A new review explores the physiology behind and proposed management strategies for body-wide symptoms of the post-acute sequelae of SARS-CoV-2 (PASC), otherwise known as “long COVID.” The review is published ahead of print in the American Journal of Physiology-Cell Physiology.
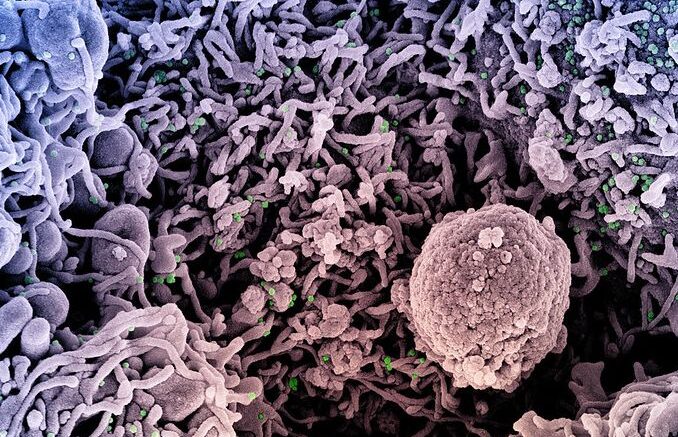
SARS-CoV-2, the virus that causes COVID-19, has infected more than 49 million people in the U.S. Studies estimate that about 26% of people who had COVID-19 experience long-term complications after they have recovered from the initial infection. These symptoms range in severity, body systems affected and symptom length. Researchers suspect a number of long-term complications stem from direct viral tissue damage, or damage to the ACE2 receptors through which the virus enters the body.
Authors of a new review examine many of the organ systems affected in people with long COVID from a pathophysiological perspective. They also give their hypotheses about why specific symptoms occur and how to manage them. Here is a breakdown:
Pulmonary System: Long-term complications of the pulmonary system include shortness of breath, scarring of lung tissue and dependence on oxygen or ventilator use. Overproduction of inflammatory proteins is thought to be one mechanism behind these issues. Management strategies may include frequent imaging of the lungs to detect structural abnormalities and functional assessment with a standard six-minute walking test.
Cardiovascular System: Cardiovascular issues post-infection may include chest pain, an increase in heart rate when transitioning from sitting to standing (postural orthostatic tachycardia syndrome) and inflammation of the heart muscle (myocarditis). Imaging of the heart and monitoring heart rate through a 24-hour Holter monitor are among the proposed protocols.
Blood Clots: The literature on long COVID suggests using a routine dose of anticoagulant medication to manage blood clots in people recovering from COVID-19. This symptom is relatively rare compared to other signs of long COVID.
Neurological and Mental Health Issues: Sleep problems, “brain fog,” headaches and lingering loss of taste and smell are common neurologic complications associated with COVID-19. People experiencing these and other long COVID symptoms may also be at a higher risk for developing depression, anxiety and post-traumatic stress disorder. The review authors emphasize the importance of psychiatric screening and appropriate treatment for these disorders and suggest olfactory training to help regain sense of smell.
Kidney Disease and Diabetes: Kidney disease and new diagnoses of diabetes can also be part of a long COVID diagnosis. Prolonged inflammation and the steroids used to treat inflammation may contribute to these sequelae. Extended fecal shedding of the virus can lead to ongoing gastrointestinal problems in some people. Establishing care with specialists in these areas may be recommended.
Musculoskeletal System: Muscle weakness and body aches may linger due to the ACE2 receptors that are located in the muscles and soft tissues throughout the body. Musculoskeletal complaints can lead to physical impairment after weeks or months of inactivity. Exercise—through rehabilitation or under the supervision of a medical professional—and good nutrition play a significant role in recovery from these symptoms.
“There are a number of considerations that are yet to be addressed in the COVID-19 pandemic. … It remains unclear how the presentation of long haul COVID-19 will be impacted in individuals infected with these [novel variant] strains of the virus,” the review authors wrote. “Specifics in terms of symptoms of patients with these novel variants stratified by age and race also remain to be seen and will depend on larger studies.”
Source: American Physiological Society