into your hands until the product is completely absorbed. In between sampling each product, either wait at least 30 minutes or wash and dry your hands.
Evaluation
Use this questionnaire, adapted for your culture using a scale of 1-5 with 5 being the highest satisfaction.
• In general, my level of satisfaction with the Product (indicate Soap A or Sanitizer B etc.) is________
o Please explain why you gave it this rating (please include any skin issues you may experience such as drying or redness):_________________________________________________________________
• Please rate your satisfaction with Product (indicate Soap A or Sanitizer B etc.) on the following criteria:
o Feel on skin during use____
o Fragrance/odor____
o Lather (for soaps only)____
o Foam (for foaming products only)____
o Skin feeling after use ____
o Please tell us any comments you think important on any of the above_____________
• In your opinion, is this product acceptable to you for adoption by our facility? YES/NO
o If NO, please explain why? _____________________________________________________________________________
If dispenser dissatisfaction is the main driver for potential change, adapt questions 1 and 3 from the Baseline and Evaluation questionnaires to determine staff opinion of the dispensers.
Tally the results and as long as you have a majority finding the product acceptable, weigh the pros and cons for conversion. Consider a two- to four- unit pilot before scaling to the entire facility using the same/similar questionnaires for baseline and actual evaluations. Changing soaps/sanitizers and dispensers can be a major decision affecting all staff within a facility - but as long as evaluations are inclusive and un-biased, you can make great decisions for the long term.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
Hand Hygiene Best Practices for Dental Offices in the COVID-19 Pandemic
By Paul Alper
This column originally appeared in the May 2021 issue of Healthcare Hygiene magazine. Please refer to that issue for associated charts and tables.
Over the past year we have provided up-to-date best practices for hand hygiene during the COVID-19 pandemic for acute-cute and long-term care settings. This month we will address an important setting, the professional dental practice, where persistent vigilance is also essential to ensure patients’ and dental professionals’ safety.
Proper hand hygiene is an effective way to help prevent the spread of infection between patients and dental professionals during both routine procedures and more invasive oral surgeries. The best way to help ensure that your team knows and follows proper hand hygiene practices is to provide effective ongoing education and training.
What does the Centers for Disease Control and Prevention (CDC), American Dental Association (ADA) and Occupational Safety and Health Administration (OSHA) say about Hand Hygiene in the Context of COVID-19 in Dental Offices? Table 1 below explains it all in detail.
Distilling the guidance down to a holistic hand hygiene approach for any dental practice, here is a practical guide for when to perform hand hygiene within a dental practice. We have included a table identifying each distinct area within a practice and what the optimized hand hygiene solution might look like in terms of product and dispensing system. Each is based on the latest CDC, ADA and OSHA guidance:
All staff should be trained on the WHO 5 moments for hand hygiene as well as how to both properly sanitize hands with an alcohol-based hand sanitizer and wash with soap and water. While the WHO 5 moments for hand hygiene are most commonly cited in the context of the hospital or post-acute setting, they are equally relevant to dental practices.
Dental professionals should perform hand hygiene:
• Before and after treating a patient
• After putting on, touching, or removing Personal Protective Equipment (PPE) or face coverings
• After handling personal devices such as cell phone, tablet, or computer keyboards
• Before and after personal tasks such as before eating and after using the restroom; taking breaks
• After touching surfaces or instruments in treatment areas with bare hands
• Anytime hands are visibly soiled or may have come into contact with blood or body fluids
• Before and after oral surgery procedures
• Before leaving the practice post shift
Plain or Antibacterial Soap? What Percentage of Ethanol?
Except for pre-surgery hand hygiene, it is totally acceptable to use a plain lotion or foaming soap. Alternatively, an antibacterial lotion or foaming soap with benzalkonium chloride (BZK) or similar active may be selected. When selecting hand sanitizers and rubs for non-pre-surgery use, anything over 60 percent ethanol is acceptable although many providers are migrating to products with 70 percent and even 80 percent ethanol for the additional efficacy they can provide.
Hand hygiene consistency, diligence and vigilance are “musts” for any dental practice in today’s pandemic environment and adherence to the above recommendations should provide significantly reduced risk for the spread of infections.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Hand Hygiene Recommendations. Guidance for Healthcare providers about hand hygiene and COVID-19. Centers for Disease Control and Prevention. Updated May 17, 2020.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html#:~:text=Hand%20hygiene%20is%20an%20important,and%20infections%20in%20healthcare%20settings.
2. Centers for Disease Control and Prevention. Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept. of Health and Human Services; October 2016.
https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf
3. Recommendations from the Guidelines for Infection Control in Dental Health-Care settings – 2003.
https://www.cdc.gov/oralhealth/infectioncontrol/pdf/recommendations-excerpt.pdf
4. Guidance for Dental Settings. Interim Infection Prevention and Control Guidance for Dental Settings During the Coronavirus Disease 2019 (COVID-19) Pandemic. Centers for Disease Control and Prevention. Updated December 4, 2020.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
5. Hand Hygiene for the Dental Team. American Dental Association. Center for Professional Success.™
https://success.ada.org/en/practice-management/dental-practice-success/dps-spring-2020/hand-hygiene-for-the-dental-team
6. Dentistry workers and employers. Occupational Safety and Health Administration.
https://www.osha.gov/coronavirus/control-prevention/dentistry
7. Protecting Workers: Guidance on Mitigating and Preventing the spread of COVID-19 in the Workplace. Occupational Safety and Health Administration.
https://www.osha.gov/coronavirus/safework
8. OSHA Compliance Dental Professional. Institute for Dental Compliance and Risk Management.
Dental OSHA Training – OSHA Compliance for the Dental Professional
9. Medical and Dental Offices. A Guide to Compliance with OSHA Standards.
https://www.osha.gov/sites/default/files/publications/osha3187.pdf
10. Dentistry. Occupational Safety and Health Administration.
https://www.osha.gov/dentistry
11. Interim Enforcement Plan for Coronavirus Disease 2019 (COVID-19).
https://www.osha.gov/memos/2020-04-13/interim-enforcement-response-plan-coronavirus-disease-2019-covid-19
Making the Business Case for Infection Control Technology
By Paul Alper
This column originally appeared in the April 2021 issue of Healthcare Hygiene magazine.
When I lecture infection preventionists on the latest approaches to optimizing hand hygiene performance, I typically open with a question, “Are you responsible for driving hand hygiene compliance improvement?” Usually everyone answers “yes.” My follow-up gets the opposite response: “Do you have a discretionary budget and authority to spend it on a vetted technology, product or service you feel will help drive sustainable improvement in compliance?” Usually no one answers to the affirmative. This leads me to conclude that improvements in hand hygiene compliance requires very sound arguments to convince leadership to allocate precious organizational resources. Here is a strategic framework to help you make the case for technology adoption and influence organizational leadership to buy in:
A. Be sure you can align your request with organizational priorities, keeping your eye on the best interests of the organization’s community-at-large
• Is patient safety, high reliability, getting to zero harm a stated organizational goal? If yes, then align your request with how adoption will support and drive success with these organizational goals.
• How will adoption address obstacles to the ideal future state? Create a vision for achieving the ideal state as the end game that adoption will help realize.
B. Identify all clinical and economic key influencers/decision making stakeholders and know what is important to them.
• Target each with simple messages that define how their interests will be served.
• Listen to any barriers/obstacles they raise and collaborate to remove or mitigate them to acceptable levels.
C. It’s all about the math
• Get the evidence and math right. The following three-step process will help you do that.
1. Know your baseline: what are you doing today and what does it really cost?
Assuming you are doing direct observation (DO), you can calculate the true cost of DO based on the evidence based calculation as published in my March column. Using the 383-bed teaching hospital as an example, the total cost for DO for inpatient units was $117,914 per year.
2. Calculate the cost for the technology. Let’s say the one you’re looking at costs $300 per bed per year on a subscription basis; that comes out to $114,900 per year (plug in whatever number applies to the technology you are considering; include all costs including any costs for badges, maintenance, repair and battery replacement, if any).
3. Make a sound assumption for what the impact on HAIs will be and calculate the ROI. Let’s look at two examples where electronic hand hygiene systems were implemented and had a positive impact on MRSA and C. diff rates, as these are infections known to be easily transmitted by the hands. Kelly, et al .2 showed a 43 percent reduction in MRSA infections and estimated each avoided infection saved the hospital $18,083. In this instance, the savings amounted to $434,000, or $670 per bed per year. Robinson, et al. 3 showed a 66 percent reduction in the rate of C. diff but did not do any economic impact analysis. Zhang, et al. 4 estimate the incremental cost of a C. diff infection to be $25,000.
Eliminating just one MRSA and one C. diff infection could save over $43,000 per year. Eliminating two of each would save over $86,000. Using the data from Kelly and Robinson as conservative baselines, how many MRSA and C. diff infections could you avoid by implementing an electronic hand hygiene compliance system (or any innovative technology for which you wish to make the business case)? Here is an example assuming just two MRSA and one C. diff infections are eliminated (cost avoidance = $61,166 per year).
Calculate the ROI dollars. For this example (set up in EXCEL for ease of use):
a) Technology Cost Plug in annual cost of your contemplated technology here = $114,900
b) Cost of DO saved Plug in current total annual cost of Direct Observation here = $117,914
c) HAI costs avoided Plug in your estimated annual HAI impact savings here = $66,166
ROI (savings per year)= a-b-c Calculate a-b-c to calculate your ROI (savings per year here) which should be a negative number as it represents savings = ($69,180)
Then, be sure to add in the additional operational benefits, if any, of the technology you are advocating for, such as provides accurate data; enables feedback to frontline staff; capable of real-time reminders at the point of care to prevent possible missed hand hygiene opportunities; supports our high reliability organizational goals; supports an enriched patient safety culture, etc.
No matter what technology or solution you are considering, this method for influencing leadership with a well document ed business case supported by the science, will help you strategically frame your request in a sound, evidence-led manner consistent with a value-driven, high-reliability organization.
Paul Alper, BA, is the vice president of patient safety innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Srigley JA, et al. Quantification of the Hawthorne Effect in Hand Hygiene Compliance Monitoring Using an Electronic Monitoring System: a Retrospective Cohort Study. (2014) BMJ Qual Saf. 23, 974-80.
2. Kelly JW, et al. Electronic Hand Hygiene Monitoring as a Tool for Reducing Health Care Associated Methicillin-Resistant Staphylococcus aureus Infection. (2016) Am J Infect Control. 44(8), 956-957.
3. Robinson N, et al. Innovative Use of Electronic Hand Hygiene Monitoring to Control a Clostridium Difficile Cluster on a Hematopoietic Stem Cell Transplant Unit. (2014) Am J Infect Control. S29-S166, S150.
4. Zhang D, et al. Attributable Healthcare Resource Utilization and Costs for Patients with Primary and Recurrent Clostridium difficile Infection in the United States. Clin Infect Dis 2018.
Calculating the True Cost of 200 Direct Observations Per Unit Per Month in 7 Steps
By Paul Alper
Editor's note: This column originally appeared in the March 2021 issue of Healthcare Hygiene magazine.
With the Leapfrog hand hygiene standard requiring 200 direct observations per unit per month for in-patient units; up to 200 observations per month for emergency department units based on the number of visits per month and up to 200 observations per unit per month for areas where the monthly occupancy rate fluctuates1 (e.g., PACU, outpatient units), many healthcare organizations are trying to calculate real the costs of direct observation as required to meet the standard.
Fortunately, there an evidence-based calculation for the true cost of those 2,400 visual observations per unit per year based on the HOW2 (Hand Hygiene Opportunities Where and When) Benchmark Study,1 published in AJIC in 2011.
The purpose of the study was, for the first time, to determine hand hygiene opportunities (HHOs) in 2 types of hospitals - teaching and community within three clinical areas: medical-surgical units, intensive care units and emergency departments. The study used trained direct observers, controlled for inter-rater reliability, to calculate the actual number of HHOs per patient day.
This column will focus on calculating the costs for in-patient areas. Because care in outpatient areas and emergency department are so variable, we will use a conservative plus up factor estimate of 15 percent for these areas, but the data is there to do exact calculations based on your organizations actual statistics to gain that level of precision, should you wish to do so.
The study determined the number of HHOs in Adult Medical Units and ICUs (Table 1). Note that the study looked for WHO 5 Moment total HHOs but also broke the data down by moment, so we can calculate that “In and Out” HHOs in and Adult Medical unit equals 48.9 percent of the total.
From here, we just need to know the true, fully loaded cost for the staff doing the observations along with the total number of units and average bed counts for each and we can then calculate the cost per year of meeting the 200 visual observations per unit per month.
The following calculations are based on two real hospitals, a teaching hospital and a community hospital. The bed counts and labor costs were provided by senior nursing leadership. The calculations were done based on the “in and out” standard for measuring hand hygiene, as most hospitals are unable to conduct accurate visual observations for the WHO 5 Moments.
The Teaching Hospital
There are 328 medical unit beds in 19 units with an average of 17.3 beds per medical unit. There are also 54 ICU beds in six units with an average of nine beds per ICU. Their average cost for their nursing staff direct observers is $42 per hour with benefits. So, here is the calculation which you can easily re-create for your organization:
Medical Units
Step 1: Divide the HHOs per patient day of 35 by 24 to get the HHOs per patient hour, in this case = 1.5
Step 2: Multiply that by the average number of beds per medical unit, in this case 17.3, to get the HHOs per unit hour = 25.2.
Step 3: Divide that into 200 (the target direct observations per unit per month) to get the number of hours needed for 200 observations per unit per month = 7.9.
Step 4: Multiply that by 12 to get the total number of hours per year needed to achieve the standard for just the observations alone = 95.1; then multiply this by a + factor you think is reasonable for the administrative time to plug the calculations into a spread sheet, create reports, review and distribute them etc., we will use 25 percent for administrative and non-observational time required = 118.9 hours needed per medical unit per year to achieve the Leapfrog standard.
Step 5: Multiply this number of hours per year by the total number of medical units (19) by the rate per hour ($42) = $94,856.57 per year for the total cost of 200 direct observations per unit per month.
Step 6: Repeat these steps for the ICUs, and you find that the total cost per year to meet the standard = $23,057.60.
Step 7: Total these two amounts and add a plus up factor of 15% for outpatient areas, other patient care areas and EDs and you get a grand total of $135,601.30 per year.
The Community Hospital
Applying the same seven steps using the HHOs for the community hospital you will find that the total cost is $182,044.81 (due to fewer number of opportunities per hour, it takes much more time to capture the requisite number of observations thus the higher cost).
Knowing the real cost of deploying professional, properly trained staff to meet the standard will help you accurately compare these costs to other options such as e-monitoring to assess which will provide the most robust, accurate, timely and actionable data for your organization.
Disclosure: Medline is a 2021 member of the Leapfrog Partners Advisory Committee and has a collaborative relationship with a company that offers electronic hand hygiene monitoring services.
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share ideas that might be of interest in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn. Also, please write to me for any help in creating your own calculator in Excel.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the vice president of patient safety innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Leapfrog Group. (2020, April 13). Leapfrog Hospital Survey. Retrieved from https://www.leapfroggroup.org/sites/default/files/Files/2020HospitalSurvey_20200413_8.1%20%28version%201%29.pdf
2. Steed C, Kelly JW, Blackhurst DW, Boeker S, Diller T, Alper P. Hospital hand hygiene opportunities: where and when (HOW2)? The HOW2 benchmark study. (2011) Am J Infect Control;39:19-26.
Direct Observation vs. Electronic Monitoring: The Essential Evidence and Facts to Consider
By Paul Alper
Editor's note: This column originally appeared in the February 2021 issue of Healthcare Hygiene magazine.
Many organizations including the Joint Commission, APIC, SHEA and The Leapfrog Group have guidelines and recommendations for hand hygiene compliance in acute care hospitals. Among them, The Leapfrog Group has established a leadership position by developing best practices for optimizing hospital hand hygiene (HH) performance and incorporating them into their evolving Hand Hygiene Standard. This Standard has five domains of performance that hospitals must meet:
• Training and Education
• Infrastructure
• Monitoring
• Feedback
• Culture
This column will address and focus on compliance monitoring, but to be clear, getting hand hygiene right to improve patient safety and drive the best possible outcomes requires meeting the performance and practice criteria for all 5 domains. While we will only consider in-patient units in acute care hospitals, similar principles and approaches as described in this column would apply to emergency departments and out-patient units.
Many infection preventionists and C-suite hospital leaders are facing the choice of the two options for measuring compliance -- direct observation or a validated electronic compliance monitoring system that can capture both hand hygiene opportunities (HHOs) as well as hand hygiene events (HHEs). Regardless of how they measure compliance, the evidence suggests1,2, that a hospital use direct observation for coaching and intervention, with the goal of identifying and removing barriers and obstacles to hand hygiene.
But when it comes to accurate, reliable and cost-effective measurement, which makes more sense? Studies have shown that the combination of electronic monitoring for measurement with direct observation for coaching and intervention can lead to significant improvement in hand hygiene compliance.3
There are 5 essential factors to consider.
1. Direct Observation, The Hawthorne Effect and Data Quality: It is well established that staff behave differently when being observed leading to overstatement of hand hygiene compliance by up to 300 percent.4 This significant lack of accuracy and reliability can easily lead to staff and leadership complacency, putting patients at risk of avoidable harm. A validated electronic monitoring system can be capable of capturing virtually all hand hygiene opportunities and events, eliminating the risk of the Hawthorne Effect and generating data truly representative of all facility wide hand hygiene behavior, 24/7.
2. Observer Bias: For hospitals using direct observation, they need to have a system for initial and recurrent training and validation of hand hygiene compliance observers which is essential to achieve inter-rater reliability. However, observers have been shown to be quite biased5 and controlling for inter-rater reliability takes time, effort and practice. A validated electronic monitoring system eliminates the risk of bias and also precludes the need for the validation of the direct observers as they will only need to be deployed for coaching and intervention.
3. Timeliness of Feedback. Typically, a hospital does not provide feedback from direct observations for up to 30 days. Feedback, to be truly actionable, should be timelier. There are electronic monitoring systems that enable feedback on hand hygiene compliance rates in less than 24 hours, some with real time alerts to prevent potentially missed events. Data from an electronic monitoring system combined with appropriate front line staff feedback has been shown to drive higher compliance, reduce infections, eliminate significant costs due to extended length of stay and additional patient care and have a positive impact on safety culture.6
4. Sufficiency of Sample Size: When direct observation is the only available method for monitoring hand hygiene compliance, many hospitals are setting a target of 200 direct observations or 1.7 percent of total hand hygiene opportunities per unit per month. There is, however, potentially a much larger and richer dataset to mine when one considers the estimated number of hand HHOs based on the HOW2 Study.7
There are electronic monitoring systems available today that are capable of capturing virtually every HHO as well as HHEs, thus providing much more robust and actionable data. A 15-unit, 250 bed academic hospital would likely have an estimated 8.3 million total in-patient HHOs/year (assuming 100 percent occupancy; 200 medical unit beds and 50 ICU beds) based on the HOW2 Study. This could be a great source of rich insights for front line staff feedback
5. The Economics of Direct Observation: The cost of meeting the 200 direct observations per unit per month target for a 250-bed academic medical center with 10 medical units (20 beds each) and 5 ICUs (10 beds each) for in-patient monitoring alone could be over $76,000/year assuming a total cost, with benefits, of $55/hour for trained direct observers. This annual number would be significantly higher for a community hospital. There are electronic monitoring systems on the market with similar or lower costs per year that could provide much more timely, in-depth and actionable data.
When considering these factors and the goal of achieving 200 observations per unit per month, it becomes clear that, while either method can be used, direct observation has significant limitations while automated systems for monitoring hand hygiene compliance should be seriously considered for their robust clinical as well as economic benefits.
An important note, when making any decisions concerning achieving the Leapfrog Hand Hygiene Standard, hospitals should refer to the Leapfrog full-text version for complete information and decision support found here: Leapfrog Group 2020 Hospital Survey.8.
Disclosure: Medline is a 2021 member of the Leapfrog Partners Advisory Committee and has a collaborative relationship with a company that offers electronic hand hygiene monitoring services.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Kelly W, Blackhurst D, Steed C, Boeker S and McAtee W. Use of the Targeted Solutions Tool and Electronic Monitoring to Improve Hand Hygiene Compliance. Paper presented at the 2016 SHEA annual meeting.
2. Son, C., Chuck, T., Childers, T., Usiak, S., Dowling, M., Andiel, C., Sepkowitz, K. (2011) Practically speaking: Rethinking hand hygiene improvement programs in health care settings. American Journal of Infection Control, 39(9), 716–724. doi:10.1016/j.ajic.2010.12.008
3. Boyce JM. Electronic Monitoring in Combination with Direct Observation as a Means to Significantly Improve Hand Hygiene Compliance. (2017) Am J Infect Control. 45(5), 528-535.
4. Srigley JA, Furness CD, Baker GR and Gardam M. Quantification of the Hawthorne Effect in Hand Hygiene Compliance Monitoring Using an Electronic Monitoring System: a Retrospective Cohort Study. (2014) BMJ Qual Saf. 23, 974-80.
5. Dhar, et al. Observer bias in hand hygiene compliance reporting. (2010) Infec Contr Hosp Epidemiol; 31(8):869-70
6. Kelly JW, Blackhurst D, McAtee W and Steed C. Electronic Hand Hygiene Monitoring as a Tool for Reducing Health Care Associated Methicillin-Resistant Staphylococcus aureus Infection. (2016) Am J Infect Control. 44(8), 956-957.
7. Steed C, Kelly JW, Blackhurst DW, Boeker S, Diller T, Alper P. Hospital hand hygiene opportunities: where and when (HOW2)? The HOW2 benchmark study. (2011) Am J Infect Control;39:19-26.
8. Leapfrog Group. (2020, April 13). Leapfrog Hospital Survey. Retrieved from https://www.leapfroggroup.org/sites/default/files/Files/2020HospitalSurvey_20200413_8.1%20%28version%201%29.pdf
Electronic Monitoring Systems: A Strategic Approach to Next-Generation System Selection
By Paul Alper
This column originally appeared in the January 2021 issue of Healthcare Hygiene magazine.
In 2009, the Joint Commission published its Monograph on Hand Hygiene Adherence (Measuring Hand Hygiene Adherence: Overcoming the Challenges) which recommended that measurement of hand hygiene behavior and staff feedback was essential to reduce the risk of healthcare-associated infections (HAIs). However, at the time as stated by the publication, the only ways available to measure hand hygiene were “observation, product measurement and surveys.”
We know now that these are very poor approaches when it comes to accurate and reliable measurement. Visual observation is biased and typically overstates compliance by up to 300 percent (Srigley, et al. 2014, among other studies); product measurement lacks an accurate denominator (how much product should have been used? It’s impossible to know with any accuracy) and surveys are just biased opinions.
We have come a long way since then. At the time of the publication of the monograph, electronic monitoring systems were just coming into being and hitting the market. The systems were based on a variety of technologies and none were ideal:
• RFID (radio frequency identification devices) integrated with RTLS infrastructure (real time locating system) can have a significant up front expense and are subject to signal attenuation and thus inaccurate capture of hand hygiene events
• Alcohol-detection based systems work okay for sanitizer but what about hand hygiene events accomplished with soap and water? Further, they typically require physically holding one’s hands close the badge which is a potential human factors/workflow concern
• Group only systems -- we know now that individual healthcare worker data & feedback is essential to driving sustainable behavior change
• A variety of other individual monitoring systems that only provided in and out data vs. The WHO 5 Moments standard
But as we enter 2021, the next generation of e-monitoring is emerging -- systems that are based on near-field magnetic induction (NFMI). While most of us have never heard of NFMI (I didn’t until a few months ago), many of us use it in our everyday life, as it’s the same technology that enables keyless starting of one’s car. Many of today’s “key” fobs use NFMI to detect whether you are inside or outside of the car and this centimeter level proximity sensitivity enables keyless starting of your car as long as you are in a certain zone.
As an inventor of one of the early-generation monitoring systems with four issued patents, I was thoroughly impressed when I “got under the hood” of this new generation of systems and learned how capable they were of accurate and reliable measurement of either standard of compliance -- both “in and out” or the WHO 5 Moments for hand hygiene. A real advance in systems design and thinking. When you factor in the economics and the fact that NFMI can cost anywhere from 50 percent to 80 percent less than RFID/RTLS, alcohol detection and group only systems, you have a real game-changer.
Here are the five things you need to know about NFMI:
1. NFMI has centimeter vs. meter* level accuracy of RFID technology – enables proximity to bed/patient zone monitoring accuracy (supports the WHO 5 Moments standard).
2. NFMI signals pass through the human body where RFID signals are absorbed by the body potentially resulting in understated compliance rates -- enables data accuracy in which front line staff will have confidence.
3. NFMI is ultra-low power enabling devices with multi-year battery life -- routine battery replacement is not needed.
4. NFMI allows for the use of AI software integration – that makes the system “smart” in determining accurate compliance in the nuanced world of hand hygiene in a healthcare setting. Also helps eliminate the risk of “data denial” by staff
5. NFMI is low-cost technology with light infrastructure requirements -- results in the most affordable, scalable and highest ROI hand hygiene monitoring technology available globally.
*Accuracy limit of most RFID systems
Essential Criteria/Considerations for an E Monitoring System: A Checklist for 2021
When evaluating electronic systems for measuring hand hygiene compliance in your organization, here is a check list of essential criteria and considerations:
1. Technology Platform: The emerging state of the art technology is NFMI. But when considering other technology platforms, they should meet the criteria 2-9 that you deem essential for your facility. Of course, there are always trade-offs to be considered when it comes to must have features and your budget. So every facility has to decide for itself what works best within its safety culture and financial situation to find the best blend of clinical features for their individual budget.
2. Performance Standard: The system should be capable of measuring both standards of hand hygiene performance -- either the WHO 5 Moments or “In and Out”
3. Reporting Level: Should be able to provide both group and individual level reporting
4. Communications Network Facility Support Requirements: The system should be a totally stand-alone infrastructure – requiring no integration with hospital Wi-Fi, IT network etc.
5. Point of Care Reminders: The system should have the ability to remind/intervene at the point of care and “rescue” potential missed opportunities.
6. Contact Tracing: The system should be capable of contact tracing reporting.
7. C. diff Room Reporting: The system should provide the ability to see both soap and sanitizer event trending so that real time feedback can be given to staff as to whether they are complying with the typical C. diff protocol - the switch to soap and water hand hygiene from alcohol-based hand sanitizer which does not kill C. diff spores.
8. Hand Hygiene Dispenser Requirements: The system should be soap/sanitizer-brand agnostic and work with any brand of hand hygiene products.
9. Economic Model: You will have to choose from a system with an up-front capital expense and on-going service costs or a subscription fee based agreement. When selecting a subscription fee based model, which can be the most cost effective in the long run, be sure the subscription fee covers all costs including, but not limited to: hardware infrastructure and installation, badges and badge administration, unlimited data access (option for either log-on or auto email push reports), staff training, maintenance and repair, battery refresh/replacement, 24/7 system integrity monitoring and on-going; unlimited access to help desk support.
It is so exciting to see new, disruptive technology offerings emerging. I recently spoke to an industry colleague and friend, Michael Mutterer (vice president of patient care and chief nursing officer at Silver Cross Hospital in New Lenox, Ill.) about what he was doing in terms of monitoring of hand hygiene compliance. Here is what he said: “We are really excited to be an early adopter of an electronic hand hygiene monitoring system based on near field magnetic induction or NFMI. It’s the only technology that lets us monitor either the WHO 5 Moments OR in and out standards of care with accuracy that is far greater than RFID or RF based technologies that are quite frankly, now outdated. Lastly, it is the most affordable technology we have seen to date and that made it easy to cost justify to our financial leadership.”
The time has come for hospital leaders to adopt what will likely be the best practice approach to optimizing hand hygiene: use e-monitoring technology for measurement and direct observation for coaching, feedback and obstacle elimination.
Hope this helps, and Happy New Year!
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share ideas that might be of interest in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
A New Strategic Framework for Healthcare Organizations: Making Hand Hygiene Second Nature
By Paul Alper
Editor's note: This column originally appeared in the November 2020 issue of Healthcare Hygiene magazine.
Everyone who enters a healthcare facility, especially during this global pandemic, has the right to expect the highest standards for patient safety and quality. One of the most fundamental ways to achieve high levels of each is to create and value a culture in which hand hygiene is second nature for every staff member and volunteer.
Given that compliance rates, when measured accurately and reliably typically fall below 50 percent, a sound and evidence based strategic framework is essential, providing a check list of hand hygiene program elements that all work synergistically to ensure optimized hand hygiene behavior.
To that end, we have created a new framework: “The 6 essential elements of hand hygiene.” See the accompanying graphic and feel free to reproduce for your infection prevention, epidemiology, patient safety and quality leadership team to use as a guide when thinking about your organization’s strategic approach to hand hygiene.
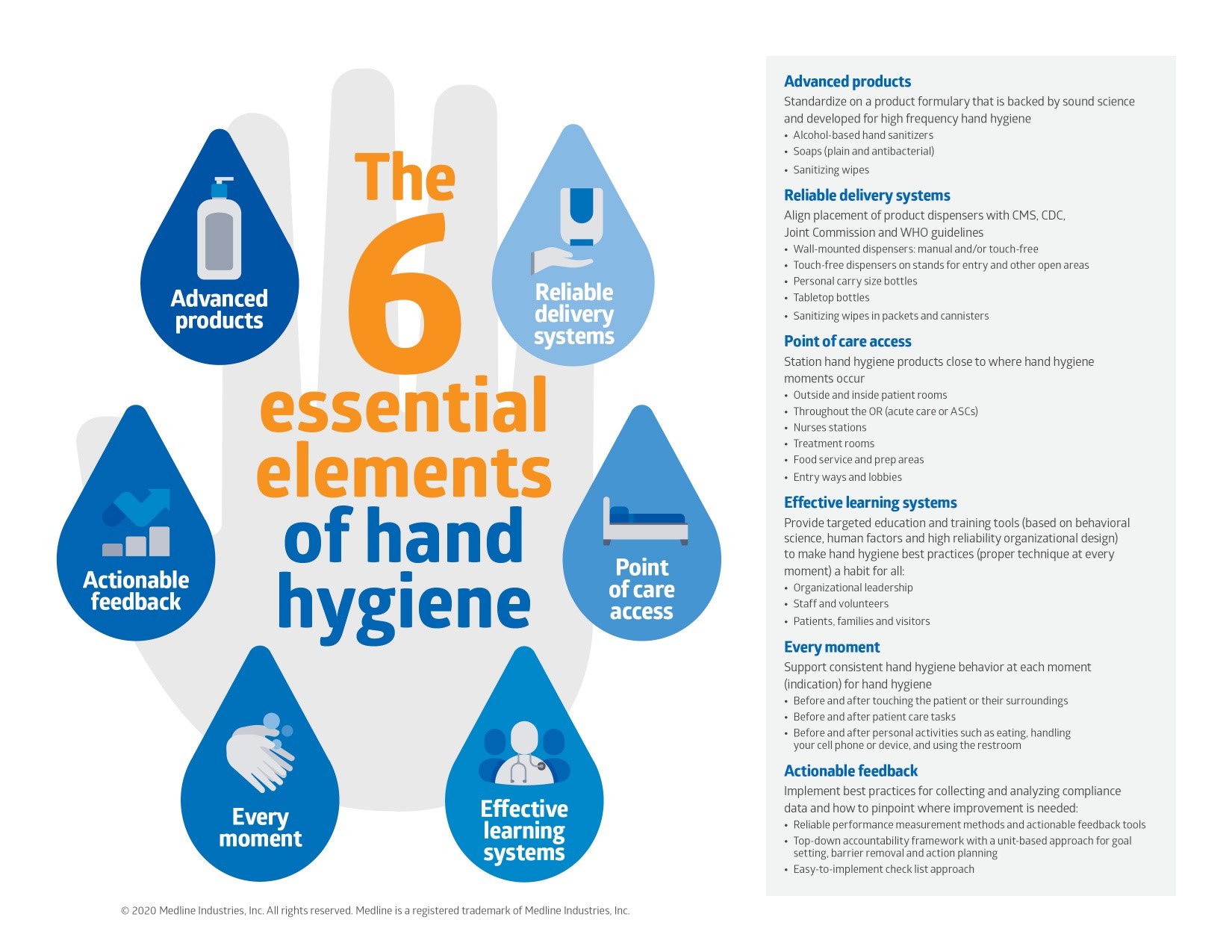
The six essential elements are: Advanced products, reliable delivery systems, point of care access, effective learning systems, every moment and actionable feedback. Each is accompanied by guidelines for how to get each one right:
Advanced Products
Select a standardized product formulary that is supported by sound science and developed for high frequency hand hygiene:
• Alcohol-based hand sanitizers
• Soaps (plain and/or antibacterial)
• Sanitizing wipes
Reliable Delivery Systems
Align placement of product dispensers with CMS, CDC, Joint Commission and WHO guidelines:
• Wall-mounted dispensers: manual and/or touch-free
• Touch-free dispensers on stands for entry and other visitor areas
• Personal carry size bottles
• Tabletop bottles
• Sanitizing wipes in packets and cannisters
Point of Care Access
Station hand hygiene products close to where hand hygiene moments occur:
• Outside and inside patient rooms
• Throughout the OR (acute care or ASCs)
• Nurses stations
• Treatment rooms
• Food service and prep areas
• Entry ways and lobbies
Effective Learning Systems
Provide targeted education and training tools (based on behavioral science, human factors and high reliability organizational design) to make hand hygiene best practices (proper technique at every moment) second nature for all:
• Organizational Leadership
• Staff and volunteers
• Patients, families and visitors
Every Moment
Support consistent hand hygiene behavior at each moment (indication) for hand hygiene:
• Before and after touching the patient or their surroundings
• Before and after patient care tasks
• Before and after personal activities such as eating, handling a phone or device, and using the restroom
Actionable Feedback
Implement best practices for collecting and analyzing data and understand how to pinpoint where improvement is needed:
• Reliable performance measurement methods and actionable feedback tools
• Top-down accountability framework with a unit-based approach for goal setting, barrier removal and action planning
• Easy-to-implement check list approach
We think this will go a long way in helping healthcare organizations think about hand hygiene in a systematic way that contributes to highly reliable staff performance (aka sustained increases in compliance).
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the vice president of patient safety innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
Introducing The 5 “Rights” of Hand Hygiene: A New Strategic Framework for Healthcare Organizations
By Paul Alper
This column originally appeared in the September 2020 issue of Healthcare Hygiene magazine.
Reflecting on the approach developed to help avoid drug and medication errors -- that is the six rights of medication administration: the right patient, right drug, right dose, right time, right route of administration and right documentation, it seemed to make sense that hand hygiene should also have its own set of “rights.”
Such a framework could guide facility leadership to a fully integrated approach comprised of essential elements necessary to finally “get hand hygiene right.”
Thinking about what components would be needed to drive a successful hand hygiene program, the following analogous framework evolved, followed by some questions we might want to ask ourselves:
• Right product: Are we always choosing to use soap, sanitizer, and wipes when we should?
• Right dispenser/delivery system: Do we always have the right dispenser strategically placed so we have access to hand hygiene products when we need them? Is placement chosen in accordance with the most up-to-date guidance from CMS, CDC, Joint Commission and WHO? And for those areas we might not have wall dispensers, do we have an appropriate personal carry size available for staff?
• Right point of care: Are we always enabling hand hygiene at every point of care; are we removing obstacles that might impede doing the right thing?
• Right moment: Are we teaching the “moments” for hand hygiene in a way that staff truly understands them? Are we emphasizing all the behaviors that should trigger a hand hygiene event including personal activities such as cell phone and tablet use?
• Right user: Are we training and motivating all the users whose proper hand hygiene behavior is essential for an optimized patient safety environment? Does this include patients, families, and visitors, not just staff and volunteers? Are we giving staff and volunteers actionable feedback on hand hygiene performance in a way that motivates sustained improvement and always “doing the right thing?”
Defining each right and adding in guidance led to the creation of this new framework for any facility to use as a strategic guide: Introducing the 5 “rights” of hand hygiene™:
The Right Product
Standardize on a product formulary that is backed by sound science and developed for high frequency hand hygiene:
• Alcohol-based sanitizers
• Soaps
• Sanitizing wipes
All used with the “right” technique
The Right Delivery System
Align placement of product dispensers with CMS, CDC, Joint Commission and WHO guidelines:
• Wall-mounted dispensers: manual and/or touch-free
• Touch-free dispensers on stands for entry and other open areas
• Personal carry size bottles of sanitizer for use when limited or no access to wall dispensers
• Tabletop bottles where wall mounted dispensers are not feasible
• Sanitizing wipes in packets and canisters
The Right Point of Care
Station hand hygiene products close to where hand hygiene moments occur:
• Outside and inside patient rooms
• Throughout the OR (acute care or ASCs)
• Nurses stations
• Treatment rooms
• Food service and prep areas
• Entry ways and lobbies
The Right Moment
Support consistent hand hygiene behavior at each moment (indication) for hand hygiene:
• Before and after touching the patient/resident or their surroundings
• Before and after patient care tasks
• Before and after personal activities such as eating, handling your cell phone or device, and using the restroom
The Right User
Provide targeted education and training on proper hand hygiene technique and routine performance feedback to primary user groups:
• Staff and volunteers
• Patients, families, and visitors
We think this will go a long way in helping healthcare organizations think about hand hygiene in a systematic way that contributes to highly reliable staff performance (aka sustained increases in compliance).
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
Self-Assessment in COVID-19: Know Your Baseline, Measure Your Progress
By Paul Alper
This column originally appeared in the August 2020 issue of Healthcare Hygiene magazine.
This month, we provide a facility-based self-assessment tool, informed by the latest guidance from CMS and the CDC. This is designed for infection prevention and clinical leaders to get a solid baseline of where they stand today and then conduct routine self-assessment updates to measure improvement. Accordingly, a scoring guide is provided.
A Hand Hygiene Self-Assessment Tool
Note that point values for each response are included as part of the questions, but these should be removed when using the tool with the units.
Select the response that best describes your facility and its routine practices related to hand hygiene:
1. Our facility has a comprehensive hand hygiene program that creates accountability for the following program elements 1.1 - 1.7:
1.1 Hand hygiene products and appropriate dispensers are available at all points of care with appropriate measures in place to ensure prompt replenishment when they are empty
a) Strongly Agree (10)
b) Agree (7)
c) Neither Agree nor Disagree (0)
d) Disagree (0)
e) Strongly Disagree (0)
1.2 Individual (personal carry) size hand sanitizers are provided for all staff and volunteers for use when hand hygiene is indicated but access to dispensers is not convenient
a) Strongly Agree (10)
b) Agree (7)
c) Neither Agree nor Disagree (0)
d) Disagree (0)
e) Strongly Disagree (0)
1.3 New and on-going staff are trained and educated routinely on performance expectations including the indications for hand hygiene along with proper technique and when to use soap vs. sanitizer
a) Strongly Agree (10)
b) Agree (7)
c) Neither Agree nor Disagree (0)
d) Disagree (0)
e) Strongly Disagree (0)
1.4 Staff are required demonstrate that they can do a proper 20 second hand wash + hand sanitization at training times
a) Strongly Agree (10)
b) Agree (7)
c) Neither Agree nor Disagree (0)
d) Disagree (0)
e) Strongly Disagree (0)
1.5 Patients, family members and visitors are educated on hand hygiene behavior expectations
a) Strongly Agree (10)
b) Agree (7)
c) Neither Agree nor Disagree (0)
d) Disagree (0)
e) Strongly Disagree (0)
1.6 Tools for such training are reviewed and updated at least annually
a) Strongly Agree (10)
b) Agree (7)
c) Neither Agree nor Disagree (0)
d) Disagree (0)
e) Strongly Disagree (0)
1.7 We use and update facility wide reminders of hand hygiene behavior expectations
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
2. Our units/departments are individually responsible for hand hygiene improvement and they are held accountable for meeting monthly/quarterly compliance growth targets.
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
3. Our units/departments leaders’ annual performance appraisal/bonus is tied in some way to meeting our hand hygiene improvement goals.
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
4. Our units/departments routinely identify obstacles and barriers to hand hygiene performance and then put in place action plans with the goal of eliminating them.
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
5. Our units/departments identify the obstacles and barriers to hand hygiene compliance using:
a. Direct Observation (10)
b. Group Discussion (7)
c. Other (1)
6. We measure hand hygiene compliance and give feedback on performance.
a. Daily or Weekly (10)
b. Monthly (7)
c. Quarterly (5)
d. Twice a year (1)
e. Once a year (0)
7. We celebrate when goals are achieved and identify what we will do differently when they are not.
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
8. When our goals are met, we then set a new, higher goal.
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
9. Psychological safety is the way we work in our facility – anyone can speak up when there is risk of doing harm without fear of retribution or other negative consequences.
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
10. Our organization’s senior leaders are responsible for modeling proper hand hygiene behavior and they are authentically engaged in our hand hygiene improvement efforts.
a. Strongly Agree (10)
b. Agree (7)
c. Neither Agree nor Disagree (0)
d. Disagree (0)
e. Strongly Disagree (0)
Add 10 points if you stop a healthcare worker as a matter of standard practice when conducting direct observation and they fail to perform hand hygiene, reminding them that they need to do so before providing care.
Scoring: Max Score including 10 Point Bonus = 170 Points
• 150-170: Outstanding. Stay diligent and focused
• 130-150: Excellent, but still room for improvement
• 100-130: Good, but should make getting over 110 a high priority for the next period
• Below 100: Poor, and in need of coaching and feedback. It’s an opportunity to take your safety culture and HH practices up a notch
We are still a long way from getting hand hygiene right; this is just one framework that requires no investment other than time and that might make sense to consider in some adapted form. Feel free to modify and adapt in any way that aligns well with your culture and organization.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
Performance Measurement, Feedback and Teamwork: Keeping the Foot on the Gas
This column originally appeared in the July 2020 issue of Healthcare Hygiene magazine.
By Paul Alper
While chatting with a few of my infection preventionist friends over the past few weeks, it was interesting that they all observed a similar pattern of behavior -- in March and April, hand hygiene compliance rates (whether measured with direct observation OR electronic monitoring) shot up into the 90s, if not hitting 100 percent routinely, and then, as dealing with COVID-19 became the new abnormal, rates have backed off a bit, albeit still much higher than pre-COVID-19 levels. But still, a drop off.
While not surprising, it begs the question, if COVID-19 doesn’t make us get hand hygiene right, what will? Maybe this is a good time to think again about the measurement and feedback process and ensure we are including space for barrier and obstacle identification at the unit level, and using such insight to drive unit-specific (team-based) behavior change. Times like these call for constant vigilance and diligence.
Unless you are using an electronic hand hygiene monitoring system, which it is estimated that less than 5 percent of the U.S. market is doing, that means using direct observation for a dual purpose -- first, for performance measurement and second, for barrier and obstacle identification. Here is a quick checklist for each:
A. Direct Observation for Performance Measurement based on the WHO 5 Moments for Hand Hygiene
1. Observation of hand hygiene behavior is accomplished using the WHO Data Collection Tool1 or a modified version as such was used in the Steed et al “HOW2 Study”2. Johns Hopkins Medicine also has created a Hopkins Medicine Monitoring Tool3.
a. Complete the top part of the header before commencing observation (except end time and duration)
b. A session should last no more than 20 minutes.
c. Record HHOs in the appropriate column and fill in the square corresponding to the indications for hand hygiene detected.
d. Record hand hygiene events or hand hygiene actions (HHEs) observed or missed for each indication.
i. Consider immediate feedback to any healthcare workers who have “missed” in order to recover and eliminate the practice of seeing misses and allowing care to proceed with unclean hands.
e. Glove use may be recorded only when a hand hygiene event is missed while the healthcare worker is wearing gloves.
f. At the end of the session, record end time and duration.
2. Compile the Data. Data from each Observation Form should be entered into a master data base such as Excel. Total hand hygiene events for a period are aggregated and divided by the total number of HHOs to determine the Compliance Rate for specific periods of time (week, month, quarter, year) for specific units as well as aggregated for the entire organization.
3. Create Graphs and Reports. Performance graphs and appropriate reports should be created and then shared with unit and organization leadership.
4. Give Front Line Staff Feedback against unit specific goals. Front line workers should be provided with performance feedback as immediate as possible after report creation.
5. Celebrate successes when goals are met; stay the course when results fall short.
6. Persistently continue the cycle.
B. Direct Observation for Barrier and Obstacle Identification (consider using or adapting the Joint Commission’s Hand Hygiene Targeted Solutions Tool [TST]4 for data capture and overall approach)
1. Deploy direct observers to collect a total of 30 missed hand hygiene opportunities per unit.
2. After missed opportunities are noted, the direct observers should approach staff, provide verbal feedback and ask what was the reason for the miss?
i. Capture and cluster the reasons to see which are the major obstacles for that particular unit.
3. Conduct mini focus groups with each unit to review the data, highlight primary obstacles and barriers observed on that unit and agree on unit-based changes (= action plan) to eliminate the obstacles and thus increase compliance. Keep it positive and opportunity embracing - not negative or punitive sounding.
a. It is important to set unit specific (again, team based) improvement goals.
4. Measure performance post the mini focus groups and Action Plan implementation using A above, or your electronic system if you have one in place, to track progress against goals and give feedback to the units.
5. Celebrate successes when goals are met; stay the course when results fall short.
6. Persistently continue the cycle.
This approach has been shown to drive statistically significant improvement. Kelly et al, 20165 achieved aggregate performance increase on four test units of 23.5 percent within six months. A three- to four-unit, four- to six-month pilot will help you see if it works for your organization.
While data from direct observation may be overstated, if collected consistently, it should provide a sound tool for measuring baseline plus real improvement along with the impact of initiatives designed to drive sustainable growth in hand hygiene behavior. Let’s be sure we keep our foot firmly on the gas to retain early COVID-driven gains in all aspects of infection prevention and patient safety.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. WHO Data Collection Tool
2. Steed C, et al. (2011). Hospital hand hygiene opportunities: Where and when (HOW2)? The HOW2 Benchmark Study. Am J Infect Control. 39(1), 19–26. doi:10.1016/j.ajic.2010.10.007
3. Hopkins Medicine Monitoring Tool
4. Joint Commission TST for Hand Hygiene
5. Kelly W, et al. (2016) Use of the Targeted Solutions Tool and Electronic Monitoring to Improve Hand
Hygiene Compliance. Paper presented at the 2016 SHEA meeting.
Hand Hygiene During the Covid-19 Pandemic: A Practical Guide for Long-Term Care Facilities
By Paul Alper
This column originally appeared in the June 2020 issue of Healthcare Hygiene magazine.
The pandemic has been disproportionately hard on the nation’s long-term care facilities (LTCFs.
Here are some big numbers; according to a recent New York Times1 article, while 11 percent of all coronavirus cases in the U.S. have occurred in long term care facilities, a staggering 35 percent of all U.S. coronavirus deaths are nursing home residents or workers.
Populations in LTCFs are at a high risk of being infected by, and dying from, the coronavirus, according to the Centers for Disease Control and Prevention.2 COVID-19 is known to be particularly lethal to older adults with underlying health conditions, and can spread more easily through congregate facilities, where workers move from room to room in a confined environment, according to the same New York Times article.
At least 28,100 residents and workers have died from the coronavirus at LTCFs in the U.S., according to the May 11 New York Times database. The virus so far has infected more than 153,000 individuals at 7,700 facilities.
While reducing the risk of infection requires a multi-modal approach, hand hygiene remains one the most important elements of an infection control program. This month’s column is devoted providing a framework for a best practice hand hygiene framework for LTCFs. Prior columns offered quite a bit of advice, and I recommend you refer to the November 2019 column that provided a checklist to drive higher hand hygiene compliance, as well as:
• December 2019 for a self-assessment tool (change the word “unit” to “facility” to make it work at the facility, versus Unit level)
• February 2020 for information on the importance of gloves as part of a total hand hygiene program
• March 2020 for a robust approach to the WHO 5 Moments of hand hygiene
• April 2020 for information on the importance of moisturizers
• May 2020 for advice for hand hygiene at home for healthcare professionals
Following is a simple checklist to use as a framework for a best-practice program that incorporates the CMS, CDC, JC and WHO guidance on hand hygiene.
1. Make hand hygiene a corporate priority. C-suite engagement, psychological safety (anyone-workers, volunteers and patients- can and do speak up when HH is missed) and role modeling by leaders organizational norms become integral to the facility’s safety culture.
2. Identify barriers and obstacles to hand hygiene with front line staff as well as leadership and establish action plans to remove them.
3. Train staff and volunteers on the WHO 5 moments for hand hygiene. How to properly sanitize hands with an alcohol based hand sanitizer and how to wash hands with soap and water.
a. Include training on resident and family engagement along with your C. difficile hand hygiene protocol.
b. Train residents and families on hand hygiene basics and explain your program and commitment to excellence to them.
4. Measure (audit) hand hygiene performance against goals, give feedback routinely and celebrate successes. See my March 2020 column for more on this.
5. Product Access - Dispensers etc.:
a. Place automatic (touch-free) dispensers with alcohol based hand sanitizer on stands at all entrances with appropriate instructional signage.
b. Place wall mounted dispensers with alcohol based hand sanitizer outside and inside (as close to bedside as is reasonable) all resident rooms, in elevator lobbies (can also use stands here if more convenient) and any other area where care is going to take place or hand hygiene is indicated.
i. Optional - provide alcohol-based hand sanitizing wipes at bedside for resident and family use as appropriate while considering the self-care and cognitive capabilities of each individual resident.
c. Place wall mounted soap dispensers adjacent to all sinks throughout the facility. Use pump bottles if wall space is not available.
d. Place wall mounted dispensers with alcohol based sanitizer at all nurses’ stations. If wall space is not convenient, consider table top pump bottles (at least 12 ounces or larger).
e. Provide 2-4 ounce size personal carry size bottles of alcohol based hand sanitizer (or small packets, such as 20 count, of hand sanitizer wipes) to all caregivers with the training that hand hygiene should take place using wall mounted dispensers when convenient, but when not, to use the personal carry size.
Hand hygiene consistency, diligence and vigilance are “musts” in today’s pandemic environment and adherence to the above Check List should provide an effective road map to achieving them.
References:
1. New York Times
2. Centers for Disease Control and Prevention
3. Based on CDC Guidance
4. CDC CoVID-19 Guidance
5. CDC CoVID-19 Nursing Home Checklist
6. WHO Guidance
7. WHO CoVID-19 Guidance
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share ideas that might be of interest in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
Hand Hygiene at Home During the Covid-19 Pandemic: A Practical Guide for Healthcare Professionals
By Paul Alper
Editor's note: This column originally appeared in the May 2020 issue of Healthcare Hygiene magazine.
Now that we are in the middle of this pandemic suddenly thrust upon us, making hand hygiene -- both on and off the job -- a matter of utmost importance when it comes to the health and safety of ourselves and family, it seems like a practical guide to hand hygiene at home might make sense and be helpful.
What does the CDC and WHO Say About Hand Hygiene in the Context of Covid-19?
Here is the CDC Hand Hygiene Guidance: “Wash your hands often with soap and water for at least 20 seconds especially after you have been in a public place, or after blowing your nose, coughing or sneezing.
• If soap and water are not readily available, use a hand sanitizer that contains at least 60 percent alcohol.
o Cover all surfaces of your hands and rub them together until they feel dry.
• Avoid touching your eyes, nose, and mouth with unwashed hands.”
Here are the WHO Recommendations for Hand Hygiene in the Context of Covid-19:
• Wash your hands with soap and running water when hands are visibly dirty.
• If your hands are not visibly dirty, frequently clean them by using alcohol based handrub [sanitizer] or soap and water.
Protect yourself and others from getting sick. Wash your hands:
• After coughing or sneezing
• When caring for someone who is sick
• Before, during and after you prepare food
• Before eating
• After toilet use
• When hands are visibly dirty
• After handling animals or animal waste
Most public health experts would add the following to the list of “when to clean hands” in the age of this pandemic and social distancing:
• After leaving the grocery, drug store or any retail environment
• When returning home from any outing
• After handling any delivered items such as boxes, take out deliveries or groceries
Always keep in mind the importance of a full 20-second wash with brisk scrubbing or rubbing of wrists, thumbs, all sides of and in between the fingers, fingertips, palms and backs of the hands. Proper technique does matter. This applies both to soap and water washing as well as sanitizing with an alcohol-based sanitizer.
Product Selection
With “rogue” products now being offered for sale, here are some facts about how soaps and sanitizers are regulated by the FDA and what you should look for when buying them:
• Alcohol based hand sanitizers should only be used if they have a minimum of 60 percent alcohol. Many healthcare professionals are migrating to at least 70 percent or higher for both professional and home use.
o Avoid non-alcohol-based sanitizers, as they are not as effective on pathogenic microorganisms and they are not recommended by the CDC or WHO.
• While under normal circumstances sanitizers must be made in FDA registered plants and have an NDC (National Drug Code) assigned and printed on the label, the FDA is allowing a liquid sanitizer with a final concentration of 80 percent v/v ethyl alcohol or 75 percent v/v isopropyl alcohol to be made, waiving most of the normal manufacturing requirements but with a set of specific formula and manufacturing guidelines.
That’s why you see a number of distilleries now making hand sanitizer. Note that these products are liquids as opposed to the normal gels or foams on the market so don’t be surprised when it comes out runny if you buy one of these.
• Soaps can be plain or antibacterial and the latter are also regulated by the FDA. Note that the CDC and WHO do not give a specific recommendation for using plain or antibacterial soap. The key is to clean all parts of the hands for 20 seconds and not miss any surface from the wrists to the fingertips.
o The CDC web site states: “handwashing mechanically removes pathogens.”
Antibacterial soaps must also be made in an FDA-registered plant and contain an NDC number on the label.
• Antibacterial soaps and sanitizers must be tested for safety, efficacy against 31 microorganisms including MRSA and stability. This is also known as GRASE or Generally Regarded as Safe and Effective.
o While the CDC states on its web site that: “ABHR [alcohol-based handrubs] formulations containing 80 percent ethanol or 75 percent isopropanol, both of which are in the range of alcohol concentrations recommended by CDC, inactivate SARS-CoV-2,” the FDA does NOT allow for virucidal efficacy claims on soaps or sanitizers sold to hospitals or consumers. This is an inconsistency that often causes confusion. We would like to see alignment between CDC and WHO guidance and FDA regulatory requirements.
Are there any special considerations with regard to skin health in the light of the COVID-19 pandemic?
There has been a dramatic increase in clinician hand hygiene due to the Pandemic. It is more important than ever to protect the skin’s natural barrier by applying a moisturizer routinely during the day after soap-and-water handwashing and especially before leaving the facility.
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share ideas that might be of interest in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
Moisturizers: An Essential Component of Proper Hand Hygiene and Skin Health
By Paul Alper
This column originally appeared in the April 2020 issue of Healthcare Hygiene magazine.
Just as important as proper cleaning and sanitizing of hands is proper moisturizer use. We will address when and why to use moisturizers as an essential element of your overall hand hygiene and skin health strategy and ultimately, part of your facility’s infection prevention and control approach. For purposes of simplicity, we will use the term “moisturizer” here to mean collectively lotions, creams, moisturizers and other similar names.
The CDC states that to maintain skin health:1
• “Lotions and creams [aka moisturizers] can prevent and decrease skin dryness that happens from cleaning your hands
• “Use only hand lotions approved by your healthcare facility because they won’t interfere with hand sanitizing products”
Why is overall skin health vital to a successful hand hygiene program? Contact dermatitis is extremely common among nurses, ranging in prevalence surveys from 25 percent to 55 percent. Actually, as many as 85 percent relate a history of having skin problems.2,3 High-frequency hand hygiene, especially in today’s pandemic environment, can lead to chronic contact dermatitis among healthcare workers, no matter how mild the soaps and sanitizers they use are.
Hand hygiene products, along with household detergents and cleaners, can damage the skin by causing denaturation of stratum corneum proteins, changes in intercellular lipids, decreased corneocyte cohesion and decreased stratum corneum water-binding capacity.4
Among these, the main concern is the depletion of the lipid barrier that may result from contact with lipid-emulsifying detergents and lipid-dissolving alcohols.4 Frequent handwashing can lead to depletion of surface lipids with resulting deeper action of detergents into the superficial skin layers. During dry seasons and in individuals whose skin is typically dry, this lipid depletion occurs more quickly.4
When the natural barrier of the skin breaks down drying and even cracks in the skin can occur which may allow bacteria an entry point and increases risk of infection. Applying a moisturizer can prevent those effects along with the itching, redness, flaking, and pain that can accompany skin breakdown. It also helps to avoid chronic damage and changes in the normal skin flora.5
Using a moisturizer will help promote and maintain healthy skin, reduce transepidermal water loss (TEWL), increase skin hydration, and improve overall skin tolerance. Moisturizing hands with the right product reduces microbial shedding from the skin and will protect people from picking up viruses and reduce the likelihood of transmission.6
Selecting a product that is non-sensitizing, non-irritating, and compatible with gloves, sanitizers and CHG based products if they are used in the facility (for example for skin decolonization) is essential. It should be an emollient rich product that is free of alcohol, artificial fragrances, and dyes. Staff should use only the moisturizers provided by the facility to ensure glove and CHG compatibility. Personal products should only be used after a shift ends and at home -- never during the work day.
Healthcare workers should use a moisturizer:
• At the start of a shift after washing hands with soap and water and drying them thoroughly
• After washing and drying hands throughout the day to keep the skin well hydrated
• At the end of the shift, again after washing and drying hands
There has been a dramatic increase in clinician hand hygiene due to the COVID-19 pandemic. It is more important than ever to protect the skin’s natural barrier. Cracks and fissures can allow easy access to microorganisms. Clinicians should be applying a moisturizer routinely during the day after soap-and-water handwashing to protect from the risk of infection, discomfort, and potentially chronic skin issues.7
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. https://www.cdc.gov/handhygiene/providers/index.html
2. Larson E, et al. Prevalence and correlates of skin damage on the hands of nurses. Heart & Lung. 1997;26:404-412.
3. Lampel HP, et al. Prevalence of hand dermatitis in inpatient nurses at a U.S. hospital. Dermatitis. 2007;18:140-142.
4. Skin Reactions Related to Hand Hygiene. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care., U.S. National Library of Medicine, Jan. 1,1970, www.ncbi.nlm.nih.gov/books/NBK144008/.
5. Diamond F and Popescu S. Hand Hygiene and Infection Control: Skin Care Supports Patient Care. Infection Control Today. May 19, 2008. www.infectioncontroltoday.com/hand-hygiene/hand-hygiene-and-infection-control-skin-care-supports-patient-care.
6. Gale R. Don't Just Wash Your Hands to Prevent Coronavirus. Moisturize Them, Too. The Washington Post. March 6, 2020, www.washingtonpost.com/lifestyle/wellness/hand-washing-coronavirus-moisturizer-dry/2020/03/06/ede43874-5fcb-11ea-b014-4fafa866bb81_story.html.
7. Gajanan M. COVID-19: How to Avoid Dry Skin After Washing Your Hands. Time. March 11, 2020, time.com/5800275/covid-19-wash-hands-dry-skin-tips/.
Direct Observation: A Robust Approach for the WHO 5 Moments
By Paul Alper
Editor's note: This column originally appeared in the March 2020 issue of Healthcare Hygiene magazine.
I was recently asked by the head of infection prevention at a community hospital how to design a robust hand hygiene direct observation program. Their objective was to get the most accurate compliance data possible, as they got ready for an upcoming Joint Commission visit.
I thought there might be others who would like to know how to accomplish this given that direct observation is still the most widespread method used for hand hygiene performance measurement. This is in spite of the fact that direct observation has been shown to have many shortcomings, including lack of accuracy due to the Hawthorne Effect,1 lack of inter-rate reliability and bias on the part of the observers.
An Evidence-Based Approach
Drawing on the methodology of a landmark study2 by Steed, et al. that, for the first time, scientifically determined the number of hand hygiene opportunities (HHOs) in various settings using a disciplined approach to direct observation-based on the WHO 5 Moments, I have created a “best practices for direct observation” checklist.
Here is a summary and checklist for how facilities could implement the approach used in the study and acquire compliance data that is as accurate and reliable as we likely can expect data from direct observation to be.
Checklist for a Robust Direct Observation Program
Note that apps to capture and compile direct observation data for smart phones and tablets are available from your App Store or provider. We will address the manual process in Steps 3, 4 and 5 below but simply follow app instructions if you are using one of them instead.
1. Train observers. This should consist of the following three steps:
a. Total familiarization with The WHO 5 Moments Poster.
b. Complete familiarization with the WHO Hand Hygiene Training Films and Slides Accompanying the Training Films.
c. Practice doing observations with feedback from a lead observer or infection prevention manager.
2. Assess inter-rater reliability. Conduct this routinely to ensure consistency of data collection.
a. In its simplest form, observers could conduct direct observations together and compare results. A lead observer could also accompany observers to reinforce consistent results.
3. Conduct Direct Observation. Observation of hand hygiene behavior is accomplished using the WHO Data Collection Tool or a modified version as such was the case in the HOW2 Study. Johns Hopkins Medicine also has created a Hopkins Medicine Monitoring Tool.
a. Complete the top part of the header before commencing observation (except end time and duration)
b. A session should last no more than 20 minutes.
c. Record HHOs in the appropriate column and fill in the square corresponding to the indications for hand hygiene detected.
d. Record hand hygiene events or HHEs (or hand hygiene actions) observed or missed for each indication.
e. Glove use may be recorded only when a hand hygiene event is missed while the healthcare worker is wearing gloves.
f. At the end of the session, record end time and duration.
4. Compile the data. Data from each Observation Form should be entered into a master data base such as Excel. Total hand hygiene events for a period are aggregated and divided by the total number of HHOs to determine the Compliance Rate for specific periods of time (week, month, quarter, year) for specific units as well as aggregated for the entire organization.
5. Create graphs and reports. Performance graphs and appropriate reports should be created and then shared with unit and organization leadership.
6. Give front-line staff feedback. Front line workers should be provided with performance feedback as immediate as possible after report creation.
7. Create performance improvement action plans. Units and departments should be responsible and accountable for action plans to remove unit specific barriers and obstacles to proper hand hygiene behavior.
While data from direct observation may be overstated, if collected consistently, it should provide a sound tool for measuring real improvement and the impact of initiatives designed to drive sustainable growth in hand hygiene behavior.
Thanks to the HOW2 authors for the creative research that inspired this column.
References:
1. Srigley JA, Furness CD, Baker GR and Gardam M. (2014). Quantification of the Hawthorne Effect in Hand Hygiene Compliance Monitoring Using an Electronic Monitoring System: A Retrospective Cohort Study. BMJ Qual Saf. 23, 974–80.
2. Steed C, Kelly JW, Blackhurst D, Boeker S, Diller T, Alper P and Larson E. (2011). Hospital hand hygiene opportunities: Where and when (HOW2)?
The HOW2 Benchmark Study. Am J Infect Control. 39(1), 19–26. doi:10.1016/j.ajic.2010.10.007
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC. He can be reached for questions or comments at paul@next-levelstrategies.com.
Gloves: An Essential Component of Proper Hand Hygiene
By Paul Alper
This column originally appeared in the February 2020 issue of Healthcare Hygiene magazine.
Just as important as proper cleaning and sanitizing of hands, is proper glove use. While there are a variety of gloves used in healthcare, we will address the proper use of non-sterile, single use (disposable) exam gloves and their role in protection of the patient as well as the healthcare provider.
Complete Hand Hygiene Education
Hand hygiene education must include instruction on proper glove use, not just when and how to perform hand washing or sanitizing. Wearing gloves does not replace proper hand hygiene practices but should be used as indicated according to accepted guidelines.
Using an alcohol based hand sanitizer before donning gloves is essential to ensure no contamination of other gloves in the box as they are removed from the original box or storage container.
Guidelines and Recommendations – When to Wear/When to Remove or Change
The WHO (World Health Organization), CDC (Centers for Disease Control) and OSHA (Occupational Safety & Health Administration) all recommend glove use during a procedure or task when contact is likely:
• With blood or bodily fluids
• With mucous membranes
• With non-intact skin
• With other potentially infectious materials
• When handling or touching contaminated equipment or surfaces
Knowing when to remove or change gloves is just as important as when to wear them. Gloves protect the healthcare worker as well as the patient but they also pose a risk if not removed when contaminated. Timing of and technique for donning and doffing of gloves is essential to eliminating the risk of HAI transmission.
he CDC, WHO and OSHA all have recommendations regarding removing and changing of gloves:
The CDC recommendations include:
• Remove gloves after caring for a patient
• Do not wear the same pair of gloves for the care of more than one patient (this also means never washing them between patients)
• Change gloves when moving from work on a soiled body site to a clean body site on the same patient or if another clinical indication for hand hygiene occurs
• Carefully remove gloves to prevent hand contamination
The WHO recommends that gloves should be removed:
• As soon as gloves are damaged or suspected of being damaged
• When contact with blood, other body fluids, non-intact skin and mucous membranes has occurred and ended
• When there is an indication for handwashing or sanitizing
OSHA’s recommendations for when to change gloves include:
• As soon as practical when contaminated, torn or punctured
• Changing gloves between patients regardless of condition
Common Usage Errors
Common errors with proper glove use include prolonged use, using when not indicated and the presence of jewelry.
Prolonged use and over use of gloves also poses a risk. Using gloves for an extended period of time can result in the transmission of disease causing microorganisms due to a possible failure to identify an indication for hand hygiene and then performing it.
When there is no potential for exposure to blood or body fluids, mucous membranes, non-intact skin or contaminated environmental surfaces, gloves should not be worn.
Jewelry should never be worn during patient care, even if wearing gloves. Nor should it be worn during proper hand hygiene.
Skin Health and Gloving
Occupational dermatitis is a common issue among healthcare workers. High frequency hand hygiene can potentially remove protective lipids from the skin, making it more prone to drying and irritation. This increases the risk of colonization with bacteria and can potentially result in the spread of disease causing microorganisms.
Proper and frequent use of a latex and nitrile compatible lotion, especially at the start and end of the shift, along with the use of gloves manufactured with therapeutic additives such as oatmeal and aloe are two ways to reduce the risk as well as help soothe and recover hands that have become dry, chapped and irritated.
Importance of Glove Size
Selecting proper sized gloves is essential to achieving proper protection. In general, gloves should cover the entire hand and wrist and feel snug without being too tight and allow full movement of the hand and fingers.
Like most things in life, one size does not fit all. Common disposable gloves range in size from extra small to extra-large. Be sure to follow the manufacturer’s guidance on how to properly fit each healthcare worker on your staff.
Steps to Take Now
• Review your facility’s hand hygiene training and education and be sure that proper use of gloves is adequately covered including demonstrations for proper donning and doffing technique
• Use direct observation not only for measuring hand hygiene compliance but proper glove use adherence, taking the time for interventional feedback when errors occur.
o Make the unit leadership responsible for proper glove use by all front line workers
• Foster a psychologically safe patient safety culture so that healthcare workers feel safe talking to anyone at any level about their proper use of gloves as well as hand hygiene
Proper glove use is often taken for granted, but attention to all of the details surrounding proper use – when, why and how to use them is essential for the prevention of HAIs and the overall safety of everyone one in your facility’s community.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the VP Patient Safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
Electronic Monitoring Systems: Essential Considerations
By Paul Alper
This column originally appeared in the January 2020 issue of Healthcare Hygiene magazine.
In my October column I said the following about electronic monitoring: “While a nascent category that is still in the early adopter phase, the migration from human direct observation or secret shoppers, to validated, automated, systems that constantly measure healthcare worker performance is here to stay. The scientific evidence is becoming clear that the future “gold standard” will be the combination of direct observation (DO) as a “coaching and obstacle identification tool” with electronic monitoring as the “measurement tool.”
I thought it might make sense to follow that column up with a checklist of essential consideration” should you and your organization decide to consider potential adoption in the near future and need a framework to create an RFP.
While there are systems with many more features to consider, these are the ones that are most important to think about.
For some, you will have to choose between options based on what would best suit your organization’s culture and your budget. Of course, whatever system you consider, there should be published outcomes evidence in support of adoption:
1. Numerator capture (how many HH events actually occurred). The system must aggregate BOTH soap and sanitizer hand hygiene events into an accurate numerator with a minimum 98 percent validated capture.
2. Denominator calculation (how many HH events should have occurred). You must choose: does the system base its HH rate on a) IN and OUT HH or b) Or the WHO 5 Moments for HH? In either case, you will want to see evidence on how the denominator is calculated and how it has been validated.
3. Reporting level. You will have to choose – does the system base its reporting on a) group/unit/department level hand hygiene rates or b) Individual healthcare worker HH rates?
4. Report/dashboard access. The system should provide intuitive, unambiguous reports and dashboards both via direct system access (such as by logging on to the system) and also via “push” or automatically generated reports via email.
5. C. diff room reporting. The system should provide the ability to see both soap- and sanitizer-event trending so that real time feedback can be given to staff as to whether or not they are complying with the typical C. diff protocol - the switch to soap and water hand hygiene from alcohol-based hand sanitizer which does not kill C. diff spores.
6. Type of Infrastructure. You must choose: a) is the system exclusively dedicated to hand hygiene compliance measurement (aka a stand-alone infrastructure) or b) one that works like an application (APP) with a new or previously installed real-time locating system (RTLS) infrastructure. RTLS systems will typically support multiple APPs such as nurse call, workflow assessment, people and equipment tracking etc. If you do go with option b, you will want to explore the level of hand HH expertise on the part of the RTLS/APP provider to be sure you’re comfortable that they have the requisite capability needed to support your organization’s enterprise wide adoption.
7. Behavior change support. Successful outcomes (for example sustainable compliance improvement, culture change and reduced infections) are going to be very much dependent on how you approach changing your culture from one that relies on Direct Observation for measurement (with its typical overstatement of real compliance rates by up to 300 percent) to one that relies on virtually real time data that will likely reveal a 30 percent to 40 percent compliance range when you first implement it.
You will want to verify that the system under consideration a) provides an evidence based behavior change framework, b) supports “psychological safety” – the ability for anyone to speak up in a professional and appropriate manner to colleagues (peers, superiors and subordinates) when hand hygiene does not occur when it should have and c) uses a positive and pro-active approach to dealing with data denial – this is the attitude by some on staff who will take the position that “my behavior is fine, it’s the data/system that’s inaccurate.”
8. Reminders to do HH at the point of care. You will have to decide if this a “must have,” “nice to have,” or “doesn’t matter to us” feature. This is accomplished, for example and depending on the system, by lights on the badge or dispenser, badge vibrations or by a voice reminder at the dispenser.
While I think there will be some exciting next-generation technologies introduced over the next couple of years that will leapfrog the current generation in terms of new and important features, accuracy, reliability, evidence in support of adoption and lower cost, I hope this proves helpful. Happy New Year!
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share ideas that might be of interest in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the vice president of patient safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
A Self-Assessment Tool: How Do Your Units Compare?
By Paul Alper
This column originally appeared in the December 2019 issue of Healthcare Hygiene magazine.
In last month’s column, (see page 34 in the November 2019 issue), I presented an evidence-based checklist for how to drive improvement with what you have; that is, regardless of how you are training, educating, measuring and giving feedback, the checklist provides a framework for driving improvement that has been shown to work when implemented with solid discipline.
This month, we will take that a step forward and provide a self-assessment tool for unit managers to use for the purpose of getting a solid baseline of where they stand today and then conducting routine self-assessment updates to measure improvement. Also included is a scoring guide so that infection preventionists (IPs) can compare their units and use the scoring to identify those units that need the most immediate coaching and feedback.
A Hand Hygiene Self-Assessment Tool
Note that point values for each response are included as part of the questions, but these should be removed when using as the tool with the units. Select the response that best describes your unit and its routine practices. Be honest and frank:
- Our unit is responsible for hand hygiene improvement and we are held accountable for meeting monthly/quarterly compliance growth targets.
- Strongly agree (10)
- Agree (7)
- Neither agree nor disagree (0)
- Disagree (0)
- Strongly disagree (0)
- Our unit leadership’s annual performance appraisal/bonus is tied in some way to meeting our hand hygiene improvement goals.
- Strongly A\agree (10)
- Agree (7)
- Neither agree nor disagree (0)
- Disagree (0)
- Strongly disagree (0)
- Our unit routinely identifies obstacles and barriers to hand hygiene performance and then puts in place action plans with the goal of eliminating them.
- Strongly agree (10)
- Agree (7)
- Neither agree nor disagree (0)
- Disagree (0)
- Strongly disagree (0)
- Our unit identifies the obstacles and barriers to hand hygiene compliance using:
- Direct observation (10)
- Group discussion (7)
- Other (1)
- We measure hand hygiene compliance and give feedback on performance:
- Daily or weekly (10)
- Monthly (7)
- Quarterly (5)
- Twice a year (1)
- Once a year (0)
- We celebrate when goals are achieved and identify what we will do differently when they are not.
- Strongly agree (10)
- Agree (7)
- Neither agree nor disagree (0)
- Disagree (0)
- Strongly disagree (0)
- When our goals are met, we then set new, higher goal.
- Strongly agree (10)
- Agree (7)
- Neither agree nor disagree (0)
- Disagree (0)
- Strongly disagree (0)
- Psychological safety is the way we work; anyone can speak up when there is risk of doing harm (such as not doing proper hand hygiene when it is indicated) without fear of retribution or other negative consequences.
- Strongly agree (10)
- Agree (7)
- Neither agree nor disagree (0)
- Disagree (0)
- Strongly disagree (0)
- Our organization’s senior leaders are responsible for modeling proper hand hygiene behavior and they are authentically engaged in our hand hygiene improvement efforts.
- Strongly agree (10)
- Agree (7)
- Neither agree nor disagree (0)
- Disagree (0)
- Strongly disagree (0)
Add 10 points if you stop a healthcare worker as a matter of standard practice when doing Direct Observation and they fail to perform hand hygiene, reminding them that they need to do so before providing care.
Scoring:
- 100: Outstanding. Stay diligent and focused!
- 80-99: Excellent, but still room for improvement.
- 60-79: Good, but should make getting more than 80 a high priority for the next period.
- Below 60: Poor. An opportunity to take your safety culture and hand hygiene practices up a notch. In need of coaching and feedback.
We are a long way from “getting hand hygiene right,” and this is just one framework that requires no investment other than time and that might make sense to consider in some adapted form. Feel free to modify and adapt in any way that aligns well with your culture and organization. A three- to four-unit pilot will help you see if it works for you.
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share any ideas that might be of interest and help in this monthly column paul@next-levelstrategies.com. Connect with me on LinkedIn.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs and is now the vice president of patient safety innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
A Checklist to Drive Higher Compliance: Using Actionable Feedback to Drive Meaningful Change
By Paul Alper
This column originally appeared in the November 2019 issue of Healthcare Hygiene magazine.
I’m often asked a simple question by healthcare organizations: “We are not ready to change products or put in an electronic monitoring system yet – but we do want to use evidence-based practices to drive improvement with what we have in place today.”
Giving that some thought, I’ve put together a checklist based on an actionable feedback model that should help you make some changes in the way your organization thinks about hand hygiene compliance, its safety culture and the social fabric of your community. The checklist is based on insights and inspiration gained from some interesting studies1-3 basic PDSA cycles thinking and my 35-plus years of working in many aspects of hand hygiene and patient safety innovation. Here’s the list:
- Make hand hygiene compliance a unit/ward/department responsibility. Hand hygiene compliance improvement should be a defined responsibility at the Unit level with the manager responsible and accountable for meeting growth targets.1 A great way to help ensure results is to tie this directly to the performance appraisal process.
- Identify the unit-specific barriers and obstacles to hand hygiene behavior plus action plans to remove Them. Each unit becomes responsible for identifying its unique barriers and obstacles to hand hygiene compliance and putting in place specific action plans to remove them.1 This might be best accomplished using Direct Observation to capture those unit specific behaviors that need to be modified.2
- Establish unit-specific improvement goals. Each unit is responsible for establishing its own realistic improvement goals monthly, which should be achievable assuming the action plans are carried out as assigned.1 The end game is that the barriers and obstacles identified can be continuously reduced or eliminated.
- Measure performance and give routine feedback consistently. Use the most robust approach to measurement available to your organization within the resource constraints (time, people, money) and provide performance feedback on a consistent basis (weekly to start, migrating to monthly, for example). Be sure to measure the behavior standard that you train staff on – in/out, WHO 5 Moments, CDC or a variant you’ve chosen for your organization. If the approach is electronic monitoring, ensure its accuracy has been validated. If you’re using direct observation, be sure you control for inter-rater reliability.
Note: A quick thought about the Secret Shopper concept: it seems difficult to comprehend why an organization would allow the practice of seeing potential risk (not cleaning hands) and then only marking down the missed hand hygiene event without intervening to ensure care is delivered with cleaned hands. It’s a troubling concept.
- Celebrate successes and then set a new, higher goal. When goals are not met, have the same barrier/obstacle/action plan conversation.
- Make psychological safety a cultural norm. Anyone at any level within the organization can remind anyone else regardless of their level or status when hand hygiene is missed in a professional, “out of patient view” way, without the fear of reprisal.
- Make leaders responsible for modeling and authentic engagement. C-suite leaders must know about, support and model the behaviors expected across the entire staff community.
In one of the studies on which the checklist is based on, Childers, et al. used this basic framework at Memorial Sloan-Kettering Cancer Center, and a baseline rate of hand hygiene of 60-70 percent increased to 97 percent as measured with direct observation.1
Kelly, et al. also used a similar approach with electronic monitoring for measurement at the Greenville Memorial Hospital and achieved a 25 percent increase in hand hygiene compliance with a 43 percent reduction in MRSA infections.3
Steed, et al. also used a variant at the same organization combining modified use of the Joint Commission’s Targeted Solutions Tool with electronic monitoring for measurement and achieved aggregate performance increase on four test units of 23.5 percent within six months that was statistically significant.2
To be clear, we are a long way from “getting hand hygiene right” – this is just one framework that requires no investment other than time that might make sense to consider in some adapted embodiment that aligns well with your culture and organization. A three- to four-unit pilot will help you see if it works for you.
Let me know what you think and please send me your specific hand hygiene challenges, frustrations and nagging problems – I’ll share any ideas that might be of interest and help in this monthly column paul@next-levelstrategies.com.
Paul Alper, BA, led the launch of PURELL®, invented the first electronic hand hygiene monitoring system proven to reduce infections while improving behavior and eliminating costs, and is now the vice president of patient safety innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
- Son C, Chuck T, et al. Practically speaking: Rethinking hand hygiene improvement programs in health care settings. Am J Infect Control. 39(9), 716–724. 2011.
- Kelly W, Blackhurst D, et al. Use of the Targeted Solutions Tool and Electronic Monitoring to Improve Hand Hygiene Compliance. Paper Presented at the 2016 SHEA Conference.
- Kelly W, Blackhurst D, McAtee W and Steed C. Electronic Hand Hygiene Monitoring as a Tool for Reducing Healthcare-Associated Methicillin-Resistant Staphylococcus aureus Infection. Am J Infect Control. 44(8), 956-957. 2016.
Hand Hygiene: The Problem We Only Think We Solved
By Paul Alper, BA
Editor's note: This column originally appeared in the October 2019 issue of Healthcare Hygiene magazine.
All truth passes through three stages. First, it is ridiculed. Second, it is violently opposed. Third, it is accepted as self-evident. – Arthur Schopenhauer, philosopher
What would Ignaz Semmelweis think if he were able to observe the state of healthcare hand hygiene today? The Austrian physician who, while working at Vienna General Hospital’s first obstetrical clinic, first proved the link between hand hygiene (disinfection with a chlorinated lime solution) and the reduction of infections (child bed fever) in 1847, might wonder why so much, yet so little, progress has taken place in the 172 years since his discovery. In spite of the innovations highlighted below, global hand hygiene compliance rates remain no greater than 50 percent, and patients are still getting infections from pathogens such as methicillin-resistant Staphylococcus aureus (MRSA), methicillin-susceptible Staphylococcus aureus (MSSA), vancomycin-resistant Enterococcus (VRE), associated with transmission by unclean hands.
Semmelweis certainly experienced the first two stages of truth as Schopenhauer observed them. Many contemporary doctors were offended at the notion they should wash their hands, and not only ridiculed him, but also shunned him. Acceptance of the benefits of hand hygiene as “self-evident” took the work of Louis Pasteur and Joseph Lister and occurred years after Semmelweis’s death.
Since that seminal work more than 100 years ago, there have been only three major, disruptive changes in healthcare hand hygiene.
1. “Bag in a Box” (BIB) soap technology in the 1970s:This invention introduced sealed, sanitary soap cartridge refills with a proprietary valve that only fit compatible, proprietary dispensers. The inner workings of the dispenser were engineered to accept the BIB refill. Think “razor” (the dispenser) and “disposable razor blade” (bag in a box refill) business model. Pushing or pulling the dispensing bar activated a valve that allowed the soap to flow from the dispenser. This sanitary approach eliminated the use of gallons that could fill any bulk reservoir soap dispenser by simply pouring in the liquid.
Sani Fresh® invented the original BIB with a “pull” style dispenser, and eventually Kimberly-Clark purchased that company. GOJO accelerated this trend by entering into the market with its “push” style dispenser. Of note is that the bulk soap sold in the range of $3 to $5 per gallon, but with BIB refills costing about $2 to $3 per 800 ml refill, the price of soap went up to more than $10 to $12 per gallon. Mocked as ridiculously expensive by purchasing departments, the Sani Fresh team pushed its sanitary benefits with clinical decision makers and today, sealed soap and sanitizer refills are the standard of care in healthcare, with the use of bulk, pour and fill style dispensers virtually non-existent.
2. Alcohol Hand Sanitizer: “We’ll never use that stuff; we wash with soap and water,” was the typical response from infection preventionists in the late 1980s and 1990s when introduced to alcohol-based hand sanitizers (or hand disinfectants and handrubs, as they were also known largely in Europe). The idea of no longer using soap and water was ridiculed by infection preventionists! It was a violation of everything they took to be self-evident when it came to soap and water handwashing.
The widespread use of alcohol for hand disinfecting began in the 1970s in Europe but didn’t come into serious use in U.S. hospitals and healthcare facilities until the late 1980s when PURELL® and other brands were first introduced into institutional use. Once healthcare workers realized how much faster and efficient it was to clean hands with an alcohol hand sanitizer, objections went away, and institutional use accelerated. Use of alcohol hand sanitizer further increased with the retail launch of PURELL and the first TV ads that ran in 1997, which led to its use becoming a societal norm and part of the popular culture. The CDC’s updated Healthcare Hand Hygiene Guideline in 2002 cemented alcohol based hand sanitizers as the absolute standard of care and the primary way healthcare workers sanitized their hands, the exception being when hands are visibly soiled or recently exposed to bodily fluids or spores at which point they need to be washed with soap and water.
3. Electronic monitoring for hand hygiene compliance. Hand hygiene compliance, whether a worker properly performs hand hygiene when indicated, has typically been measured by direct observers attempting to watch healthcare workers. This practice mimics that of “secret shoppers,” whereby the observers try to remain unknown to the workers and attempt to discreetly record whether they do hand hygiene when indicated. This system is inherently flawed however, because if a secret shopper observes the lack of hand hygiene and does not intervene, they are enabling risk of harm to the patient.
The problem is that healthcare workers—no matter how discreet the secret shopper is—know when they are being observed and behave differently. This phenomenon is known as the Hawthorne Effect: people behave differently when they know they are being watched. Further compounding the problem is that direct observation typically only captures less than 1 percent of all hand hygiene opportunities, which is not a statistically valid sample. The result is that compliance rates are dramatically overstated – typically by up to 300 percent based on studies,1 and this means that compliance measured as 90 percent with direct observation may in reality be only 30 percent.
A number of electronic systems to measure compliance were launched during the 2010s. These systems eliminated many of the shortcomings of direct observation, such as the Hawthorne Effect and small sample size, since electronics can capture nearly 100 percent of hand hygiene events at all times. Die-hard defenders of direct observation certainly ridicule and oppose the technology’s adoption, citing direct observation as the “gold standard” (which it was until this more accurate, reliable and effective technology category came along). While a nascent category that is still in the early adopter phase, the migration from human direct observation or secret shoppers to validated, automated, systems that constantly measure healthcare worker performance is here to stay. The scientific evidence is becoming clear that the future “gold standard” will be the combination of direct observation as a “coaching and obstacle identification tool” with electronic monitoring as the measurement tool. 2-3 Further, overstated rates, such as those proven by Srigley et al, enable a false sense of complacency that unacceptably puts patients at risk. Given the ability to mitigate the risk of patient harm with this new technology, it is likely that it will overcome the ridicule and opposition phases and move towards widespread acceptance.
And, the market is moving, too. For instance, a growing number of progressive health systems have gone with full commercial implementation (the Greenville Health System, now Prisma Health, in South Carolina and the Atlantic Health System in New Jersey among them). Further, most of the group purchasing organizations that have added the category of e-monitoring and studies have demonstrated its clinical and economic benefits.4
Whether e-monitoring will become the standard of care will depend on whether a system that is simple, affordable and overcomes some of the inherent implementation and cultural barriers in currently available systems is developed – and there is no reason why that shouldn’t happen.
The Future of Hand Hygiene
Despite these innovations, healthcare hand hygiene still has a lot of room for improvement, given that compliance is only about half of what it should be. For instance, healthcare workers who must clean their hands 40 to 50 times a shift should be confident that the products they use actually improve skin health, but products they find drying remain a barrier.
Additionally, healthcare hand hygiene should be multidisciplinary, drawing from fields such as human factors engineering, behavioral science, and data science to propel the next innovations.
An inventory of the prospective attributes of that best in class, next generation hand hygiene approach might look like this:
• Hand hygiene products (soaps, sanitizers and lotions) that are “skin friendly,” with the lowest possible risk of healthcare worker intolerance
• Dispensers that are not only able to measure compliance, but indicate product levels and any performance issues, ensuring product is always available and empty dispensers are a thing of the past
• Training and educational tools based on sound behavioral science that drive high levels of sustainable performance improvement with requisite culture change
• Affordable, validated methodology for measuring compliance accurately and reliably, with feedback approaches that foster psychological safety (everyone feels safe reminding anyone to do hand hygiene when an opportunity is missed) and the development of a just safety culture
• Predictive analytics that forecast hot spots (risk of low compliance and/or hospital acquired infection transmission) before they occur
• And what roles will artificial intelligence, learning systems and the Internet of Things play? Probably significant ones.
One would hope that we are about to put all the learning and capabilities to work and that by the 200th anniversary of Semmelweis’s seminal research, proper hand hygiene will be a habit for every healthcare worker around the world.
Whatever the next disruptive innovation brings, it is time to get hand hygiene right. We live in an age of value-based healthcare, and variability of performance should not and cannot be tolerated. It will take early adopter pioneers, willing to accept the ridicule, knowing that what they are doing represents the truth for themselves and those for which they care.
Paul Alper led the launch of GOJO’s PROVON® and PURELL® brands in the late 1980s and 1990s. He invented and was highly involved in the clinical research behind the first hand-hygiene electronic monitoring system. He is now the vice president of patient safety Innovation for Medline Industries, Inc. through an exclusive engagement with his consulting practice, Next Level Strategies, LLC.
References:
1. Srigley JA, Furness CD, Baker GR and Gardam M. Quantification of the Hawthorne
Effect in Hand Hygiene Compliance Monitoring Using an Electronic Monitoring System: a
Retrospective Cohort Study. BMJ Qual Saf. 23, 974-80. 2014.
2. Boyce JM. Electronic Monitoring in Combination with Direct Observation as a Means
to Significantly Improve Hand Hygiene Compliance. Am J Infect Control. 45(5), 528-535. 2017.
3. Kelly JW, Blackhurst D, McAtee W and Steed C. Electronic Hand Hygiene Monitoring
as a Tool for Reducing Health Care Associated Methicillin-Resistant Staphylococcus aureus Infection. Am J Infect Control. 44(8), 956-957. 2016.
4. Kelly W, Blackhurst D, Steed C, Boeker S and McAtee W. Use of the Targeted Solutions Tool and Electronic Monitoring to Improve Hand Hygiene Compliance. Paper presented at the 2016 SHEA annual meeting.