Water Quality and Conservation
By Richard Dixon and David W. Koenig, PhD
This article originally appeared in the December 2023 issue of Healthcare Hygiene magazine.
Water is vital for life on this planet. Some organisms have up to 90 percent water by body weight. Humans contain up to 60 percent water. Water is also critical in the survival and transmission of pathogens in the healthcare environment. Microorganisms require water to grow and reproduce.
Water requirements for growth are best defined in terms of water activity, aw, of the substrate rather than as water concentration. The water activity of a solution is expressed as aw = P/Po, where P is the water vapor pressure of the solution and Po is the vapor pressure of pure water at the same temperature. Addition of a solute to an aqueous solution in which a microorganism is growing will have the effect of lowering the aw, with a concomitant effect upon cell growth.
Every microorganism has a limiting ‘aw’ below which it will not grow, e.g., for streptococci, Klebsiella spp., Escherichia coli, Clostridium, and Pseudomonas spp. the value is 0.95. Staphylococcus aureus is the most resistant and can proliferate with an aw as low as 0.86. Some fungi can grow with an aw of 0.7. Therefore, wet environments favor the survival and therefore transmission of fomites.
Water is also key to the cleaning and disinfection of these surfaces. Cleaners and disinfectants are mostly water based either being used as a ready-to-use (RTU) or diluted with water at the point if use. Taken together water is critical for life, critical for pathogen transmission and survival, and critical for infection control. Therefore, it is important to understand water as it enters the healthcare facility and all the forms it can be encountered in that facility.
Water Quality
In the United States potable water or drinking water is regulated by the Environmental Protection Agency (EPA). The EPA sets the legal limits on more than 90 chemical and microbial contaminates for drinking water. The EPA mandates that any water treatment technology must meet a disinfectant standard and that the resulting product is free of pathogens.
Although potable water standards ensure safe drinking water, the water is not sterile. Following EPA standards ensures that drinking water has a low probably of containing at risk organisms. The disinfectant is added at the treatment facility and is at a level that allows for preservation of the drinking water through the potable water distribution system to point of use. The level of disinfectant can be relatively low at the point of use dependent on the demand in the distribution system. The disinfectant added is not sufficient to control contaminates that may be introduced into the distribution system due breaks in the system. Once the water is removed from the distribution system, that level can decrease rapidly due to demand. Importantly for infection control measures, the design of the buildings’ water distribution system can significantly alter water quality. The water in the building can pass into water heaters, heat exchangers, faucet aerators, and lie stagnant in dead legs before use. Ice machines can be a challenge for microbial control. Furthermore, in older buildings, mixed metals and plastics used in the distribution system due to renovations and building additions can impact mineral build-up and biofilm development. Water systems that are not managed appropriately allow waterborne pathogens to increase in types and numbers resulting in infections in susceptible individuals.
Innovations for optimizing water quality, safety and conservation in a healthcare facility are insightful, forward-thinking, and necessary. By employing a holistic approach to water management, facilities can not only enhance operational efficiency and reduce the cost of the water supply from the local municipality but also contribute to environmental sustainability and most importantly patient, staff, physician, and visitor safety. The next sections will review those processes and provide insights in optimizing water usage while reducing pathogen transmission risk.
Water Microbiology: The main risk of bacteria in drinking water is usually due to contamination events that introduce human fecal organisms to the water distribution system. The most common problem organisms associated with drinking water are Vibrio cholerae, Vibrio parahaemolyticus, Salmonella enterica, Shigella dysenteriae, Shigella flexneri, Shigella boydii, Shigella sonnei, Escherichia coli, and Campylobacter sp. Problem viruses include adenovirus, astrovirus, hepatitis A and E viruses, rotavirus, norovirus, and enteroviruses, including coxsackieviruses and polioviruses. Other bacteria associated with water and infection include Mycobacterium, Legionella, Burkholderia, Klebsessia, and Ralstonia. Fungi can be isolated from tap water distribution systems, but their types and numbers are poorly defined. The most detected fungi are Aspergillus, Cladosporium and Penicillium. Giardia and Cryptosporidium are the most problematic protozoans found in water systems.
Point-of-Use Water Disinfection Technology
Reactive Oxygen Species (ROS): An innovative method of reducing pathogens in water is the use of point-of-use (POU) of ROS such as superoxide radicals, hydrogen peroxide, and hydroxyl radicals, are molecules that can cause oxidative stress and damage to pathogen cellular components. Water, on the other hand, is a fundamental molecule that supports life and biochemical processes by acting as a solvent and facilitating various reactions within cells but does not kill any bacteria.
Germicidal Ultraviolet Light: The most effective systems are those ultraviolet lights with the C wavelength (UVC) at 254 nanometers, which can easily disinfect the incoming or return water lines.
Copper-Silver Ionization: The proposal of using hot water produced at the central boiler room, treated through a copper/silver ionization system for bacterial control, is a proactive step to ensure safe water distribution. This measure, particularly in combating bacteria like Legionella, is both prudent and necessary, for safeguarding the well-being of all stakeholders in a healthcare facility.
Hand Hygiene Sinks That Use Ozonated Water: A smart flow sink that uses ozonated water to eliminate bacteria both on hands and on the sink, itself is a truly an easy way to eliminate harmful pathogens that collect in the P-trap below hand hygiene sinks. Ozonated water has been shown to be more effective than soap and water for bacterial removal from hands. This sink also provides a source of ozonated water for general cleaning and sanitizing. Convenient and twice as powerful as bleach. The sink is programmed to disinfect itself automatically, every hour, eliminating CPOs (Carbapenem-producing organisms, like Kleb’s pneumonia and E. coli) and preventing biofilm formation in the P-trap to prevent CPO outbreaks in a healthcare facility. And the system does not generate ozone into the air.
Engineering and Process Control Steps to Maintain Water Quality
Water Quality Measurement: Incorporating technology to monitor water quality parameters like hardness, pH, and total dissolved solids (TDS) is a crucial step toward ensuring the safety and suitability of water for various purposes. By setting and adhering to quality standards, you’re building a foundation for a consistent and reliable water supply throughout the facility.
Eliminate Dead-End Piping: Toward this end, it is important that a healthcare facility identify dead-end piping systems and segregate them from the active water lines. Keep in mind that most water distribution systems flow through copper pipes.
Eliminate Aerators on Sink Faucets: Aerators on sink faucets collect minerals and pathogens so their use should not be allowed on any sink in the healthcare facility.
Eliminate the Traditional P-Trap Under Sinks: An innovative approach to significantly reducing pathogen containing wet and dry biofilms in a traditional sink P-trap is to eliminate this 140-year-old method of sewer gas control with a straight vertical drainpipe. The sewer gas control is accommodated by using an automated negative pressure system from the drain piping air vent with exhaust to the facility roof. In addition, gate or ball shut off valves on the horizontal drain piping can be closed off periodically to have disinfectants poured into the sink drains with an appropriate amount of dwell time to kill the pathogens and the piping then re-opened back up for regular use. Also never dump patient medications, fluids, feces in a sink. Always follow the facility’s standard operating procedures for these components.
Ice Machines Cleaning and Disinfection: These units commonly used for producing ice cubes and crushed ice can become contaminated if not properly maintained, cleaned and disinfected. Contamination of ice machines can pose health risks, as the ice produced may encounter harmful microorganisms and impurities. Here are some potential sources of contamination and steps to prevent it:
Microbial Contamination: Bacteria, molds, and yeast can grow in the water supply, ice bin, and ice-making components of the machine. These microorganisms can multiply and contaminate the ice cubes.
Prevention: Regularly clean and sanitize the ice machine according to the manufacturer’s recommendations. This includes cleaning the ice bin, water lines, and ice-making components. Use approved cleaning agents to eliminate microbial growth. Even better, ultraviolet light systems with the C wavelength (UVC) at 254 nanometers, can easily disinfect the incoming water line. Another innovation would be to use modular ozonated water systems. An ozone generator system regularly sanitizes the water supply and kills bacteria, mold, and yeast. It produces an effective but safe amount of natural sanitizer that treats the machine interiors and sanitizes the remote storage bins and drains. No aerosolized ozone is dissipated into the air through this process.
Mineral Buildup: Over time, minerals from the water can accumulate in the ice machine, leading to scale buildup. This can affect the quality of the ice and the efficiency of the machine.
Prevention: Use a water filtration system to reduce mineral content in the water supply. Regularly descale the ice machine to remove mineral build-up. Follow the manufacturer’s instructions for use and de-scaling procedures plus the frequency.
Cross-Contamination: Improper handling of ice scoops and containers can lead to cross-contamination. If hands, containers, or utensils that are not properly sanitized encounter the ice, it can lead to contamination.
Prevention: Train staff in the proper hygiene practices when handling ice. Provide separate scoops for ice and other food items to prevent cross-contamination.
Airborne Contaminants: Airborne particles, dust, and debris can enter the ice machine and settle in the ice bin, leading to potential contamination.
Prevention: Keep the ice machine in a clean environment and regularly clean the surrounding area. Use air filters to minimize airborne contaminants entering the machine.
Improper Storage: Storing ice for extended periods without proper protection can lead to contamination from external sources.
Prevention: Use covered ice bins to protect ice from airborne contaminants. Dispose of ice that has been exposed for too long.
Water Quality: Poor water quality, including high levels of impurities or contaminants, can lead to poor-quality ice.
Prevention: Use water filtration and softening systems to improve the quality of the water used in the ice machine.
Inadequate Maintenance: Neglecting regular cleaning, maintenance, and inspection of the ice machine can increase the risk of contamination.
Prevention: Develop a predictive and preventative maintenance schedule and follow the manufacturer’s guidelines for cleaning and maintenance. Train staff on proper cleaning procedures
Water Conservation
AI-Driven Efficiency in Water Heating: Integrating artificial intelligence (AI) technology into zone booster heaters to manage hot water distribution effectively is a testament to the facility’s commitment to efficiency. By providing hot water precisely where and when it’s needed, you not only minimize wastage but also optimize energy usage. This thoughtful approach showcases the potential of technology in streamlining resource allocation. This can be achieved by heating the water in the central mechanical room at a lower temperature and using booster heaters at locations where hot water consumption is minimal or varied.
Waste Disposal Systems: A suggestion to eliminate macerator waste disposal systems is well-founded. By replacing processes that contribute to clogging municipal waste filtering systems, you’re fostering smoother waste management operations and potentially reducing maintenance costs. This proactive shift reflects a practical and sustainable approach to waste disposal.
Reverse Osmosis (RO) Water: This can be an eco-friendly and cost-effective approach, as RO systems waste a significant amount of water during the filtration process. Here are some ways you can reuse RO water:
Landscaping: One of the most common uses for reused RO water is for watering plants and gardens. Since RO water is free from many contaminants, it can be suitable for your plants. Be cautious, however, not to overdo it with sensitive plants, as RO water might lack some minerals that are beneficial for plant growth.
Humidifiers and Chillers: Reused RO water can be used in this type of equipment as it doesn’t contain minerals that can lead to scaling or deposits in these appliances. RO water for use in cooling towers, allows for less chemical use, and allows water to be re-used for significantly less cycles than municipal water.
Waste RO Water: Instead of putting the waste RO water into the sanitary drain system, it can also be disposed of into the storm sewar stream with permission of the local municipality. They also may be able to provide a tax credit using this disposal system as the water that goes into a sanitary system requires municipal processing.
Toilets: A very innovative process is to channel RO water for use in toilet flushing.
Compressing Municipal Water Supply: It’s a simple fact that along with the volume of water passing through your water meter is a volume of air. The volume of that air will vary as the water pressure fluctuates between static and dynamic pressure. The problem is that more than 99 percent of water meters are measured by volume, regardless of whether that volume is liquid or gas. A smart valve that compresses the municipal water before passing through a facility water meter takes long established principles of pressure and fluid dynamics, such as Boyle’s Law regarding gas pressure and volume, and Le Chatelier’s Principle of volumetric dynamics, and applies them in a new and financially rewarding application. This innovative process eliminates most of the air bubbles in the water and thus the volume is reduced and so is the cost.
Leak Detection Technologies: Smart meters and sensors can identify leaks and potential contamination points in water distribution systems, helping to reduce water losses and save money too. Leaks, even small ones, can waste significant amounts of water over time. Implement a proactive leak detection and repair program to fix leaks as soon as they are identified.
Educational Campaigns: Public awareness and education campaigns in the healthcare facility can promote water-saving behaviors and encourage individuals and communities to adopt water-efficient practices.
Water Audits and Monitoring: Conduct regular water audits to identify areas where water is being wasted. Install zone water meters to track usage in different parts of the facility and identify trends or anomalies.
Water-Saving Technologies: Consider installing water-saving technologies such as sensor-operated faucets, dual-flush toilets, and waterless urinals to reduce water usage.
Water Reduction Goals: Establish specific water reduction goals for your business and track progress regularly. Encourage departments to compete and collaborate on water-saving initiatives. Reward suggestions to employees who have innovative ideas to conserve water usage.
Regularly Review and Improve Strategies: Continuously monitor and assess your water conservation efforts. Regularly update your water conservation plan to incorporate new technologies and best practices. These innovations, along with healthcare policy support and public engagement, play a vital role in reducing water usage and ensuring the sustainable management of this precious resource. The key to successful water conservation in a healthcare facility is a combination of awareness, efficient technology, employee involvement, and a commitment to continuously improve your practices.
Other practical and novel conservation strategies
Rainwater from roofs or parking garage top floors can be reused for landscaping as well if it can be collected into a storage tank.
Smart irrigation systems use sensors, weather data, and soil moisture information to optimize irrigation schedules and flow amounts. Low-flow faucets, toilets, and showerheads use less water without sacrificing performance.
Smart meters and sensors can identify leaks in water distribution systems, helping to reduce water losses.
Public awareness and education campaigns in the healthcare facility can promote water-saving behaviors and encourage individuals and communities to adopt water-efficient practices.
Conduct regular water audits to identify areas where water is being wasted by using zone water meters.
Even small leaks can waste significant amounts of water over time. Fix all leaks promptly.
Consider installing water-saving technologies such as sensor-operated faucets, dual-flush toilets, and waterless urinals to reduce water usage.
Establish specific water reduction goals for your facility and track progress regularly.
Reward suggestions to employees who have innovative ideas to conserve water usage.
Continuously monitor and assess your water conservation efforts.
Regularly update your water conservation plan to incorporate new technologies and best practices.
Water quality, safety and conservation can be achieved if we all work together.
David W. Koenig PhD, is chief technology officer of DKMicrobios as well as a board member of the Environmental Services Optimization Project (EvSOP). He may be reached at dkmicrobios@gmail.com or (920) 527-8243.
Richard Dixon is the co-founder and board member of the Coalition for Community & Healthcare Acquired Infection Reduction (CHAIR). He may be reached at DixonConsulting@gmail.com or (772) 269-6491.
References:
1. Anaissie, E.J., Penzak, S.R. and Dignani, M.C., 2002. The hospital water supply as a source of nosocomial infections: a plea for action. Archives of internal medicine, 162(13), pp.1483-1492.
2. Asadi-Ghalhari, M. and Aali, R., 2020. COVID-19: Reopening public spaces and secondary health risk potential via stagnant water in indoor pipe networks. Indoor and Built Environment, 29(8), pp.1184-1185.
3. Casini, B., Aquino, F., Totaro, M., Miccoli, M., Galli, I., Manfredini, L., Giustarini, C., Costa, A.L., Tuvo, B., Valentini, P. and Privitera, G., 2017. Application of hydrogen peroxide as an innovative method of treatment for Legionella control in a hospital water network. Pathogens, 6(2), p.15.
4. Casini, B., Buzzigoli, A., Cristina, M.L., Spagnolo, A.M., Del Giudice, P., Brusaferro, S., Poscia, A., Moscato, U., Valentini, P., Baggiani, A. and Privitera, G., 2014. Long-term effects of hospital water network disinfection on Legionella and other waterborne bacteria in an Italian university hospital. Infection Control & Hospital Epidemiology, 35(3), pp.293-299.
5. Cazals, M., Bedard, E., Prévost, M. and Savard, P., 2022. Is your ice machine really clean? Uncovering the presence of opportunistic pathogens in hospital ice machines. Antimicrobial Stewardship & Healthcare Epidemiology, 2(S1), pp.s12-s13.
6. Cloutman-Green, E., Barbosa, V.L., Jimenez, D., Wong, D., Dunn, H., Needham, B., Ciric, L. and Hartley, J.C., 2019. Controlling Legionella pneumophila in water systems at reduced hot water temperatures with copper and silver ionization. American Journal of Infection Control, 47(7), pp.761-766.
7. Cotruvo, J.A. and Regelski, M., 2017. Overview of the current National primary drinking water regulations and regulation development process. Safe Drinking Water ActCRC.
8. De Giglio, O., Diella, G., Lopuzzo, M., Triggiano, F., Calia, C., Pousis, C., Fasano, F., Caggiano, G., Calabrese, G., Rafaschieri, V. and Carpagnano, F., 2020. Impact of lockdown on the microbiological status of the hospital water network during COVID-19 pandemic. Environmental Research, 191, p.110231.
9. De Giglio, O., Diella, G., Lopuzzo, M., Triggiano, F., Calia, C., Pousis, C., Fasano, F., Calabrese, G., Rafaschieri, V., Carpagnano, L.F. and Carlucci, M., 2021. Management of microbiological contamination of the water network of a newly built hospital pavilion. Pathogens, 10(1), p.75.
10. Decker, B.K. and Palmore, T.N., 2014. Hospital water and opportunities for infection prevention. Current infectious disease reports, 16, pp.1-8.
11. Edition, F., 2011. Guidelines for drinking-water quality. WHO chronicle, 38(4), pp.104-8.
12. Hozalski, R.M., LaPara, T.M., Zhao, X., Kim, T., Waak, M.B., Burch, T. and McCarty, M., 2020. Flushing of stagnant premise water systems after the COVID-19 shutdown can reduce infection risk by Legionella and Mycobacterium spp. Environmental Science & Technology, 54(24), pp.15914-15924.
13. Jeanvoine, A., Meunier, A., Puja, H., Bertrand, X., Valot, B. and Hocquet, D., 2019. Contamination of a hospital plumbing system by persister cells of a copper-tolerant high-risk clone of Pseudomonas aeruginosa. Water research, 157, pp.579-586.
14. Julien, R., Dreelin, E., Whelton, A.J., Lee, J., Aw, T.G., Dean, K. and Mitchell, J., 2020. Knowledge gaps and risks associated with premise plumbing drinking water quality. AWWA Water Science, 2(3), p.e1177.
15. Lavenir, R., Sanroma, M., Gibert, S., Crouzet, O., Laurent, F., Kravtsoff, J., Mazoyer, M.A. and Cournoyer, B., 2008. Spatio‐temporal analysis of infra‐specific genetic variations among a Pseudomonas aeruginosa water network hospital population: invasion and selection of clonal complexes. Journal of Applied Microbiology, 105(5), pp.1491-1501.
16. Ley, C.J., Proctor, C.R., Singh, G., Ra, K., Noh, Y., Odimayomi, T., Salehi, M., Julien, R., Mitchell, J., Nejadhashemi, A.P. and Whelton, A.J., 2020. Drinking water microbiology in a water-efficient building: stagnation, seasonality, and physicochemical effects on opportunistic pathogen and total bacteria proliferation. Environmental Science: Water Research & Technology, 6(10), pp.2902-2913.
17. Marchesi, I., Paduano, S., Frezza, G., Sircana, L., Vecchi, E., Zuccarello, P., Oliveri Conti, G., Ferrante, M., Borella, P. and Bargellini, A., 2020. Safety and effectiveness of monochloramine treatment for disinfecting hospital water networks. International Journal of Environmental Research and Public Health, 17(17), p.6116.
18. Moussavi, G., Fathi, E. and Moradi, M., 2019. Advanced disinfecting and post-treating the biologically treated hospital wastewater in the UVC/H2O2 and VUV/H2O2 processes: Performance comparison and detoxification efficiency. Process Safety and Environmental Protection, 126, pp.259-268.
19. Paduano, S., Marchesi, I., Casali, M.E., Valeriani, F., Frezza, G., Vecchi, E., Sircana, L., Romano Spica, V., Borella, P. and Bargellini, A., 2020. Characterisation of microbial community associated with different disinfection treatments in hospital hot water networks. International journal of environmental research and public health, 17(6), p.2158.
20. Salah, I., Parkin, I.P. and Allan, E., 2021. Copper as an antimicrobial agent: Recent advances. RSC advances, 11(30), pp.18179-18186.
21. Spina, S., Sbaraglia, M.N., Magini, R., Russo, F. and Napolitano, F., 2014. Studying a Hospital Distribution Network with a Stochastic End-uses Demand Model. Procedia Engineering, 89, pp.909-915.
22. Wang, N., Wang, Y., Bai, L., Liao, X., Liu, D. and Ding, T., 2023. Advances in strategies to assure the microbial safety of food-associated ice. Journal of Future Foods, 3(2), pp.115-126.
23. Wen, X., Chen, F., Lin, Y., Zhu, H., Yuan, F., Kuang, D., Jia, Z. and Yuan, Z., 2020. Microbial indicators and their use for monitoring drinking water quality—A review. Sustainability, 12(6), p.2249.
Engineered Infection Prevention: A New World of Better Disinfection of Air, Water and Surfaces
By Richard Dixon
This article originally appeared in the November 2023 issue of Healthcare Hygiene magazine.
Most people in the Middle Ages believed the world was flat. Brave adventurers such as the Vikings sailed across the ocean to the Atlantic seaboard, and the Chinese journeyed across the Pacific. They began the process of challenging this supposition. It then took several hundred years of voyages of discovery to map out the perimeter of North and South America in addition to inland expeditions such as the mapping experiences of Lewis and Clark in the U.S. and the Hudson Bay Company in Canada to define the nature of this vast land mass.
We do now believe the earth is round, humans have set foot on the moon, probes have landed on Mars, and a trip on a Boeing 787 Dreamliner from Seattle to Paris takes only 11 hours while we sit in comfort sipping a glass of wine. The moral of this story is that new ideas take time to become accepted, practiced, become the new normal and pave the way for the next new idea.
Many healthcare-acquired infections (HAIs) are caused by building-related environmental impacts of air, water, and surfaces, such as high-touch surfaces containing bacteria that are potentially harmful to patients and their subsequent transmission by people from surface to surface. Aerosols can also act as vehicles of microbial transmission. While we once thought medical procedures generated large amounts of aerosols, we now know that common actions like talking, shouting, singing, and coughing, generate far more aerosols than any medical procedures. Even the simple act of flushing the toilet can liberate dangerous pathogens with every use. Recent articles have nicely illustrated that aerosols from toilet plume can be potential vehicles for Clostridioides difficile and norovirus with deposition of infectious particles on bathroom or patient room touch surfaces. While handwashing and daily environmental cleaning have been the mainstays of environmental infection control for the past 170 years, today’s healthcare environments need new innovative processes in the battle with newer, more aggressive bacteria, viruses, and molds, such as the emerging threat of Candida auris.
The new ‘round’ world is about the use of engineered infection prevention (EIP) technologies, materials, automation, and strategies that are adjuncts or even replacements for traditional disinfection of air, water, and surfaces. One of most important risk assessment tools today is the quantitative microbial risk assessment (QMRA)1:
What level of bacteria/virus reduction is needed to result in a significant risk reduction?
What routes of exposure cause the greatest risk of infection?
What activities cause the greatest amount of exposure to pathogens?
How do pathogens spread via hands and surfaces and aerosolization in different environments? E.g., hospitals, outpatient clinics, urgent care, long-term care, etc.
Where does the greatest exposure occur?
How effective are hygiene products in reducing infection risks?
What is the impact of the number of persons in a facility that practice good hygiene on the other persons in the facility (herd hygiene)?
What is the impact of a product or process in practice on disease transmission in each environment?
What is the cost/benefit assessment of prevention interventions?
The tendency to reject new evidence or new paradigms such as EIP because it contradicts established norms, beliefs or paradigms is ironically known as the Semmelweis Reflex.2 Ignaz Semmelweis, of course, went to his grave unable to convince his fellow doctors of the need for hand hygiene to prevent hospital-acquired infections.
Here are some practical, safe, cost effective and sustainable examples of EIPs in our new ‘round’ world:
Germicidal ultraviolet (UV-C) light is a common type of UV well known for one hundred years for its ability to disinfect bacteria, viruses, and mold. Covering the span of invisible light from 200 to 280 nm, the most common and cost-effective wavelength is 254 nm. UV-C photons fuse neighbouring thymine and cytosine molecules on DNA strands preventing replication.
UV-C disinfection is commonly used for:
1. Water:
a. Water treatment
b. Wastewater treatment.
c. Potable drinking water systems
d. Ice machines
2. Air:
e. “Coil Cleaners” - Industrial and hospital HVAC air handling units to prevent mold, bacteria and biofilm formation in cooling coils, filters, and evaporation pans; very inexpensive and energy-efficient.
f. “In-Duct” - Hospital and office tower in-duct air disinfection systems designed to reduce pathogens, especially in recirculated air, which cause HAIs and Sick Building Syndrome, typically up to 99 percent.
g. Air Purifiers – Either stand-alone devices or located within devices downstream of HEPA or other filters; often ceiling-mount or portable; typically, 99 percent or higher reduction.
h. Upper Air Disinfection - UV-C fixtures installed near the ceiling to create a field of UV-C across the upper part of a room (above 7’6”). The efficiency of the system can be enhanced with ceiling fans that actively draw air into the UV-C field and circulate the air throughout the room.
3. Surfaces:
i. Mobile – Typically one, two or three UV-C towers on wheels that are manually placed in unoccupied rooms to disinfect spaces between occupancies; especially used in hospitals for “terminal cleans” between patients,
j. Built-In – Also known as “AutoUV,” devices that use redundant occupancy sensors, door contacts and smart algorithms to automatically disinfect spaces when unoccupied 10, 20, 30 times or more per day; typically used in hospital bathrooms, equipment rooms and utility rooms.
k. Robot systems - That autonomously or semi-autonomously disinfect important surfaces in hospitals, pharmaceutical plants, and laboratories.
l. Tunnel Systems – High-speed conveyor-based disinfection systems used in food processing facilities, medical device manufacturers, biohazardous waste recyclers, distribution centres, luggage handling, and secure government mail processing centers.
m. Personal items - Portable UV-C ‘box’ disinfectors have become popular for disinfecting small personal devices including smartphones, keys, masks, etc., especially since the onset of the COVID-19 pandemic.
UV-C is invisible and can cause sunburn or welder’s eye in just a few seconds so it is especially important that systems are designed to protect users against accidental exposure. Only purchase and use UV-C devices from reputable sources that haver registrations and certifications for UV-C from the U.S. EPA3 and Health Canada. 4
Relative Humidity (RH) in patient care is particularly important. RH in the range of 40 percent to 60 percent5 is optimal for the health of patients and is the sweet spot where growth and survivability of microorganisms is lowest. Infection rates double when RH drops from 30 percent to 40 percent, patients can also suffer from dehydration and impaired mucous membranes. More than 60 percent RH leads to mold and bacterial growth and can be uncomfortable for patients.
Ideally, for optimal comfort and infection control, RH should be maintained at 50 percent, plus or minus 5 percent. This may be harder to control in an older facility than a newer one with more sophisticated building automation system controls and better building envelope.6
Ozonated Water (OW) refers to the strong oxidative species often generated by splitting water molecules in the presence of energy and a catalyst in the new ‘round’ earth. OW is exceptionally good at disinfection and penetrating and preventing biofilms. sanitizer that can be used in the presence of people. In fact, OW is generated and used in our own cells. OW could be used as part of daily cleaning and disinfection process by Environmental Services staff. There are also hand hygiene sinks that generate up to 5 ppm ROS to safely disinfect hands, bowl and drain with each use, preventing microbial growth and the release of pathogenic bioaerosols.7
Antimicrobial Copper is registered as a biocide in the U.S. by the Environmental Protection Agency (EPA) in 2009 (including recently as effective in reducing coronavirus8) and in Canada with Health Canada’s PMRA9 in 2014. Both organizations recognize that when cleaned regularly, antimicrobial copper alloys surfaces kill greater than 99.9 percent of specific bacteria within two hours and continue to kill more than 99 percent of these bacteria even after repeated contamination. Since that time, numerous companies around the (round) earth have contributed to the research and manufacturing of different alloys for various high-touch surfaces:
Touch surfaces: One of the most common applications of antimicrobial copper is on touch surfaces in healthcare facilities, public spaces, and transportation. This includes items like doorknobs, handrails, bedrails, faucets, and elevator buttons. When these surfaces are made of copper or copper alloys, they can help reduce the transmission of pathogens through touch.
Overbed tables: These are the most touched surfaces in healthcare, used throughout each day for patient’s personal items, food serving, and clinical services like wound treatment, IVs, catheters, and phlebotomy. Overbed tables are virtually never cleaned or disinfected during a patient’s stay because environmental services staff are reluctant to remove medical devices or a patient’s personal belongings. In a perfect world, all overbed tables would be made of antimicrobial copper.
Countertops and work surfaces: In settings where hygiene is critical, such as laboratories and food preparation areas, copper countertops and work surfaces are used to inhibit the growth of bacteria and other microorganisms.
Medical equipment: Copper and copper alloys can be incorporated into various medical devices and equipment, including hospital bedrails, IV poles, and dental instruments, to reduce the risk of HAIs.
Personal protective equipment (PPE): Copper-infused fabrics and materials are sometimes used in the production of PPE, such as face masks and gloves, to provide an additional layer of protection against pathogens.
Handrails and guardrails: In public transportation systems like buses, subways, and trains, as well as in crowded public spaces, copper or copper alloy handrails and guardrails can help reduce the spread of germs from hand contact.
It is important to note that while antimicrobial copper can help reduce the presence of harmful microorganisms on surfaces, it is not a substitute for regular cleaning practices. Proper cleaning and hygiene protocols should still be followed in conjunction with the use of antimicrobial copper to ensure the highest level of safety and cleanliness. The effectiveness of antimicrobial copper may vary depending on factors such as the specific copper alloy used, surface morphology, and maintenance. However, it remains a valuable tool in the fight against the spread of infectious agents in various settings.
Silver: This metal has been used for centuries for its antimicrobial properties, and it continues to be used in various medical and industrial applications. Some common uses of silver in this context include:
Silver dressings: Silver-impregnated dressings are used in wound care to help prevent infection and promote healing. They release silver ions slowly, which can kill or inhibit the growth of bacteria in the wound.
Silver coatings: Silver coatings or nanoparticles are used in medical devices, such as catheters and implants, to reduce the risk of bacterial colonization and infection.
Water purification: Silver is sometimes used in water purification systems to disinfect water by killing harmful microorganisms.
Antimicrobial textiles: Silver nanoparticles can be incorporated into textiles, such as clothing and bed linens, to provide antimicrobial properties and reduce odors.
It is important to note that while silver can be effective against a wide range of microorganisms, including antibiotic-resistant bacteria, its use is not regulated and controlled due to potential toxicity or overexposure of silver ions. Additionally, ongoing research is being conducted to better understand the mechanisms of silver's antimicrobial action and to develop safe and effective silver-based products.
HVAC System Design Be aware that most older hospitals in the U.S. and Canada use recycled air in their HVAC systems with only recent builds that use 100 percent fresh air. This use of recycled air was for purely ‘energy’ savings while the newer designs focus on ‘infection prevention’ savings. Ironically though, the most energy efficient hospital HVAC system in Canada, Humber River Hospital, uses 100 percent outside air. HVAC systems that are designed with 100 percent fresh air supply also benefit from the use of High Efficiency Particle Air (HEPA) rated filters. True HEPA filters must capture at least 99.97 percent of particles that are 0.3 micrometers in size or larger. These filters are commonly used in medical facilities, cleanrooms, and applications where extremely high air quality is essential. The types of hospital environments where the benefit is most useful are operating rooms, intensive care units, clean rooms, decontamination, and medical equipment processing departments, burn and bone marrow transplant units.
Other types of filters called MERV (Minimum Efficiency Reporting Value) are also useful in different critical environments of a healthcare facility.
MERV 8: Often used as a pre-filter, MERV 8 filters capture small particles such as dust and mold spores with little restriction to flow. MERV 12 - 13: Improved filtration, effective against fine particles like smoke and some bacteria.
In summary, EIP technologies, materials, and strategies are adjuncts to cleaning and may be either adjuncts or replacements to traditional disinfection of air, water, and surfaces. Change is quite often slow to happen, but the COVID pandemic has proven that traditional cleaning and disinfection processes do not work well enough by themselves. EIP is therefore part of the ‘round’ world of new strategies to reduced healthcare and community-based infections and death. Infection prevention is everyone’s responsibility, so let us change together and use EIP to the maximum. Our lives depend on it.
Richard Dixon is co-founder and board member of the Coalition for Community and Healthcare Associated Infection Reduction (CHAIR). Read more at CHAIRcoalition.org
References:
1. https://www.sciencedirect.com/science/article/abs/pii/S0924224421003320
2. https://www.psychologytoday.com/ca/blog/machiavellians-gulling-the-rubes/202301/the-semmelweis-reflex-truth-is-hard-on-the-ears-0
3. https://www.epa.gov/sites/default/files/2020-10/documents/uvlight-complianceadvisory.pdf
4. https://gazette.gc.ca/rp-pr/p2/2022/2022-05-25/html/sor-dors99-eng.html Note: Canadian Registration content is currently under review in 2023/24
5. https://www.ashrae.org/file%20library/professional%20development/tech%20hour/tech-hour-ppt_stephanie-taylor_november-2019.pdf
6. https://www.ashrae.org/file%20library/professional%20development/tech%20hour/tech-hour-ppt_stephanie-taylor_november-2019.pdf
7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5432778
8. https://www.epa.gov/newsreleases/epa-registers-copper-surfaces-residual-use-against-coronavirus
9. https://www.canada.ca/en/health-canada/services/consumer-product-safety/reports-publications/pesticides-pest-management/decisions-updates/registration-decision/2014/metallic-copper-rd2014-15.html
Healthcare Sinks as a Source of Pathogens and a Potential Solution
By Richard Dixon and David Koenig, PhD
This article originally appeared in the September 2023 issue of Healthcare Hygiene magazine.
Authors’ note: The purpose of this document is to stimulate a discussion on an innovative new concept to clean and disinfect healthcare sink drains that are a common source of pathogens. It is not intended to claim any outcomes.
Antimicrobial resistance (AMR) is among the World Health Organization (WHO)’s top 10 threats for global health. The rise of AMR was initially driven by the misuse of antimicrobials in livestock, crops, and humans. The rise in AMR microbes has reduced or eliminated the effectiveness of many antibiotics used to treat infections such there are limited alternatives. Lack of treatment is predicted to lead to a tenfold increase in AMR associated deaths by 2050. AMR microbes and associated health impacts are expected to become burden on the global economy leading to a rise in poverty.
Prevention is at the core for stopping AMR emergence. It is well known that the environment plays a key role in the development and transmission of AMR microbes. Conversely, the environment is a key area for active prevention of AMR. In the hospitals, the sink has been shown to contribute to the rise of AMR. Not only is the sink a source of hospital-acquired infections (HAIs) but is also a source for dispersal of AMR microbes into the community. Therefore, eliminating the sink as a source of HAIs and AMR microbes will greatly help in the quest for controlling AMR globally.
Sinks and Drains
Researchers all over the world have been investigating sinks and drains as a source of HAI microorganisms, especially carbapenem-resistant Enterobacteriaceae (CRE). CRE infections are of particular concern because of their ability to transfer their AMR genetic elements from one bacterial species to another, for example from carbapenem-resistant Klebsiella pneumoniae to Escherichia coli. In 2000, a paper in Current Opinions in Microbiology posed the question, “Is the emergence of carbapenemase a problem waiting to happen?” Almost 20 years on, the problem is here.
Reports that suspected sinks and drains could be the source of CRE that caused HAIs began to emerge in 2003. In a 2017 review, The Hospital Water Environment as a Reservoir for CRE Causing Hospital-Acquired Infections, 17 studies identified sinks as a potential source of microorganisms causing HAI outbreaks, often in the Intensive Care Unit (ICU). Additionally, AMR microbes can colonize sinks and associated plumbing allowing for the transmission of AMR genes to non-AMR microbes, increasing the AMR problem exponentially. In that the waste stream from a sink ultimately reaches the municipal wastewater facilities, AMR microbes and other pathogens can be released into the community.

Figure 1: Carbapenem-Resistant Enterobacteriaceae (CRE). Courtesy of NIAID
Sink design directly drives the environmental conditions that favor microbial growth on plumbing line surfaces and ultimately favor AMR development. To prevent sewer gases being released into the room, sinks use water traps. These traps were first invented by Alexander Cumming in 1775, the S-bend trap. Eventually, P-trap (Figure 2) design was adopted that added a 90-degree fitting on the outlet side of a U-bend. The P-trap was popularized by Thomas Crapper in the 1880s and remains in use today. By design the P-trap allows for the sink lines to remain wet, but as was probably underappreciated in 1880 these conditions allow for the rapid growth of biofilms that will harbor pathogens and AMR microbes.

Figure 2: A P-trap.
AMR microbes can spread along waste lines connecting sinks and colonize the P-trap. Once there, they form a biofilm which can grow upwards to reach the sink strainer at a rate of up to 2.5 cm a day. When the water from the faucet hits the sink strainer there is splashing that carries pathogens (HAI) and AMR microbes in droplets onto surrounding counters and the floor up to 1 meter away. Patient-care and personal items left around the sink can become contaminated, increasing the chance of transmission of pathogens to patients. Additionally, superbugs contained in sink biofilms can be flushed out of the sink into the municipal water treatment system contaminating the outside world, leading to community AMR infections. Sink design has been virtually unchanged for more than 140 years, going back to the days of Alexander Cumming and Thomas Crapper. It is time to change this plumbing.
To date, healthcare facilities have tried a wide range of interventions to stop outbreaks associated with sinks. A few of these are listed here:
• Replacing the entire contaminated sink or replacing the downpipes and p-traps.
o Still using the Crapper design, problem reoccurs soon after replacement.
• Correct defective conditions in water systems such as dead ends, low water use areas, temperature, and pressure fluctuations.
o Helpful in simplifying water flow but the P-trap is still there, maintaining the primary driver for biofilm development.
• Placement of an offset sink drain in hand hygiene sinks.
o Will reduce splashing from the sink strainer.
o P-trap is still in place allowing for biofilm growth.
• Changing to deeper sink basins to prevent cross-contamination of hands and adjacent surfaces.
o Does not eliminate splashing or biofilm growth.
• Regularly pouring disinfectants such as sodium hypochlorite, hypochlorous acid, hydrogen peroxide, acetic acid, octanoic acid, or peroxyacetic acid down sink
o Significantly decreases bioburden, but regrowth happens within a few days.
• Blocking the drain line and allowing the disinfectant to sit in the P-trap.
o More successful than just pouring disinfectant down drain.
o Regrowth will still occur.
• A device that heats and/or subjects the downpipe to ultrasound to kill and remove the biofilm.
o There will be biofilm regrowth after treatment.
o Units require a power source near the sink.
• Unit on sink that generates ozonated water via the faucet to disinfect the P-trap and drain at each use.
o Shown to be effective at decreasing Pseudomonas aeruginosa and Candida auris contamination.
o Due to rapid decomposition of ozone, water left to sit for long period of time in P-trap will become contaminated and form biofilms.
o Units require a power source near the sink.
o Ozone generators require engineering controls to ensure no release of ozone into occupied spaces.
It seems clear that there is no silver bullet that will eliminate the risk of pathogen (HAI), and particularly CRE transmission (AMR microbes) due to ancient design of sink P-traps and drains. Some interventions resulted in the end of outbreaks but didn’t fully eliminate CRE from the P-trap or drain and the potential of a CRE infection occurring. Others were not successful at eliminating the outbreak at all. We therefore propose a very different plumbing configuration to address sink biofilms and splash transmission of HAI and AMR microbes to the hospital-built environment.
EasyFlow Concept
All the interventions to date have missed the obvious, the ancient P-traps drain design is the key to biofilm development. Thus, the necessity of the immense problem lies in a new radical approach to the design called EasyFlow (Figure 3). This design eliminates the P-trap. The P-trap encourages biofilm growth by simply providing the water needed to build luxurious biofilms that will harbor AMR microbes and pathogens (HAIs) in conditions that are hard to treat and remove. The water in the P-trap furthermore provides the necessary water of activity (aw) conditions in the waste lines from the P-trap to the sink strainer allowing growth of biofilm on all surfaces. Ultimately providing the source of microbes to be splashed into the hospital-built environment. Removal of the P-trap allows for reducing the aw in the sink lines such that luxurious biofilms will not form, significantly reducing the risk of splashing microbes into the hospital-built environment.

Figure 3: EasyFlow concept, courtesy of the authors
The key to EasyFlow is eliminating the P-trap. To do this an offset sink drain line is routed straight down or at any angle equal or less then 45 degrees from the bottom of the sink. After which the drain line is routed 90o or less to the discharge line (Figure 3). Sewage odors are mitigated by installing a negative pressure fan on the vent pipe to pull the air gases continually out of the entire system. Negative pressure fans will have the ability to adapt flow rate to ensure appropriate operation in concert with room fluctuations of the heating, ventilation, and air conditioning (HVAC) systems air flow and pressures. All fans are connected via a low voltage control wire to the healthcare facility Building Automation System (BAS) so that if a fan fails, the engineering department can receive the failure signal and repair or replace the fan/motor immediately. A hatch is required for access by engineering. The advantage of this system is that unlike the “Crapper” design this system will substantially reduce the moisture in the waste system lines thereby minimizing dangerous wet biofilms. Dry biofilms are still expected to persist but will be treated using disinfectant applications.
A horizontal drain line will be installed at an applicable distance away from the sink or varying number of sinks on the front end of the drain system. These lines will have a closure gate or ball valve that can isolate the drain for short periods of time (Figure 3). This allows for completely filling the system with the appropriate disinfectant. The goal of this procedure is to remove any dry biofilm that may propagate in the waste lines. The valve should be placed such that there is an easy to locate access hatch that is appropriately marked as such. Conversely, a remote-control valve can be used to allow for energization of the circuit without manual interventions. It is also possible to install a remotely controlled ice plug device at the point required for fluid restriction as a redundant feature. It is also possible to use these valves to close off the drain line in the case of a negative pressure fan failure stopping sewer gas escaping into the room, during fan repair.
To ensure appropriate function of the system regular auditing of the drain lines via ATP tests, protein tests, or microbial culture are recommended to ensure there is no or very little dry biofilm in the section of the drain line closest to the sink(s). Remember a dead biofilm that is still on the surfaces will enhance the regrowth of new biofilm.
The advantage of the EasyFlow concept over the “Crapper” design is:
1. Proactive biofilm through engineered infection prevention
2. Continuous drying of waste drain lines
3. Efficient removal of dry biofilms
4. Redundancy
5. Process control monitors
6. Active reduction of AMR bacterial dispersal to the hospital-built environment and community
Summary
For 140 years the same design for sinks has been used that enhances the growth biofilms. These biofilms will harbor bacteria and fungi. The microbes in the biofilms will share genetic elements allowing for transfer of AMR between divergent species and enhance the growth of HAI microbes. Sink biofilms drive the transfer of HAI and AMR microbes into the hospital-built environment through splashing as well as dispersal into the community by release into the municipal waste stream.
The EasyFlow concept removes the P-trap greatly reducing the ability of biofilms to form by lowing the aw on the surfaces of associated sink and drain lines. This will reduce the ability of microbes to transfer AMR elements to others and eliminate the biofilm on the sink strainer abolishing dispersion of pathogens into the hospital-built environment. Ultimately enhancing the lives and wellbeing of both patients and care givers.
Richard Dixon is board member and co-founder of the Coalition for Community & Healthcare Acquired Infection Reduction (CHAIR); a Canadian Standards Association former standards writer: Vice-chair Infection Control During Construction, Renovations & Maintenance of Healthcare Facilities. chair, Cleaning and Disinfection of Health Care Facilities, Member Health Care Facilities (building new health care facilities), Special Requirements for Plumbing Installations in Health Care Facilities; and a research consultant for Vancouver Coastal Health (Environmental & Patient Care). He may be reached at: DixonConsulting@gmail.com or (226) 698-1768 (Canada) or (772) 269-6491 (U.S.)
David Koenig, PhD, is currently chief technology officer of DKMicrobios and a board member of the Environmental Services Optimization Playbook (EvSOP). He is formerly a research technical leader with Kimberly Clark Corporation (infection control, human microbiome, and skin health), as well as a former microbiologist for the NASA Johnson Space Center (ISS environmental and water subsystems, ISS Crew Health subsystem, Lunar/Mars Regenerative life support systems), and formerly a microbiologist for Betz Paperchem (biofilm control). He may be reached at: dkmicrobios@gmail.com or (920) 527-8243.
References:
Aranega-Bou, P., Cornbill, C., Verlander, N.Q. and Moore, G., 2021. A splash-reducing clinical handwash basin reduces droplet-mediated dispersal from a sink contaminated with Gram-negative bacteria in a laboratory model system. Journal of Hospital Infection, 114, pp.171-174.
Aranega-Bou, P., George, R.P., Verlander, N.Q., Paton, S., Bennett, A., Moore, G., Aiken, Z., Akinremi, O., Ali, A., Cawthorne, J. and Cleary, P., 2019. Carbapenem-resistant Enterobacteriaceae dispersal from sinks is linked to drain position and drainage rates in a laboratory model system. Journal of Hospital Infection, 102(1), pp.63-69.
Aspelund, A.S., Sjöström, K., Liljequist, B.O., Mörgelin, M., Melander, E. and Påhlman, L.I., 2016. Acetic acid as a decontamination method for sink drains in a nosocomial outbreak of metallo-β-lactamase-producing Pseudomonas aeruginosa. Journal of Hospital Infection, 94(1), pp.13-20.
Avaness, M., Salt, N., dit Mieusement, L.M., Marchand-Senecal, X. and Leis, J., 2020. Role of Sinks as an Environmental Reservoir in CPE Outbreak in a Burn Intensive Care Unit. American Journal of Infection Control, 48(8), p.S39.
Bandara, H.M.H.N. and Samaranayake, L.P., 2022. Emerging strategies for environmental decontamination of the nosocomial fungal pathogen Candida auris. Journal of Medical Microbiology, 71(6), p.001548.
Bert, F., Maubec, E., Bruneau, B., Berry, P. and Lambert-Zechovsky, N., 1998. Multi-resistant Pseudomonas aeruginosa outbreak associated with contaminated tap water in a neurosurgery intensive care unit. Journal of Hospital Infection, 39(1), pp.53-62.
Breathnach, A.S., Cubbon, M.D., Karunaharan, R.N., Pope, C.F. and Planche, T.D., 2012. Multidrug-resistant Pseudomonas aeruginosa outbreaks in two hospitals: association with contaminated hospital waste-water systems. Journal of Hospital Infection, 82(1), pp.19-24.
Buchan, B.W., Arvan, J.A., Graham, M.B., Tarima, S., Faron, M.L., Nanchal, R. and Munoz-Price, L.S., 2019. Effectiveness of a hydrogen peroxide foam against bleach for the disinfection of sink drains. Infection Control & Hospital Epidemiology, 40(6), pp.724-726.
Carling, P.C., 2018. Wastewater drains: epidemiology and interventions in 23 carbapenem-resistant organism outbreaks. Infection Control & Hospital Epidemiology, 39(8), pp.972-979.
Chan, A., Thure, K., Tobey, K., Shugart, A., Schmedes, S., Burks IV, J.A., Hardin, H., Moore, C., Carpenter, T., Brooks, S. and Gable, P., 2023, May. Containment of a Verona Integron-Encoded Metallo-Beta-Lactamase-Producing Pseudomonas aeruginosa Outbreak Associated With an Acute Care Hospital Sink—Tennessee, 2018–2020. In Open Forum Infectious Diseases (Vol. 10, No. 5, p. ofad194). US: Oxford University Press.
Cole, K. and Talmadge, J.E., 2019. Mitigation of microbial contamination from waste water and aerosolization by sink design. Journal of Hospital Infection, 103(2), pp.193-199.
De Geyter, D., Blommaert, L., Verbraeken, N., Sevenois, M., Huyghens, L., Martini, H., Covens, L., Piérard, D. and Wybo, I., 2017. The sink as a potential source of transmission of carbapenemase-producing Enterobacteriaceae in the intensive care unit. Antimicrobial Resistance & Infection Control, 6(1), pp.1-6.
De Jonge, E., De Boer, M.G.J., Van Essen, E.H.R., Dogterom-Ballering, H.C.M. and Veldkamp, K.E., 2019. Effects of a disinfection device on colonization of sink drains and patients during a prolonged outbreak of multidrug-resistant Pseudomonas aeruginosa in an intensive care unit. Journal of Hospital Infection, 102(1), pp.70-74.
Decraene, V., Phan, H.T.T., George, R., Wyllie, D.H., Akinremi, O., Aiken, Z., Cleary, P., Dodgson, A., Pankhurst, L., Crook, D.W. and Lenney, C., 2018. A large, refractory nosocomial outbreak of Klebsiella pneumoniae carbapenemase-producing Escherichia coli demonstrates carbapenemase gene outbreaks involving sink sites require novel approaches to infection control. Antimicrobial agents and chemotherapy, 62(12), pp.10-1128.
Diorio-Toth, L., Wallace, M.A., Farnsworth, C.W., Wang, B., Gul, D., Kwon, J.H., Andleeb, S., Burnham, C.A.D. and Dantas, G., 2023. Intensive care unit sinks are persistently colonized with multidrug resistant bacteria and mobilizable, resistance-conferring plasmids. Msystems, pp.e00206-23.
Franco, L.C., Tanner, W., Ganim, C., Davy, T., Edwards, J. and Donlan, R., 2020. A microbiological survey of handwashing sinks in the hospital built environment reveals differences in patient room and healthcare personnel sinks. Scientific Reports, 10(1), p.8234.
Fucini, G.B., Geffers, C., Schwab, F., Behnke, M., Sunder, W., Moellmann, J. and Gastmeier, P., 2023. Sinks in patient rooms in the ICU are associated with higher rates of hospital-acquired infections. A retrospective analysis of 552 ICUs. Journal of Hospital Infection.
Gettler, E., Smith, B.A. and Lewis, S.S., 2023. Challenges in the Hospital Water System and Innovations to Prevent Healthcare-Associated Infections. Current Treatment Options in Infectious Diseases, 15(1), pp.1-13.
Grabowski, M., Lobo, J.M., Gunnell, B., Enfield, K., Carpenter, R., Barnes, L. and Mathers, A.J., 2018. Characterizations of handwashing sink activities in a single hospital medical intensive care unit. Journal of Hospital Infection, 100(3), pp.e115-e122.
Heenan, E., Salter, M., Schweikert, C. and Schweikert II, M., 2022. Decreasing Pseudomonas aeruginosa Bioburden Via Once Weekly Disinfection of Hospital Sink Drains. International Journal of Infectious Diseases, 116, p.S85.
Hoque, S.N., Graham, J., Kaufmann, M.E. and Tabaqchali, S., 2001. Chryseobacterium (Flavobacterium) meningosepticum outbreak associated with colonization of water taps in a neonatal intensive care unit. Journal of Hospital Infection, 47(3), pp.188-192.
Inkster, T., Peters, C., Wafer, T., Holloway, D. and Makin, T., 2021. Investigation and control of an outbreak due to a contaminated hospital water system, identified following a rare case of Cupriavidus pauculus bacteraemia. Journal of Hospital Infection, 111, pp.53-64.
Jamal, A.J., Mataseje, L.F., Brown, K.A., Katz, K., Johnstone, J., Muller, M.P., Allen, V.G., Borgia, S., Boyd, D.A., Ciccotelli, W. and Delibasic, K., 2020. Carbapenemase-producing Enterobacterales in hospital drains in Southern Ontario, Canada. Journal of Hospital Infection, 106(4), pp.820-827.
Jung, J., Choi, H.S., Lee, J.Y., Ryu, S.H., Kim, S.K., Hong, M.J., Kwak, S.H., Kim, H.J., Lee, M.S., Sung, H. and Kim, M.N., 2020. Outbreak of carbapenemase-producing Enterobacteriaceae associated with a contaminated water dispenser and sink drains in the cardiology units of a Korean hospital. Journal of Hospital Infection, 104(4), pp.476-483.
Kearney, A., Boyle, M.A., Curley, G.F. and Humphreys, H., 2021. Preventing infections caused by carbapenemase-producing bacteria in the intensive care unit-Think about the sink. Journal of Critical Care, 66, pp.52-59.
Kotay, S.M., Donlan, R.M., Ganim, C., Barry, K., Christensen, B.E. and Mathers, A.J., 2019. Droplet-rather than aerosol-mediated dispersion is the primary mechanism of bacterial transmission from contaminated hand-washing sink traps. Applied and environmental microbiology, 85(2), pp.e01997-18.
Kotay, S.M., Parikh, H.I., Barry, K., Gweon, H.S., Guilford, W., Carroll, J. and Mathers, A.J., 2020. Nutrients influence the dynamics of Klebsiella pneumoniae carbapenemase producing enterobacterales in transplanted hospital sinks. Water Research, 176, p.115707.
Kumar, J., Eilertson, B., Cadnum, J.L., Whitlow, C.S., Jencson, A.L., Safdar, N., Krein, S.L., Tanner, W.D., Mayer, J., Samore, M.H. and Donskey, C.J., 2019. Environmental contamination with Candida species in multiple hospitals including a tertiary care hospital with a Candida auris outbreak. Pathogens and Immunity, 4(2), p.260.
Lalancette, C., Charron, D., Laferrière, C., Dolcé, P., Déziel, E., Prévost, M. and Bédard, E., 2017. Hospital drains as reservoirs of Pseudomonas aeruginosa: multiple-locus variable-number of tandem repeats analysis genotypes recovered from faucets, sink surfaces and patients. Pathogens, 6(3), p.36.
Leitner, E., Zarfel, G., Luxner, J., Herzog, K., Pekard-Amenitsch, S., Hoenigl, M., Valentin, T., Feierl, G., Grisold, A.J., Högenauer, C. and Sill, H., 2015. Contaminated handwashing sinks as the source of a clonal outbreak of KPC-2-producing Klebsiella oxytoca on a hematology ward. Antimicrobial agents and chemotherapy, 59(1), pp.714-716.
LemariÚ, C., Legeay, C., Mahieu, R., Moal, F., Ramont, C., Kouatchet, A. and Eveillard, M., 2021. Long-term contamination of sink drains by carbapenemase-producing Enterobacterales in three intensive care units: characteristics and transmission to patients. Journal of Hospital Infection, 112, pp.16-20.
Lowe, C., Willey, B., O’Shaughnessy, A., Lee, W., Lum, M., Pike, K., Larocque, C., Dedier, H., Dales, L., Moore, C. and McGeer, A., 2012. Outbreak of extended-spectrum β-lactamase–producing Klebsiella oxytoca infections associated with contaminated handwashing sinks. Emerging infectious diseases, 18(8), p.1242.
Lucero, C.A., Cohen, A.L., Trevino, I., Rupp, A.H., Harris, M., Forkan-Kelly, S., Noble-Wang, J., Jensen, B., Shams, A., Arduino, M.J. and LiPuma, J.J., 2011. Outbreak of Burkholderia cepacia complex among ventilated pediatric patients linked to hospital sinks. American journal of infection control, 39(9), pp.775-778.
Matheu, M.M., Rice, N., Singson, K., John, B.S., Lindsay, H., Burnett, K., Coombs, J., Fernley, T. and Lopansri, B.K., 2022, December. 1221. Stenotrophomonas maltophilia Outbreak Associated with Sink Drains in an Intensive Care Unit. In Open Forum Infectious Diseases (Vol. 9, No. Supplement_2, pp. ofac492-1053). US: Oxford University Press.
Okomo, U., Senghore, M., Darboe, S., Bojang, E., Zaman, S.M., Hossain, M.J., Nwakanma, D., Le Doare, K., Holt, K.E., Hos, N.J. and Lawn, J.E., 2020. Investigation of sequential outbreaks of Burkholderia cepacia and multidrug-resistant extended spectrum β-lactamase producing Klebsiella species in a West African tertiary hospital neonatal unit: a retrospective genomic analysis. The Lancet Microbe, 1(3), pp.e119-e129.
Parkes, L.O. and Hota, S.S., 2018. Sink-related outbreaks and mitigation strategies in healthcare facilities. Current infectious disease reports, 20, pp.1-14.
Regev-Yochay, G., Smollan, G., Tal, I., Zade, N.P., Haviv, Y., Nudelman, V., Gal-Mor, O., Jaber, H., Zimlichman, E., Keller, N. and Rahav, G., 2018. Sink traps as the source of transmission of OXA-48–producing Serratia marcescens in an intensive care unit. Infection Control & Hospital Epidemiology, 39(11), pp.1307-1315.
Schärer, V., Meier, M.T., Schuepbach, R.A., Zinkernagel, A.S., Boumasmoud, M., Chakrakodi, B., Brugger, S.D., Fröhlich, M.R., Wolfensberger, A., Sax, H. and Kuster, S.P., 2023. An intensive care unit outbreak with multidrug-resistant Pseudomonas aeruginosa–spot on sinks. Journal of Hospital Infection.
Shaw, E., Gavaldà, L., Càmara, J., Gasull, R., Gallego, S., Tubau, F., Granada, R.M., Ciercoles, P., Dominguez, M.A., Manez, R. and Carratalà, J., 2018. Control of endemic multidrug-resistant Gram-negative bacteria after removal of sinks and implementing a new water-safe policy in an intensive care unit. Journal of Hospital Infection, 98(3), pp.275-281.
Starlander, G. and Melhus, Å., 2012. Minor outbreak of extended-spectrum β-lactamase-producing Klebsiella pneumoniae in an intensive care unit due to a contaminated sink. Journal of hospital infection, 82(2), pp.122-124.
Stribling, W., Hall, L.R., Powell, A., Harless, C., Martin, M.J., Corey, B.W., Snesrud, E., Ong, A., Maybank, R., Stam, J. and Bartlett, K., 2023. Evolution and spread of a persistent P. aeruginosa outbreak clone over decades in a single US hospital. bioRxiv, pp.2023-07.
Teoh, Z., Ankrum, A.L., Meinzen-Derr, J., Weingartner, M., Goebel, M.J., Huang, F.S. and Schaffzin, J.K., 2022. An outbreak of Burkholderia contaminans at a quaternary children’s hospital linked to equipment reprocessing. Infection Control & Hospital Epidemiology, pp.1-7.
Turner, C., Mosby, D., Partridge, D., Mason, C. and Parsons, H., 2020. A patient sink tap facilitating carbapenemase-producing enterobacterales transmission. Journal of Hospital Infection, 104(4), pp.511-512.
Umemura, T., Mutoh, Y., Sukawa, M., Hioki, T., Sakanashi, D., Kato, H., Hagihara, M., Yamada, T., Ikeda, Y., Mikamo, H. and Ichihara, T., 2023. Diminishment of Carbapenemase-Producing Enterobacterales from Sink Outlets Using a Steam Cleaner. Hygiene, 3(1), pp.13-17.
UN Environment Programme. 2023. Antimicrobial resistance: a global threat. Antimicrobial resistance: a global threat | UNEP - UN Environment Programme
Valentin, A.S., Dos Santos, S., Goube, F., Gimenes, R., Decalonne, M., Mereghetti, L., Daniau, C., van der Mee-Marquet, N., Abdoush, H., Alfandari, S. and Allaire, A., 2021. A prospective multicentre surveillance study to investigate the risk associated with contaminated sinks in the intensive care unit. Clinical Microbiology and Infection, 27(9), pp.1347-e9.
van der Zwet, W.C., Nijsen, I.E.J., Jamin, C., van Alphen, L.B., von Wintersdorff, C.J.H., Demandt, A.M.P. and Savelkoul, P.H.M., 2022. Role of the environment in transmission of Gram-negative bacteria in two consecutive outbreaks in a haematology-oncology department. Infection Prevention in Practice, 4(2), p.100209.
Vanstokstraeten, R., Calafell, J.B., De Geyter, D., Muyldermans, A., Wybo, I., Pierard, D. and Demuyser, T., 2022. Preliminary data of high-throughput culture on sink drains reveals a possible link between the presence of Candida species and VIM-producing Pseudomonas aeruginosa in a Belgian tertiary care intensive care unit. In 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID).
Volling, C., Thomas, S., Johnstone, J., Maltezou, H.C., Mertz, D., Stuart, R., Jamal, A.J., Kandel, C., Ahangari, N., Coleman, B.L. and McGeer, A., 2020. Development of a tool to assess evidence for causality in studies implicating sink drains as a reservoir for hospital-acquired gammaproteobacterial infection. Journal of Hospital Infection, 106(3), pp.454-464.
Weinbren, M. and Inkster, T., 2021. The hospital-built environment: biofilm, biodiversity and bias. Journal of Hospital Infection, 111, pp.50-52.
Weinbren, M.J., 2020. Dissemination of antibiotic resistance and other healthcare waterborne pathogens. The price of poor design, construction, usage and maintenance of modern water/sanitation services. Journal of Hospital Infection, 105(3), pp.406-411.
WHO. 2021. Antimicrobial resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
Call to Action: A Team-Based HAI Response
By Richard Dixon
This article originally appeared in the July 2023 issue of Healthcare Hygiene magazine.
A good risk management question to ask in a healthcare facility is: Who is responsible for safety? The most likely response would be “everybody.” Great answer! What about: Who is responsible for reducing healthcare-acquired infections (HAIs)? Answers typically are infection prevention and control (IP&C), environmental services (EVS), or nurses and doctors. Let’s take a closer look at the clinical and environmental issues and answer this important question properly.
IP&C staff monitor antibiotic use, assist in the policies for EVS and chemical selection, monitor HAI statistics with a watchful eye on outbreaks, provide education on prevention on many typical issues, guide contractors through the difficult processes of renovations in the facility, product review and evaluation, manage HAI outbreaks and more.
EVS is clearly responsible for the cleaning and disinfection in most healthcare facilities, with daily attention to horizonal and vertical surfaces, and special attention to high-touch surfaces plus a variety of waste management and recycling functions, pest management, laundry, and a wide variety of other areas.
Specialized cleaning and disinfection also take place in the food service department (food preparation, storage, serving, waste management), and in facilities management (ducts, cooling towers, HVAC equipment, and more).
Medical device reprocessing plays an important role in the operating and procedure rooms, as cleaning, disinfection, and sterilization of the many pieces of equipment and instruments -- some of which are extremely difficult to achieve 100 percent efficacy, such as endoscopes.
Nurses do their best to clean up blood and other fluid spills in medical and surgical inpatient units plus in ambulatory departments like endoscopy units.
Laboratory personnel, especially microbiology staff, identify bacteria, virus and fungal pathogens with incredible accuracy and speed but seldom are involved in the outcomes and trends of the patients that these tests are concerning.
A healthcare facility is therefore a complex web of different departments within an environment of multi-factorial issues that inevitably causes HAIs.
Let’s take the example of a patient in an older-style double room. Patient A is recovering from a respiratory illness and patient B is recovering from an abdominal issue who will test positive two days later for Clostridioides difficile (C. diff) from an endoscopy procedure. In the meantime, Patient A starts off with a mild diarrhea, uses the ensuite bathroom with the door partly open, and to complicate this issue, the bathroom’s negative-pressure vent is hardly drawing in any air, so the flushing of the toilet results in a plume of air containing fecal particles with C. diff bacteria to be distributed to Patient A whose bed is adjacent to the bathroom door. In the meantime, EVS staff try to clean and disinfect the room and bathroom, although both patients have personal items on the sink, overbed and bedside tables, so those surfaces don’t get any attention – it’s the same with the bedside rails because both patients are sleeping or have frequent visitors. As you can see, a perfect circumstance for Patients A and B to both contract as HAI, with further potential transmission beyond that patient room.
So, you can see in this over-simplified example, that HAIs are multi-factorial, and a different approach is required by all the separate departments who reside in their own silos. Here is just a sampling of these multi-factorial issues:
• Patient acuity
• Hand hygiene practices and auditing with consideration of the Hawthorne Effect
• Antibiotic stewardship programs
• Clinical practices
• Fecal waste management
• Environmental cleaning and disinfection practices, plus education
• Patient and visitor education
• Visitor restrictions
• HAI statistics availability and future predictions
• Personal protective equipment (PPE)
• Auditing of routine and specialized practices
• Recognition of transmission routes and challenges
• Facility design
• Facility audit of positive and negative pressures, water temperatures
• Clinical glove use policy
• Training and education
• Budgets to maintain within only a focus on initial control, not long-term prevention, and risk adverse interventions.
The bottom line is that the typical healthcare system of silos does not function properly to the benefit of patient care. However, the first clue is that when an outbreak occurs, the entire group of departments gets together to work through the cause, effect, and resolution issues to a successful conclusion, and hopefully put into future processes of the lessons learned. Let’s then not miss the biggest learning opportunity of all. Teamwork among the silo partners resulted in a positive patient-care solution. Why would or should the silos be maintained as status quo?
A few answers would be “We have always done it that way” or “I don’t want to change the process as it would be too hard,” or “I don’t like change.” The best way may be to start with the concept of a patient care multi-disciplinary team (PC-MDT) taking full responsibility for the entire scope of processes on a patient-focused basis. Here are some suggestions on membership of the PC-MDT:
- Infection Prevention & Control
- Environmental Services
- Microbiology and/or Laboratory
- Food Services
- Facilities Management
- Quality & Risk Management
- Nursing (inpatient and outpatient)
- Administration
- Medical Device Reprocessing
- Infectious Disease Physicians/Epidemiologists
- Occupational Health & Safety
- Other stakeholders as required
Let’s also look at some of the initial tasks the PC-MDT can address in the short and long term:
- EVS is on the front lines of defense of HAIs and should be recognized for their heroic efforts with addition budget support for training and education
- HAI statistics (facility, community, regional, national, etc.)
- IP&C staff attend clinical rounds
- Policies and procedures blended for an integrated approach
- Key performance indicators of success
- IP&C also focuses on an ‘interventional’ focus via a learning and problem-solving approach
- Observational auditing (visual, marker, ATP, microbial culture) including when who, how, cost, etc. and use the outcome in trending analysis, celebrating success and learning
- Organizational audits of departments or significant multi-faceted processes
- Specialized audits targeting potential sources of transmission (sinks and drains)
- Chemical products (manufacturer’s use requirements, safety, fit for the desired outcome, PPE use, etc.)
- Terminal, shared equipment and specialized cleaning
- Engineered infection prevention solutions such as ultraviolet light, ozonated water hygiene sinks, self-sanitizing surfaces like copper alloys
- Patient, visitor, physician, and staff surveys
- Building trust and success, not fault or punitive measures
- Target typically higher rates of common HAIs (VRE, C. diff, MRSA, CPO), and be on the outlook for fungal infections (Candida auris, Aspergillosis) and more impacts of SARS-CoV-2 variants
- Collaborate with local healthcare facilities on regional learning and cooperation
- Attending professional conferences with a cross representation of attendance
- Seek out local, regional, national, and international standards relevant to the facility’s needs.
- Recommendations to administration on operational changes and capital equipment or facility changes that have a positive impact on patient care (Tip: while the upfront costs are very important, the real issue is what a proposed change can do to reduce HAIs, noted as a return on patient care investment and a strong perspective that HAIs cause illness and death) and financial issues for the facility
- Communication strategy to healthcare stakeholders
- Use science- and evidence-based decision-making
- Randomized clinical trials in environmental assessments do not do well in some multi-factorial HAI-related issues, but rather a practical approach of quantitative risk management assessment (QMRA) which has its roots in food services risk management and safety. This is about assessing the risk of transmission and developing changes to lessen the risk.
Did this whole discussion not start about who is responsible for safety? We are all responsible for HAIs and should dedicate our resources and trust in a PC-MDT to lead the way to safer environment for patients, staff, physicians, and visitors. Remember, the word “team” has four letters that can spelled also as mate; thus, we are all teammates.
Richard Dixon is the co-founder and a board member of the Coalition for Community & Healthcare Acquired Infection Reduction (CHAIR). He has 40 years of experience in senior administration, planning, design, construction, commissioning plus infection prevention and control in healthcare facilities in Canada and across the globe.
The Business Case for Hospitals to Expand Their CMS Reimbursement Potential
By John Scherberger, FAHE
This article originally appeared in the January 2023 issue of Healthcare Hygiene magazine.
Doing more with less – including lower reimbursement rates, fewer staff and smaller budgets – has become healthcare institutions’ new normal as the nation emerges from the pandemic while addressing continued challenges related to evolving patient populations, increased expectations around infection prevention, and the need for the C-suite to manage fiscal operations while meeting the IHI’s Triple Aim initiative of improving the patient experience of care (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare. Additionally, the implementation of the Patient Protection and Affordable Care Act and the Centers for Medicare and Medicaid Services (CMS)’ Hospital Value-Based Purchasing Program presents both challenges and opportunities.1
In the interim, the world experienced the effects of the SARS-CoV-2 pandemic. Millions died worldwide, shook national economies to their foundation, and hospitals experienced challenges for which they were unprepared. The U.S. government stepped forth with a double-edged sword to combat the pandemic and save lives. The success or failure of the efforts remains controversial. As never seen before, an infusion of federal funds was one edge of the sword.
Hospitals are now experiencing the effects of the other edge of the sword. With the declaration of the end of the COVID-19 pandemic, drastic cuts to federal funds took place, hospitals are facing 2022 ending with the worst financial results, and 2023 may not show an economic turn-around. The fatted calf was laid on the altar of economic expedience, and there is not another one waiting in the wings.
In May 2021, one healthcare industry news outlet2 shouted, "Post-COVID-19 era hospital revenues plummet." In September 2022, they proclaimed 2022 "the most financially difficult year for hospitals and health systems since the start of the pandemic."
Times have changed, things have changed, and operations must change.
With the financial disasters facing healthcare because of the pandemic, it is time for chief financial officers and Medicare billing departments, along with their Medicare administrative contractors, to broaden their approaches realistically, ethically, and financially to maximize their CMS reimbursement opportunities.
They must revisit their approach to the Medicare Provider Manual, Part 1, Chapter 21 (Rev. 454). Specifically, Chapter 102.2 Costs Related to Patient Care, Section 2135 Purchased Management and Administrative Support Services, subsection 2135.1 General, and 2135.2 Evaluation of the Need for Purchased Management and Administrative Support Services.
(https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Paper-Based-Manuals-Items/CMS021929) Then click on Chapter 21 -- Costs Related to Patient Care.
An additional source for information is https://portal.cms.gov/portal/
Allowability of costs is subject to the regulations prescribing the treatment of specific items under the Medicare program.
Long-term adjustments, not knee-jerk reactions, must occur. Hospitals must recognize a paradigm shift for doing business, a new method (a late Middle English word meaning, in a sense, “prescribed medical treatment for a disease.” Derived via Latin from the Greek “methodos” meaning a pursuit of knowledge, from meta- (expressing development) plus “hodos” meaning way.)
Environmental, Social and Governance (ESG)
Hospitals and hospital systems face a new challenge in this post-pandemic time -- environmental, social, and governance (ESG) programs. With the financial difficulties incumbent upon their survival, ESG is demanded of them. They can no longer give lip service to sustainability or "reduce, reuse, recycle" campaigns. Hospitals must look beyond the healthcare environment; they must seek to do what is best for the environment and community in which they live and serve.
For example, hospitals are the most significant contributors to their community landfills and have it within their power to reduce their negative ecological footprint. They must look at how to incorporate reusable, sustainable products and recognize that the disinfectants and chemicals they use to keep their facilities hygienic are also polluting their environment. The same disinfectants they use damage the surfaces of their healthcare environment – equipment, floors, surfaces, mattresses, and countless other valuable and costly possessions.
Most importantly, they are endangering the health of their staff and patients with antiquated disinfectants (pesticides). They needlessly contribute to putting tons of waste into landfills that will never decompose. Disposable isolation gowns and plastic containers that hold disinfectants now find new "forever homes" in landfills because they cannot recycle them. (https://www.epa.gov/pesticide-worker-safety/containers-containment-storage-and-disposal-pesticides). Billions (and still counting) of disposable, single-use wipes and wipers contaminated with disinfectants are populating landfills regardless of manufacturers' claims that they are "recyclable."
What does ESG have to do with possible CMS reimbursement? Disposable products are not "reimbursable" events but a direct expense to hospitals. Hospitals must reduce their direct costs effectively, efficiently, and in ecologically sound manners. Thinking outside the proverbial box with CMS as a partner will bring rewards. Why have hospitals been reticent to go outside of the box? Maybe because it has yet to be done.
With the implementation of the Patient Protection and Affordable Care Act, CMS Value-Based Purchasing, and the financial wreckage healthcare providers are facing, healthcare must understand that times have changed, things have changed, and operations must change. The CMS Roadmap for Implementing Value Driven Healthcare in the Traditional Medicare Fee-for-Service Program opens with the following paragraph: "Given that CMS policies have a transformative impact on the healthcare system, it is important to develop the tools necessary to create rational approaches to lessen healthcare cost growth and to identify and encourage care delivery patterns that are not only high quality but also cost-efficient."
Healthcare facilities must go beyond using the best and most appropriate DRG to apply to a procedure to capture the highest reimbursement, participating in group purchasing organizations (GPOs), or utilizing just-in-time inventory. They must "develop the tools necessary to create rational approaches to lessen healthcare cost growth and to identify and encourage care delivery patterns that are both high quality and cost-efficient."
To quote Thomas Pynchon: "If they can get you asking the wrong questions, they don't have to worry about answers."
John Scherberger, FAHE, is principal of Healthcare Risk Mitigation.
References:
1. Scherberger J. The Case for Moving Infection Prevention Textiles to the Linen/Laundry Department. Infect Control Today. Sept. 9, 2019. Accessible at: https://www.infectioncontroltoday.com/view/case-moving-infection-prevention-textiles-linenlaundry-department
2. Becker's Hospital CFO Report. Post-COVID-19 Era Hospital Revenues Plummet. May 31, 2022,.
3. Becker's Hospital CFO Report. Sept. 16, 2022.
Three New Studies Evaluate the Impact of Environmental Hygiene Strategies on HAI Reduction
By Linda Homan, RN, BSN, CIC
This article originally appeared in the September 2022 issue of Healthcare Hygiene magazine.
In today’s environment of limited budget and staffing resources for environmental hygiene, it is more important than ever to weigh the evidence before investing in a product, process or technology. Evaluating the clinical impact of environmental cleaning and disinfection products, processes and technologies remains challenging.
In 2013, leaders at the Division of Healthcare Quality Promotion of the Centers for Disease Control and Prevention (CDC) published an article that outlined the hierarchy of evidence needed to advance the science of environmental hygiene and improve patient safety.1 The hierarchy of study design for increasing patient safety through healthcare environmental surface cleaning and disinfection, listed from lowest to highest strength of evidence is as follows:
I. Laboratory demonstration of bioburden reduction efficacy (103-106 log reductions depending on the claims).
• Data that must be submitted to the Environmental Protection Agency (EPA) to prove efficacy of a product.
II. Demonstrate in-use bioburden reduction.
• Evidence that use of a product, process or technology reduces bioburden on surfaces in a clinical setting.
III. Demonstrate that in-use bioburden reduction may be clinically relevant.
• Terminal-only use: Reduction of same room transmission
• Terminal and daily use: Reduction of hand contamination
IV. Demonstrate reduced pathogen transmission via admission-discharge active surveillance testing or clinical incidence.
• Evidence that patients do not become colonized with pathogens during their healthcare stay.
V. Demonstrate reduced infections.
• Evidence that the product, process or technology reduces patient infections - the ultimate goal of environmental hygiene.
The authors point out that, for studies to reach the rigor required for levels III-V, careful attention must be paid to baseline infection rates, trends, patient population and sample size. Level III-V studies must also control for other key infection prevention interventions such as hand hygiene, source control/isolation practices, device/procedure-specific interventions and antibiotic use, as these variables can influence the patient outcome.
In the past decade, the body of evidence supporting the role of environmental hygiene in infection prevention has grown significantly. However, the most important evidence (Level V) demonstrating that a product, process or technology decreases healthcare-associated infections (HAI), has been slower in coming. This is at least in part due to the rigor that is required to measure this outcome.
Three recent studies evaluated the efficacy of different environmental hygiene strategies on HAI reduction – 1) monitoring and feedback of environmental cleaning using a made-for-purpose fluorescent marker, 2) implementing a comprehensive environmental hygiene program, and 3) the use of UV-C disinfection upon patient discharge or transfer.
Read on to find out which of these interventions were found to decrease HAIs and which were not.
Optimized Process: Environmental Hygiene Monitoring and Feedback
The CDC, as well as professional associations such as the Association for the Healthcare Environment (AHE), the Association of perioperative Registered Nurses (AORN), and the Association for Professionals in Infection Control and Epidemiology (APIC), recommend the use of an objective environmental hygiene monitoring method, along with direct observation, to ensure that high-touch objects are consistently and thoroughly cleaned.
A new study published in July 2022 reports on 10 years of retrospective data on the impact of a monitoring and feedback program using a made-for-purpose fluorescent marker to improve the thoroughness of cleaning in multiple hospital units.2 The author found that the use of a fluorescent marker improved and ultimately sustained thoroughness of cleaning over the course of a decade. The initiative started with patient room discharge cleaning and expanded into operating room, cardiac cath lab, labor and delivery and endoscopy suites over time. Over time, and with consistent effort, thoroughness of cleaning improved to meet target goals and was sustained over several years. A key strategy was the use of nurse liaisons who, along with other infection prevention initiatives, were trained to conduct environmental hygiene monitoring and provide feedback to environmental services (EVS) staff and leadership. The value of this approach was reinforced as they found that, during periods when EVS was self-monitoring, the cleaning results were falsely higher than cleaning scores as validated by an objective third party.
Most importantly, the author reported that improvements in cleaning and disinfecting performance throughout the hospital over a 10-year period were associated with infection reduction: A 75 percent overall reduction in HAI rates, including a 55 percent reduction in surgical site infection rates and a 70 percent reduction in hospital-acquired C. difficile infection rates. As mentioned above, for a Level V study, controlling for variables that may impact the infection rates is important. This study was conducted retrospectively, measuring real-world implementation of a quality improvement program. It did not control for baseline infection rates, trends, patient population and sample size or variables such as other infection prevention initiatives that may have impacted the results over the 10-year time span. Such is the nature of measuring any infection prevention strategy, especially over a long period of time – it is hard to tease out the independent impact of one initiative when we often implement multiple strategies at the same time to ensure the best patient outcome. In the case of this study, the 10-year length of the study adds strength to the findings.
Optimized Product AND Process
In June, 2022, a multi-center, controlled study measuring the impact of an optimized environmental hygiene program on hospital-onset C. difficile was published.3 In this study, eight hospitals that had implemented a program to improve environmental cleaning measured their C. difficile infection rates before and after implementation of the program. The program consisted of daily cleaning with a hydrogen peroxide/peroxyacetic acid sporicidal disinfectant, training on a standardized, evidence-based process, monitoring and feedback on thoroughness of cleaning with a made-for-purpose fluorescent gel marker, and actionable data to drive improvement via a digital dashboard. Thoroughness of cleaning was improved and sustained over the 18 months following implementation of the program. The result was a sustained 50 percent decrease in HO-CDIs in the hospitals that implemented the program versus control hospitals that had not implemented the program. This study met the rigor needed for a Level V study, thus demonstrating that the intervention reduced infections. To do this, the researchers addressed the following variables and confounders that can impact patient outcomes.
• They addressed baseline infection rates and trends. The intervention site patient acuity was stable over 39 months. The endemic HO-CDI SIRs before the intervention were stable.
• They included hospital controls. They compared the C. difficile infection rates in the intervention hospitals to rates in hospitals in the same hospital system that had not implemented the program and found that CDI rates did not decline as much in the hospitals that had not implemented the program.
• They controlled for other key infection prevention interventions. They surveyed infection preventionists from the eight intervention hospitals and found that other hospital-level factors that could have driven lower C. difficile rates showed no identifiable changes between the pre-intervention and post-intervention periods that would have impacted the outcome.
• Lastly, the researchers utilized a “removed treatment design” to show that a nonequivalent dependent variable of catheter-associated urinary tract infection (an HAI for which the environment does not play a key role in infection transmission) did not change during the intervention period in intervention hospitals whereas the HO-CDI rate declined.
UV-C disinfection as an adjunct to standard cleaning and disinfection
In the past decade, as hospitals look for ways to further improve environmental hygiene, decrease HAIs and instill confidence in patients that the hospital environment is as clean as possible, ultraviolet light technology has been introduced into the workflow to augment standard cleaning and disinfection practices upon patient discharge or transfer. Although UV-C technologies have shown microbicidal efficacy in laboratory studies, assessment of their effectiveness and ability to augment physical cleaning and disinfection in the clinical setting has been challenging. Well-designed, independent, controlled, comparative studies are needed to objectively quantify the cost and potential added value of such technologies when routine cleaning and disinfection has been optimized.4
A new multi-center study evaluated the effectiveness of ultraviolet-C (UV-C) disinfection as an adjunct to standard chlorine-based disinfection for terminal room cleaning in the reduction of multidrug-resistant organisms -- MRSA, VRE, CRE, ESBL and C. difficile.5 They compared acquisition of these five pathogens between patients exposed to them in rooms that had been terminally cleaned with chlorine-based disinfectant versus patients who had been exposed in rooms that had been terminally cleaned with chlorine-based disinfectant plus UV-C disinfection. The authors found that that adjunct UV-C disinfection did not provide incremental value in reducing transfer of MDRO above and beyond standard cleaning and disinfection. They concluded that “our analysis does not support the use of UV-C in addition to post-discharge cleaning with chlorine-based disinfectant to lower risk of prior occupant pathogen transfer.” This study meets the criteria for a Level IV study. It demonstrates reduced pathogen transmission via admission-discharge active surveillance testing or clinical incidence.
Reduction of HAIs is the goal of all environmental hygiene strategies, and the CDC has outlined the hierarchy of evidence needed to demonstrate the impact of a product, process or technology on HAI reduction. The level of scientific rigor required to demonstrate a clear connection between a strategy and HAI reduction is considerable and there are relatively few studies that have met this criteria to date. In today’s environment of limited resources for environmental hygiene, it is more important than ever to weigh the evidence before investing in a product, process or technology. The three recently published studies discussed here provide important insights into the clinical impact of environmental cleaning and disinfection products, processes and technologies to help EVS leaders make informed decisions on where to focus limited resources.
Linda Homan, RN, BSN, CIC, is director of clinical affairs for Ecolab Healthcare.
References:
1. McDonald LC and Arduino M. Climbing the Evidentiary Hierarchy for Environmental Infection Control. Clin Infect Dis. 2013;56(1):36-9. DOI: 10.1093/cid/cis845
2. Parry MF, et al. (2022). Environmental cleaning and disinfection: Sustaining changed practice and improving quality in the community hospital. Antimicrobial Stewardship & Healthcare Epidemiology. 2022;2(e113):1-7. https://doi.org/10.1017/ash.2022.257
3. Carling PC, et al. (2022). Mitigating hospital-onset Clostridioides difficile: The impact of an optimized environmental hygiene program in eight hospitals. Infect Control & Hosp Epidemiol. 2022 Jun 20:1-7 https://doi.org/10.1017/ice.2022.84
4. Carling PC. Health Care Environmental Hygiene: New Insights and Centers for Disease Control and Prevention Guidance. Infect Dis Clin N Am. 2021;35:609–629. https://doi.org/10.1016/j.idc.2021.04.005
5. Hodges JC, et al. (2022). Assessment of the effectiveness of ultraviolet C disinfection on transmission of hospital-acquired pathogens from prior room occupants. Antimicrobial Stewardship & Healthcare Epidemiology. 2022;2(e110):1-5. https://doi.org/10.1017/ash.2022.254
Leverage Principles of Adult Learning, Individual Learning Styles and Online Learning to Optimize Training on Environmental Hygiene in the OR
By Linda Homan, RN, BSN, CIC
This column originally appeared in the March 2022 issue of Healthcare Hygiene magazine.
Training staff on environmental hygiene in the operating room has always been important and challenging. And the staff turnover brought on by COVID-19 makes this challenging task even more difficult. You may be dealing with record-high staffing shortages even as surgical volume increases, creating a constant need for on-boarding and refresher training.
This is a good time to ensure that your training is effective. There is an entire educational discipline dedicated to the principles of adult learning. Regardless of whether you are training clinicians or environmental services staff on environmental hygiene in the operating room, it pays to be aware of these principles, along with individual learning styles.
MS Knowles, a leading expert in adult education, outlined the following principles of adult learning.1
Adult learners want to know why they should learn
We are more likely to put time and energy into learning if we know why it’s important. Make sure those that clean operating rooms understand the critical role they play in preventing patient infections. We also learn better if we understand the costs of not learning. “What’s in it for me?” Be sure to emphasize that learning this information will make their work easier and faster and that they will be recognized for completing the work well.
Adults need to take responsibility
Adults assume they oversee their own behavior and can make their own decisions. We expect to be treated as capable of taking on responsibility. However, once we enter a classroom, we may revert to their experience in school, where we were passive learners. To prevent this from happening, develop training methods that are outside the usual classroom passive learning setting. Online learning is a good example of this. It enables learners to take responsibility for their own learning.
Adults bring life experience to learning
For better or worse, adults come to the table with a wealth of personal experience and knowledge. Respect and value our experience but know how it tempers our learning. On the negative side, experience can lead to bias and presumption -- “I already know how to do this.” On the positive side, information learned earlier can be adapted to new situations. For instance, for a new employee who has experience in environmental services in the hospitality industry, compare the purpose and methods in that setting to those in the operating room.
Adults want to learn when the need arises
Adults learn best when it is their choice. Know that some learners might not want to be there, while others are ready to learn. To the extent possible, allow choice and self-directed learning. Again, this can be accomplished with online, self-directed learning.
Adults are task-oriented
We want our learning to be practical and problem-centered – a means to an end. Keep training focused on the tasks that are needed to do the work.
In addition to the differences between child and adult learners, each individual has a preferred learning style that is either visual, auditory, or kinesthetic. There are different ways of effectively teaching for each of these styles. Think about your own learning style as you read through these!
Visual learners learn by seeing. They like visual stimuli and picture themselves doing the task in their “mind’s eye.” In a classroom setting this may look like they are into staring off into the distance. They may drift away when extensive listening is required. These learners need something to watch. Use visual aids like video clips and graphics to supplement text in online learning. For in person learning use demonstrations, slides, and flipcharts.
Auditory learners learn by listening. They learn by listening to audio and can repeat and follow verbal instructions. They also like to talk so they enjoy dialogues and music. To teach auditory learners, tell them what they are going to learn, teach them, then tell them what they have learned. Include auditory activities such as listening to stories or playing verbal games. In online learning, include voice-over as an option.
Kinesthetic learners learn by doing. They learn better when they can move and manipulate things. They will learn best from hands on experience. In a classroom setting, keep them engaged by using activities like return demonstration (see one, do one, teach one) and role play. In online learning, use gamification.
Everyone uses all three styles of learning, so try to incorporate variety in your training methods to keep people engaged.
Leveraging the principles of adult learning and individual learning styles will make your training more effective. Effective training provides a huge return on investment through increased patient safety, staff engagement and retention, regulatory compliance, and sustainable performance improvement.
You don’t need to do this alone. Good vendor partners will provide training that incorporates the principles of adult learning and individual learning styles, are delivered digitally, in multiple languages, and on any connected device. Look for vendor training modules that have built-in mechanisms to assess knowledge and document competence. Now more than ever, we need ways to provide quality training and education that can be delivered “just in time, just in place, just enough, and just for me.”
Linda Homan, RN, BSN, CIC, is senior manager of clinical affairs for Ecolab.
Reference:
1. Craig RL, ed. The ASTD Training and Development Handbook: a Guide to Human Resource Development. New York: McGraw-Hill, 1996.
COVID-19 is Driving Practice Changes: Seize the Opportunity to Evaluate Which Changes Keep and Which to Toss Post-Pandemic
By Linda Homan, RN, BSN, CIC
Editor's note: This column originally appeared in the December 2021 issue of Healthcare Hygiene magazine.
A disastrous event like a pandemic causes practice changes, some based on evidence, and some based on ignorance or fear of the unknown. In our personal lives, some of us started carrying personal-sized hand sanitizer and practicing physical distancing. These evidence-based practices would be good to continue post-pandemic, as they can help prevent transmission of a host of infections, including colds and influenza. Some folks started washing their groceries and leaving packages outside for days to kill SARS-CoV-2. These are examples of practices borne out of ignorance. Now that we know more about the virus that causes COVID and how unlikely it is to be transmitted on our groceries or packages, these are practices that should be tossed. As we continue to manage through the pandemic, there is an opportunity to critically evaluate changes we’ve made in environmental hygiene practice. Here are some learnings and practices that we should consider keeping, as their value extends beyond the pandemic.
Environmental hygiene is infection prevention
In an article published in the Annals of Internal Medicine, environmental services workers were described as “unsung heroes, the critical first line of defense against infection” and “the unnoticed sinew of a well-functioning hospital.”1 If nothing else good comes of the pandemic, it has demonstrated the importance of environmental hygiene and the environmental services (EVS) team in infection prevention. Suddenly, in addition to being an integral part of day-to-day infection prevention by disinfecting patient rooms and procedure areas, EVS has been asked to disinfect more spaces, in more ways than ever before. Other departments such as physical therapy and nutrition may have requested increased environmental hygiene. It requires critical thinking and evaluation of the evidence to decide what really needs to be done, and how best to accomplish it.
There is reason to believe that increased cleaning and disinfection in areas outside of patient rooms is a practice worth keeping. A recent study demonstrated that high-touch objects in areas such as procedure rooms, waiting rooms, and clinics are contaminated with pathogens that can cause HAIs.2 The researchers cultured high-touch surfaces in radiology, physical therapy, emergency departments, waiting rooms, clinics, and endoscopy centers across four hospitals, four outpatient clinics, and one surgery center and found that 9.4 percent of cultured surfaces were positive for at least one bacterial pathogen.
Key Learnings: As the pandemic shines a light on the importance of environmental hygiene and environmental services, it’s time to recognize and embrace the critical role they play in infection prevention and incorporate EVS into the safety culture of the hospital. We should continue or perhaps even increase our focus on cleaning and disinfection in areas beyond patient rooms and procedure areas.
Be a healthy skeptic
As COVID spread, suddenly everyone thought they were environmental hygiene experts and had an opinion on how cleaning and disinfection should be done. New technology was suggested for you to use, and sometimes there was minimal data available to evaluate the technology. The drive to clean larger surface areas caused some to look at technology that hadn’t been considered before. You may have been asked about fogging, misting, spraying, or pesticidal devices such as UV lights, ozone generators, or air purifiers. Perhaps you developed a new appreciation for EPA’s Emerging Viral Pathogen Claims and List N. In these situations, it’s important to be a healthy skeptic. Carefully evaluate new chemistry or new ways of applying familiar chemistry and technology to make sure you are using it in a way that is supported by its claims. Refer to EPA’s Antimicrobial Products Registered with EPA Claims Against Common Pathogens https://www.epa.gov/pesticide-registration/selected-epa-registered-disinfectants
Key Learning: Evaluate new chemistry and technology based on its safety, effectiveness and fit into the workflow before incorporating it into your day-to-day operations post-pandemic.
Expect to be flexible
This is a new-to-the-world virus, so new guidelines were developed to address it, and then the guidelines evolved quickly as our knowledge of the virus grew. This required frequent practice changes and was a source of frustration for many. But the truth is, science is defined as “knowledge about or study of the natural world based on facts learned through experiments and observation.”3 As we learned more about COVID through experiments and observation, we quickly adjusted practice accordingly. Change in practice based on new information is good! For example, if we hadn’t adapted our practice based on new information, we would still be “double-dipping” our cloths and mops in disinfectants.
Key Learning: For environmental hygiene practice to be evidence-based, we must adapt quickly once new, credible information is available.
Ensure adequate supply for the next disaster
As Maya Angelou said, “When someone shows you who they are, believe them the first time.” Were your vendors good partners during the pandemic? This was an opportunity for vendors to demonstrate their true value to you. A good vendor partner ensured that existing customers kept receiving products and only took on additional customers as supply allowed. Now is a good time to ask your vendors if they are taking key learnings from the pandemic and applying them to prevent future product shortages when the next disaster strikes.
Key Learning: There are two questions you can ask your vendor partner to ensure that they are applying lessons learned from the pandemic to ensure adequate future supply.
1. How are vendors ensuring adequate supply, production capabilities, raw material availability, and distribution capacity?
For example:
• By staying close to their customers to know and understand any changes in demand
• By ensuring responsive supply chains, and, where possible, planning with max lead time
2. How are vendors applying the learnings from this pandemic to develop and communicate response plans for the next pandemic or disaster?
For example:
• By sourcing and supplying customers from manufacturing operations close to the customer.
• By identifying potential bottlenecks in situations and reducing dependency on single sources or multi-source suppliers of raw materials.
Linda Homan, RN, BSN, CIC, is senior manager of clinical affairs for Ecolab.
References:
1. Tyan K and Cohen PA. Investing in our first line of defense: Environmental services workers. Annals of Internal Medicine. 2020;173(4):306-7. doi: 10.7326/M20-2237
2. Cadnum JL, Pearlmutter BS, Jencson AL, et al. Microbial burden of inpatient and outpatient areas beyond patient hospital rooms. Infect Control Hosp Epidemiol. 2021 Jul 23;1-5. doi: 10.1017/ice.2021.309
3. Merriam Webster Online Dictionary (2021). Merriam Webster, Inc. https://www.merriam-webster.com/dictionary/science
The Critical Role of Environmental Hygiene in the Prevention and Control of Candida auris
By Linda Homan, RN, BSN, CIC
Editor's note: This column originally appeared in the September 2021 issue of Healthcare Hygiene magazine.
Candida auris is an emerging, multidrug- resistant fungi that is highly transmissible. The word “auris” is derived from the Latin word for ear, because this was the first body site in which the fungi was identified.1 As with other Candida species, C. auris colonizes the skin, mucous membranes, gastrointestinal tract and the female genital tract. Five percent to 10 percent of susceptible patients develop invasive infections, such as bloodstream infections, with high mortality rates. Infections caused by this organism have been tracked carefully and, until recently, were thought to occur due to exposure to antifungal drugs rather than via person-to-person transmission. However, in July 2021, the Centers for Disease Control and Prevention (CDC) released a report confirming transmission from patient-to-patient.2
In the wake of this new understanding that C. auris can be transmitted from person-to-person, the Association for Professionals in Infection Control and Epidemiology (APIC) released a statement urging healthcare facilities to adopt aggressive infection prevention and control measures to stop the spread of C. auris in healthcare settings.3 The most important prevention and control measures, as described by the CDC and reinforced by APIC, include:4
• Adherence to hand hygiene: Alcohol-based hand sanitizers are effective against C. auris, and are the preferred method for hand hygiene when hands are not visibly soiled.
• Transmission-based precautions are applied based on the setting, as with other multi-drug resistant organisms.
• Early identification and susceptibility testing, followed by coordinated communication between laboratory and clinical staff and between facilities is critical when C. auris is identified.
• Meticulous cleaning and disinfection of the patient-care environment that is confirmed by increased environmental monitoring in patient care areas.
As we have seen with other pathogens of concern such as C. difficile, these guidelines reinforce the critical role that the environment plays in the transmission of C. auris. Studies have determined that this organism can survive on moist and dry surfaces for up to one month.3,5 Even more challenging, there is evidence that it can survive in both wet and dry biofilms, making it harder to eradicate from the environment once it has been introduced.6.
In 2020, the CDC created Core Components for Environmental Cleaning and Disinfection in Hospitals.7 These core components outline an effective environmental hygiene program, and are more important than ever when faced with an emerging pathogen such as C. auris. Let’s look at these Core Components and how relate to management of C. auris:
Integrate EVS into the hospital safety culture.
Providing a clean patient environment is a cornerstone of a hospital’s safety culture. To prevent transmission of C. auris, frequent communication and collaboration between departments is critical. When patients are diagnosed or admitted with C. auris, the environmental services (EVS) department must be promptly notified so that C. auris protocols can be activated.
Educate and train.
When novel pathogens such as C. auris arise, all staff must be educated on the organism, its transmission, transmission-based precautions needed, and specific practices and products that must be incorporated to prevent transmission. Reinforce concepts with ongoing education with new healthcare personnel and as new guidance becomes available.
Select products that are effective against the organisms of concern.
There have been several studies that evaluate the efficacy of disinfectants against C. auris.8 The Environmental Protection Agency (EPA) maintains List P, which includes all EPA-registered antimicrobial products with claims against Candida auris, along with their contact times.9 Among the active ingredients that are effective are hydrogen peroxide/peracetic acid, dodecylbenzenesulfonic acid (DDBSA), hydrogen peroxide and sodium hypochlorite. If products on List P are not accessible or are otherwise unsuitable, interim CDC guidance permits the use of an EPA-registered, hospital- grade disinfectant that is effective against C. difficile. Quaternary ammonium compounds (QACs) are widely used as disinfectants in healthcare; however, data from recently published studies indicates that products whose only active ingredient is QAC are not effective against C. auris.4,10 Regardless of the product selected, it is important to read label claims and follow all manufacturer’s instructions for use, including applying the product for the correct contact time.
No-touch technologies such as vaporized hydrogen peroxide or germicidal UV irradiation are increasingly integrated into terminal cleaning processes.11 While there is limited research about the efficacy of these technologies specifically against C. auris, they may be an adjunct to routine cleaning and disinfection processes. Decontamination with 35 percent hydrogen peroxide vapor was deployed as part of a range of measures to successfully control a C. auris outbreak in a European hospital.12 In laboratory testing, Candida auris and two other Candida species were significantly less susceptible to killing by UV-C than MRSA.13
Standardize protocols.
The CDC C. auris guidelines recommend meticulous attention to daily and terminal cleaning/disinfection of all patient rooms, all areas where they receive care, and all shared equipment. C. auris has been cultured from many locations in patient rooms, including high touch surfaces and general environmental surfaces such as windowsills. Shared equipment such as glucometers, blood pressure cuffs and nursing carts have also been found to be contaminated with C. auris.4
Monitor Adherence and Provide Feedback.
Disinfectants are only effective when consistently and correctly applied. Objective monitoring and feedback on the thoroughness of cleaning using objective methods such as fluorescent markers are essential to ensure that critical surfaces and equipment have been disinfected. The CDC C. auris guidelines recommend increased environmental hygiene monitoring when there is a patient with known/suspected C. auris in the facility.4 Environmental hygiene monitoring data must be shared with staff and leadership to drive continuous improvement. For more information on evaluating environmental cleaning, review the CDC Toolkit: Options for Evaluating Environmental Cleaning.14
We now understand that Candida auris, a very dangerous emerging pathogen, can be transmitted easily from patient-to-patient, with the healthcare environment as a key vector. Once again, environmental hygiene plays a central role in preventing transmission of this emerging infection. The CDC has published recommendations for infection prevention for Candida auris, including the use of disinfectants that are effective against C. auris and increased environmental hygiene monitoring to ensure cleanliness. These pathogen-specific recommendations dovetail into previously published Core Components of Environmental Cleaning and Disinfection in Hospitals.
Linda Homan, RN, BSN, CIC, is senior manager of clinical affairs for Ecolab.
References:
1. Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K and Yamaguchi H. (2009). Candida auris sp. nov., a novel ascomycetous yeast isoated from the external ear canal of an inpatient in a Japanese hospital. Microbiology and Immunology, 41-44.
2. Lyman M. (2021). Notes from the Field: Transmission of Pan-resistant and Echinocandin-resistant Candida auris in healthcare facilities - Texas and the District of Columbia, January-April 2021. Morbidity and Mortality Weekly Report, 1022-1023.
3. Association for Professionals in Infection Control and Epidemiology. July 28, 2021. APIC Statement: With resistant C. auris spreading, healthcare facilities must adopt aggressive infection prevention and control measures. Retrieved from Association for Professionals in Infection Control and Epidemiology: https://apic.org/apic-statement-with-resistant-c-auris-spreading-healthcare-facilities-must-adopt-aggressive-infection-prevention-and-control-measures/
4. Centers for Disease Control and Prevention. July 19, 2021. Infection Prevention and Control for Candida auris. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/fungal/candida-auris/c-auris-infection-control.html
5. Piedrahita C, Cadnum J, Jencson A, Saikh A, Ghannoum M and Donskey C. July 28, 2017. Environmental surfaces in healthcare facilities are a potential source for transmission of Candida auris and other Candida species. Infection Control and Hospital Epidemiology, 1107-1109. Retrieved from Association for Professionals in Infection Control and Epidemiology: https://apic.org/apic-statement-with-resistant-c-auris-spreading-healthcare-facilities-must-adopt-aggressive-infection-prevention-and-control-measures/
6. Ahmad S and Alfouzan W. (2021). Candida auris: Epidemiology, diagnosis, pathgenesis, antifungal susceptibility, and infection control measures to combat the spread of infections in healthcare facilities. Microorganisms, 807-832.
7. Centers for Disease Control and Prevention. Oct. 13, 2020. Reduce Risk from Surfaces: Core Components of Environmental Cleaning and Disinfection in Hospitals. Retrieved from Centers for Diease Control and Prevention: https://www.cdc.gov/hai/prevent/environment/surfaces.html
8. Ku T, Walraven C and Lee S. (2018). Candida auris: Disinfectants and Implications for Infection Control. Frontiers in Microbiology, 1-12.
9. United States Environmental Protection Agency. July 21, 2021. List P: Antimicrobial products registered with EPA for claims against Candida auris. Retrieved from EPA: https://www.epa.gov/pesticide-registration/list-p-antimicrobial-products-registered-epa-claims-against-candida-auris
10. Cadnum J, Shaikh A, Piedrahita C, et al. (2017). Effectiveness of disinfectants against Candida auris and other Candida species. Infect Control Hosp Epidemiol. 1240-1243.
11. Weber D, Kanamori H and Rutala W. (2016). No Touch technologies for environmental decontamination. Focus on ultraviolet devices and hydrogen peroxide systems. Current Opinion in Infectious Diseases, 424-31.
12. Schelenz S, Hagen F, Rhodes J, Abdolrasouli A, Chowdhary A, Hall A, et al. (2016). First hospital outbreak of the globally emerging Candida auris in a European hospital. Antimicrobial Resistance and Infection Control, 1-7.
13. Cadhum J, Shaikh A, Piedrahita C, Jencson A, Larkin E, Ghannoum M and Donskey, C. (2017). Relative resistance of emerging fungal pathogen Candida auris and other Candida species to killing by ultraviolet light. Infect Control Hosp Epidemiol. 94-96.
14. Centers for Disease Control and Prevention. Oct. 15, 2010. Healthcare-associated Infections: Options for Evaluating Environmental Cleaning. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/hai/toolkits/evaluating-environmental-cleaning.html
The Business Case for UV-C Disinfection
By Jim Gauthier
Editor's note: This column originally appeared in the July 2021 issue of Healthcare Hygiene magazine.
Contaminated surfaces play a significant role in the transmission of pathogens. A paper by Jon Otter of the National Center for Biotechnology Information summarized studies that demonstrated different healthcare pathogens that are found in the environment that are shed by patients that can be moved to other patients. Organisms included Clostridioides difficile, antibiotic resistant organisms, and viruses.
Frequently touched surfaces are more heavily contaminated and represent greater risk. In a hospital environment, surfaces near patients are often contaminated. Those contaminated surfaces increase the risk of transmission, either directly or through hands of patients and staff. Crowded rooms with lots of activities and poor ventilation can help spread respiratory viruses. Manual cleaning and disinfection is often inadequate, creating increased risk for transmission.
Carling, et al. (2008) studied cleaning compliance across 23 acute-care facilities and found that overall compliance with key surfaces was 49 percent (range of 35 percent to 81 percent), indicating half of high-touch surfaces were not being routinely cleaned during discharge (terminal) cleaning of patient rooms. Cleaning compliance varied significantly by surface (the bathroom light switch was 20 percent and the sink was 82 percent). Carling’s study found a high variability between hospitals, with the cleaning compliance by surface in a different order for each hospital.
Due to time pressures, manual cleaning and disinfection are not being consistently performed to achieve safe environments. A study by the Association for the Healthcare Environment (AHE) of environmental services (EVS) cleaning in hospitals in the U.S. found that on average staff spent 15 minutes performing a daily clean of a patient’s room and 44 minutes performing terminal cleaning procedures in a recently vacated patient room. Because of time pressures, staff may resort to shortcut cleaning practices, which reduces cleaning compliance. Also, individuals will clean a room slightly differently than their peers, regardless of training received.
In their study, Bernstein, et al. (2016) found that 30 percent of EVS staff say they don’t have enough time to do daily cleaning and 20 percent state they don’t have enough time for discharge cleaning. This type of oversights can present serious risk to patients admitted into a room previously occupied by colonized or infected patient.
The Centers for Disease Control and Prevention (CDC) recommends “…a multi-barrier strategy to prevent healthcare-associated infections.” In their Hierarchy of Controls (see figure 1), rather than focusing only on improving cleaning compliance (an administrative control), adding an engineering control may be more effective, and could help reduce some of the variability seen between different EVS staff.

Figure 1: Hierarchy of Controls. Courtesy of the CDC
“No-touch” disinfection solutions such as UV-C devices work without user involvement to protect from any gaps in current cleaning practices. What’s more, UV-C devices have been robustly tested and found effective through more than 40 studies measuring either the biocidal effect of UV-C light on microorganisms or the impact on healthcare-associated infection (HAI) rates. UV-C has been proven to kill vegetative bacteria, fungi, viruses and bacterial spores.
Wong, et al. (2016) evaluated 61 rooms and 360 surfaces for contamination before and after regular hospital disinfection. The authors found that prior to cleaning, 30 percent to 35 percent of rooms tested positive for MRSA, VRE, or C. difficile. Standard patient room cleaning and disinfection had a modest effect as some surfaces were routinely missed, and other surfaces appeared to have been contaminated during the cleaning process. However, the use of UV-C reduced contamination in those rooms to less than 5 percent. Floor bacterial levels were similarly reduced due to UV-C.
Ultraviolet (UV) light is a component of the electromagnetic spectrum that falls in the region between visible light and X-rays. It is invisible to the human eye, has been used for decades to disinfect air and water. Killing of microorganisms is most effective at light wavelengths of 254 nanometers. UV light can be divided into UV-A (black light), UV-B (tanning beds), or UV-C (disinfection). UV-C can deactivate DNA (dimerization). The physical process does not kill organisms directly, but it will prevent them from reproducing. While UV-C can be used as an effective, environmentally friendly, non-chemical approach to disinfection, it is most effective if surfaces are properly cleaned prior to its application, as UV-C has poor penetration through soils or fabric.
UV light, as electromagnetic radiation, behaves according to set rules of physics. It should be noted that UV light intensity decreases with the square of the distance from the bulb. This mean, if 100 arbitrary units of energy were delivered at one foot from the bulb and the distance was doubled to 2 feet, only 25 percent of the energy would be detected (2 squared is four, ¼ of 100 is 25). And that efficacy number goes down to 11 percent when the bulb is 3 feet away from a surface (3 squared is 9, 1/9 of 100 is ~11). This is physics and not a device issue, as light energy (photons) collides with molecules in the air and lose energy.
UV-C effectiveness is also impacted by the angle of incidence. UV-C light intensity decreases when the light strikes surfaces at flatter angles. Full energy is delivered when a device is perpendicular to the surface (90 degrees). At a 45-degree angle, the effectiveness of the energy drops to 70 percent. And a 22-degree angle cuts efficiency to 38 percent. Anything that reduces the dose delivered reduces efficacy, which, as shown, includes distance to surface and angle of incidence. Efficacy is measured by the total dose of UV-C delivered to a surface, and hence, is a function of bulb intensity, distance of a surface to the bulb, angle to the surface and time of exposure.
UV-C device makers address these factors by:
• Moving the unit on a robotic base; however, these types of these units typically do no stay in one place long enough to provide significant efficacy
• Adding more and more bulbs to the device, trying to shorten the overall exposure time within the area
• Implementing longer cycle times. While this can increase the dose delivered, it can also cause surface damage over time, especially to objects closer to the bulb system, and the longer cycle time can add to delays in reusing the room.
Ideally, the UV-C device under evaluation should feature actuating arms, which can overcome these issues.
Additional issues to factor in concerning the use of UV-C devices include:
• Shadowing: This is when UV light cannot strike a surface directly, so it receives less energy, reducing efficacy. UV light does not reflect (bounce) very efficiently (as the distance issue above becomes more pronounced). UV-C reflective paints have been suggested, but the distance the light has to travel, and the corresponding reduction in power is still a factor.
• Overexposure: High amounts of UV-C for extended periods on certain plastics, such as ABS, may yellow these materials over time.
• Soil residue: Soil on surfaces reduces efficacy of UV light. Cleaning surfaces before UV-C disinfection is highly recommended.
At a recent Association for Professionals in Infection Control and Epidemiology (APIC) conference, a focus panel with infection preventionists around UV-C selection criteria found that turnaround time of the room was the most important consideration for a UV-C device (26 percent of participants). This was followed by cost (18 percent), efficacy (18 percent), ease of use (9 percent) and portability (9 percent). Other criteria included prep time (6 percent), cycle reporting capabilities (6 percent), evidence/studies of effectiveness (5 percent) and user safety (3 percent).
Assuming a hospital wants to move forward with a UV-C device for their facility, questions about funding sources will likely arise. The first thing to do is create an awareness around the need for UV-C. Be sure to identify the problem(s) to be solved. Funds for these types of devices can typically be found in capital equipment budgets, the government, foundations, community interest groups, private funding (i.e., families and others), online campaigns and lobbying in local news and radio.
To justify funding, follow the rules of the SBAR format:
• Situation: Describe the circumstances; bring something unique to the funding source, talk about the need for a non-chemical insurance plan.
• Background: Tell a story; draw a picture, use data from articles to show that cleaning and disinfection may not be 100 percent.
• Assessment: Bring data to the story. Everyone has needs, illustrate why UV-C is so important and will ultimately make the community better.
• Recommendation/request: Do not be shy; ask for what you need.
Another funding avenue is through creating a purchase/procurement policy to leverage grant funding. To assure no bias in the process, several key policy items need to be considered:
• Ensure procurement procedures are well documented
• Adopt a clear conflict-of-interest policy
• Avoid the purchase of unnecessary or duplicative items
• Provide full and open competition
• Establish micro and simple acquisition thresholds that are in line with federal rules and reflect internal operations
• Plan for formal procurement
• Non-competitive procurement would be a last resort
Also worth looking into:
• The government’s Emergency Grants for Rural Health Care' program. As part of President Biden’s COVID-19 relief package announced in March, $500 million is set aside for grants that will help rural hospitals’ efforts around COVID-19
• In April HHS announced $1 billion from the American Rescue Plan for construction and renovation projects at health centers
• In May, the U.S. Department of the Treasury announced the American Rescue Plan will deliver $350 billion for eligible state, local, territorial, and Tribal governments to respond to the COVID-19 emergency and bring back jobs
In summary, contaminated surfaces play a significant role in the spread of pathogens, and manual cleaning and disinfection may not always be optimal or consistent. UV-C is a proven and effective chemical-free technology to reduce contamination, risk and process variance. Evaluation of key criteria can help determine the UV-C device that best fits a facility’s needs and workflows. Staff and patients appreciate the investment in technology to keep them safe and resources are available to help with purchase and funding.
Jim Gauthier is senior clinical advisor for infection prevention at Diversey. Funding information provided by Reagan Lynch.
References:
Bernstein DA , Salsgiver E, Simon MS, Greendyke W, Eiras DP, Ito M, Caruso DA, Woodward TM, Perriel OT, Saiman L, Furuya EY and Calfee DP. Understanding Barriers to Optimal Cleaning and Disinfection in Hospitals: A Knowledge, Attitudes, and Practices Survey of Environmental Services Workers. Infect Control Hosp Epidemiol. 2016 Dec;37(12):1492-1495. DOI: 10.1017/ice.2016.206. Epub 2016 Sep 13. DOI: 10.1017/ice.2016.206
Carling PC, Parry MF, Von Beheren SM. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infect Cont Hosp Epidemiol 2008;29(1):1-7. DOI: 10.1086/524329
Wong T, Woznow T, Petrie M, Murzello E, et al. Postdischarge decontamination of MRSA, VRE, and Clostridium difficile isolation rooms using 2 commercially available automated ultraviolet-C-emitting devices. Am J Infect Control. 2016;44:416-20. http://dx.doi.org/10.1016/j.ajic.2015.10.016
Healthcare Drains as a Hidden HAI Reservoir: Challenges and Prevention Strategies
By Linda Homan, RN, BSN, CIC
Editor's note: This column originally appeared in the June 2021 issue of Healthcare Hygiene magazine.
Published literature reviews provide evidence that sink, shower and other wastewater drains in healthcare settings have been associated with outbreaks, particularly among the most vulnerable patient populations in neonatal and adult intensive care units, burn units, transplant units and hematology/oncology units. These outbreaks are difficult to recognize and manage because long intervals of time may pass between cases, and the number of cases at any given time is low. Once an outbreak is identified, it can be challenging to eliminate the source – bacteria growing in biofilms in drains. Previously identified methods to disinfect drains have had very limited success.1,2
Waterborne bacteria are the predominant organisms found in sink-related outbreaks with the most common organism being Pseudomonas aeruginosa. Other pathogens include Enterobacteriaceae, such as Escherichia coli, Klebsiella pneumoniae, Klebsiella oxytoca, Serratia marcescens, Enterobacter species, and Citrobacter species. Multidrug-resistant strains of these organisms are commonly found, with carbapenemases most frequently identified. Enterobacteriaceae producing extended-spectrum beta-lactamases (ESBLs) as well as multidrug-resistant P. aeruginosa and A. baumanii are also commonly identified. The true burden of sink-related infections is likely underestimated as there is currently no widespread systematic strategy to identify and track this type of healthcare-associated infection.3
Immunocompromised patients are most susceptible to infections with these organisms.1 In a review of four studies, Kizny-Gordon, et al. found that risk factors for wastewater drain-associated colonization or infection are: preceding surgery, patient location, prolonged mechanical ventilation, older age, burns, longer hospital stay, and drinking tea from a contaminated dispenser.2 Almost all identified outbreaks have occurred in ICUs and hematology-oncology units.
Parkes, et al. reviewed the risk mitigation strategies for sink related outbreaks between 2012-2018, discussed here.3
• Sink and faucet configurations may contribute to the transmission. Faucets flowing directly into drains and shallow sink basins have been shown to cause splash-back. This can contaminate the hands of healthcare workers or patient care items that are stored adjacent to the sink. In addition, sinks are often used to dispose of fluids and materials other than water. These non-water substances can provide nutrients to encourage bacterial biofilm growth.
• Hospitals often have aging and modified water systems with uneven temperature control and dead-end pipes. Temperature fluctuations and stagnant water can contribute to bacterial growth in hospital tap water.
• Below the drain, plumbing issues may also exist, such as scale build up or p-traps and piping made of materials that encourage biofilm growth.
• Most methods to disinfect drains are not effective at killing bacteria in drains. Efforts to disinfect drains have included complete replacement of the sink or its components, installing self-cleaning traps, disinfection with processed steam, enhanced manual cleaning, descaling of pipes, and disinfection with chlorine-based solutions or other liquid disinfectants. Liquid disinfectants do not contact the surface of the drain long enough to meet the contact time needed to kill the bacteria.4
Existing methods to react to drain-associated outbreaks have been “woefully ineffective” at eliminating sink colonization.3
Parkes, et al. suggest a more proactive approach including optimizing best practices in sink design and placement and changing healthcare worker behavior to prevent transmission:
• Correct defective conditions in water systems such as dead ends, low water-use areas, and temperature/pressure fluctuations
• Ensure that faucets don’t flow directly into the drain to minimize splashing/aerosolizing
• Consider changing to deeper sink basins to prevent cross-contamination of hands and adjacent surfaces
• Eliminate misuse of sinks to dispose of fluids and materials that can provide nutrition for bacterial biofilm growth
• Ensure that patient care items are not stored adjacent to sinks to avoid cross-contamination
• Ensure that p-traps and piping are made of materials that minimize biofilm growth
• Consider replacing sinks or affected components to remove the source of transmission. (Replacing sinks may solve the problem temporarily, but eventually biofilm will grow in the new sink if other prevention measures aren’t taken.)
• Various methods of cleaning and disinfecting drains have been tried with mixed results. They sometimes end the outbreak but do not provide sustained decolonization of sinks.
If you have concerns about drains as a vector for pathogens, a drain disinfection program with a product that kills biofilm and can be easily applied on a routine schedule may provide sustained decolonization of the sink drain, thereby preventing transmission of potentially dangerous pathogens from sinks. However, it’s important that the product used to disinfect drains stays in contact with the drain surface above the p-trap for the required contact time in order to be effective. When compared to liquid or chlorine-based disinfectants, recent studies conducted using hydrogen peroxide/peracetic acid/octanoic acid foaming disinfectant have demonstrated efficacy in drains, have been effective in suppressing proximal sink drain colonization for at least three days, and are easy to use.4-5
Linda Homan, RN, BSN, CIC, is senior manager of clinical affairs for Ecolab.
References:
1. Carling PC. Wastewater drains: Epidemiology and interventions in 23 carbapenem-resistant organism outbreaks. Infect Control Hosp Epidemiol. 2018;39(8):972-979.
2. Kizny Gordon AE, Mathers AJ, Cheong EYL et al. Carbapenem-resistant organisms causing hospital-acquired infections: A systematic review of the literature. Clin Infect Dis. 2017;64:1435-1444.
3. Parkes LO, Hota SS. Sink-related outbreaks and mitigation strategies in healthcare facilities. Current Infectious Disease Reports. 2018;20:42.
4. Jones LD, Mana TSC, Cadnum JL, Jencson AL, Silva SY, Wilson BM, Donskey CJ. Effectiveness of foam disinfectants in reducing sink-drain gram-negative bacterial colonization. Infect Control Hosp Epidemiol. 2020;41:280-285.
5. Ramos-Castaneda JA, Faron ML, Hyke J et al. How frequently should sink drains be disinfected? Infect Control Hosp Epidemiol. 2020:1-3.
Do Surfaces Contribute to the Spread of COVID-19 and What is the Risk of Contamination?
By Linda Lybert
This column originally appeared in the June 2020 issue of Healthcare Hygiene magazine.
The Centers for Disease Control and Prevention (CDC) last week came out with new guidelines for how to safely reopen and further informed the public that coronavirus does not easily spread via surfaces. Please don’t be confused -- surfaces matter and there is not enough evidence to say it does not spread via surfaces.
It is important to remember this is a novel virus, and there is significant ongoing research happening to try to understand the virus and protect the health and welfare of everyone as we navigate through this serious pandemic. Information is changing, and confusion occurs.
SARS-COv-2 is a novel respiratory virus that causes COVID-19; the primary mode of transmission is aerosolized droplets and human contact. The scientific evidence of this is apparent.
Early research that endeavors to understand the way this virus is transmitted revealed that the pathogen on various surfaces, including walls. Just because the virus was found does not mean that the virus can be acquired from the surface, transmitted to a human host, and they become sick. More research is needed; there is, however, enough research to warn people of a potential area of concern.
The new CDC guidelines clearly outline intensified cleaning and disinfection and state that surfaces are not a primary mode of transmission. There are many recent articles written that minimize the need to clean and disinfect surfaces. What it actually means is that we no longer need to clean all of our groceries, packages, and money. It does call attention to frequently touched surfaces. See the excerpt from the CDC guidelines below.
Intensify cleaning, disinfection, and ventilation (Steps 1–3)
• Clean and disinfect frequently touched surfaces at least daily and shared objects between use
• Avoid use or sharing of items that are not easily cleaned, sanitized, or disinfected
• Ensure safe and correct application of disinfectants
• Ensure that ventilation systems operate properly and increase circulation of outdoor air as much as possible such as by opening windows and doors. Do not open windows and doors if doing so poses a safety risk to individuals and employees using the workspace
• Take steps to ensure that all water systems and features (for example, drinking fountains, decorative fountains) are safe to use after a prolonged facility shutdown to minimize the risk of Legionnaires’ disease and other diseases associated with water
SARS-CoV-2 is a virus, and viruses require a host to survive. While it may live on a surface, what is unknown is how much bioburden it takes for transmission of the virus from the surface to a host and the host to become infected. More research is needed.
As businesses begin to reopen, and infection prevention and cleaning and disinfection strategies and protocols are developed, an assessment of "high-touch" surfaces must be completed. There are many different surface materials and textiles in any given setting, and most people evaluate environmental surfaces. Unfortunately, that leaves out many highly touched surfaces. Consider soft surfaces such as clothing that become highly contaminated throughout the day from many different locations, ultimately supporting the transmission of pathogens wherever people go. What about medical equipment such as blood pressure cuffs, gait belts, wheelchairs, IV poles? It is surprising how highly touched these surfaces are but would not be considered high-touch. The list is long, and it gets complicated very quickly.
Humans shed approximately 1 million microbes a day (Gan, 2015). What amount of viral shedding from a COVID-19 patient does it take before the surfaces surrounding that patient have enough bioburden for easy cross-contamination to then occur? A sick patient with symptoms who is at home will remain in a relatively small area such as a bedroom, identification of surfaces that must be regularly disinfected can be easily identified.
We now know that about 40 percent of the people who are COVID-19 positive are asymptomatic. The identification of high touch and highly touched surfaces must come following observation of the human interaction with surfaces is observed. Sinks, doorknobs, faucets are a great start. What about the family car, with high-touch surfaces including the steering wheel, door handle (both inside and out), seat belt, center console, turn signal, information display, radio, and the keys -- the list of high-touch surfaces in a vehicle is endless.
An immediate and easy solution is to be diligent with hand hygiene. Also, a surface, hands will come in contact with your face and transmit any pathogens that have been acquired. It is easy to take a few minutes to wash your hands using soap and water or hand sanitizer.
Since the release of the new guidelines, there have been numerous articles written, and much misinformation shared. Surfaces are not the primary mode of transmission, but the CDC recommends "intensifying cleaning, disinfection and ventilation." Additional facts include:
• Scientific evidence has shown that the virus spreads via aerosolized spray and droplets and human contact
• We are dealing with a novel virus, and what we know today may change as more research is done.
Looking beyond COVID-19, it is a fact that there are many different types of microbes that effectively live and, in some cases, thrive on surfaces for days weeks and even months. Surfaces have a significant impact in microbial acquisition and transmission. More research is essential. While a virus needs a host to survive for very long other pathogens do not, and you are always at risk. A good cleaning and disinfection strategy, process and protocols are critical.
Linda Lybert is founder and executive director of the Healthcare Surfaces Institute.
References:
Centers for Disease Control and Prevention. Accessible at: https://www.cdc.gov/coronavirus/2019-ncov/downloads/php/CDC-Activities-Initiatives-for-COVID-19-Response.pdf#page=49
Gan V. Our Bodies, Our Microbial Clouds. Sept. 22, 2015.
Cleaning and Disinfection in the Era of COVID-19
By J. Darrel Hicks
The necessary steps of cleaning and disinfection include best-in-class products, processes and people who are educated about the prevention and transmission of disease.
The simple cleaning and disinfection of environmental surfaces or frequently touched surfaces may be one of our key defenses in the future battle against infectious disease such as COVID-19. With antibiotic-resistant organisms proliferating on common touch-points for up to 56 or more days, the study of cleaning and measuring cleanliness is becoming all-important.
Firstly, coronavirus is an enveloped virus.
Enveloped viruses tend to be easier to disinfect because the outer membrane “envelope” is sensitive to heat, dry conditions and disinfectants. There is a tendency, in the context of a new pandemic, to go for the strongest disinfectant conceivable for surface disinfection.
With a harder to kill virus, or a virus with particularly high mortality, that may be appropriate, however, for COVID-19 that appears to be unwarranted. Of course, if you want a stronger disinfectant, with full virucidal claims, then there are several available for surface disinfection.
However, in the normal course of events, where surface contamination is a concern, but not a confirmed risk, then Standard Precautions, using a compatible hospital grade disinfectant and wipe should be sufficient to ensure a clean and disinfected surface.
Part of the issue here, is not to destroy surfaces or adversely affect staff or medical equipment with unnecessarily strong disinfectants such as highly concentrated chlorine solutions.
Let’s review the terms used.
• Cleaning is the process of removing contaminants from the environment and putting them in their place. Cleaning occurs after contaminants have entered the indoor environment. In cleaning we find, identify, capture, contain, remove and dispose of contaminants. Cleaning is not diluting. Cleaning is removing. We don’t hide or brush aside dusts and wastes and say we’re cleaning. We must remove and dispose of them, too. The CDC’s definition for cleaning refers to the removal of dirt and impurities, including germs, from surfaces. Cleaning alone does not kill germs. But, by removing the germs, it decreases their number and therefore any risk of spreading infection.
• Again, the CDC’s definition for disinfecting works by using chemicals to kill germs on surfaces. This process does not necessarily clean dirty surfaces or remove germs. But killing germs remaining on a surface after cleaning further reduces any risk of spreading infection.
• For an environment to be considered disinfected, we remove or make safe the vast majority (95%) of microbes of concern in it. We eliminate the pathogens that are most threatening to humans. A disinfected condition can be achieved, but only with much work.
• For an environment to be considered sanitary, we clean it to the point that it protects human health in general, but it still has some contamination. A risk of disease still exists, but it is at an acceptable risk level. At a minimum, cleaning must always achieve a state of “sanitation.” An unsanitary condition poses a likely health risk. The purpose of cleaning is to correct the risky condition. Therefore, if a risk has not been improved to a level we call sanitary, cleaning has not been accomplished.
A word about COVID-19 and medical waste: Waste from COVID-19 patient’s room does not meet the definition of “red bag” or regulated medical waste unless blood and body fluids are present and the waste meets the federal, state and local definition of such waste. Although any item that has had contact with blood, exudates, or secretions may be potentially infective, treating all such waste as infective is neither practical nor necessary. Federal, state and local guidelines and regulations specify the categories of medical waste that are subject to regulation and outline the requirements associated with treatment and disposal. State regulations also address the degree or amount of contamination (e.g., blood-soaked gauze) that defines the discarded item as a regulated medical waste. Check your state for additional regulation regarding treatment of medical waste.
Carpeting presents Its own issues. Hospitals and nursing homes have a surprising amount of carpet, and a concern with vacuuming is that it could aerosolize bacteria and viruses like COVID-19 that have settled onto the carpet. Vacuuming protocols must be examined from an infection control and cross-contamination lens to ensure that these risks are mitigated.
Dr. Gavin Macgregor-Skinner of the Global Biorisk Advisory Council (GBAC), a division of ISSA, notes that many facilities have used vacuums to pick up dust and debris without thinking about how to minimize the risk of infection. During the COVID-19 pandemic, some facilities have stopped vacuuming altogether for fear of aerosolizing the virus, and those facilities are becoming quite dirty, so we must find a safe way to vacuum. Macgregor-Skinner says there are many knowledge gaps around vacuuming, including about the use of HEPA filters, whether or not they are effective against SARS-CoV-2, the best type of vacuum to use, and the best time of day to vacuum. Training and education are needed to resolve these gaps.
One training tool he uses is smoke near a running vacuum to demonstrate how the air moves through and around the vacuum. That visualization then leads to a discussion about how vacuums might contribute to moving virus particles throughout an environment, and how to address that problem.
This discussion around cleaning and vacuuming for infection control in healthcare settings is not new, but Macgregor-Skinner says it has not been well thought-out in the past and is receiving much more attention during the current COVID-19 crisis.
J. Darrel Hicks, BA, MREH, CHESP, is the owner/principal of Darrel Hicks, LLC and the author of the book Infection Prevention for Dummies. He is also interim president and an executive board member of the Healthcare Surfaces Institute.
A Novel Crisis Requires Essential EVS Leaders
By J. Darrel Hicks, BA, CHESP, MESRE
Editor's note: This column originally appeared in the May 2020 issue of Healthcare Hygiene magazine.
SARS appeared in late 2002 and quickly spread around the world the following year. The CDC reported that 8,098 people were infected in 26 countries, and that 774 died. SARS was called the first pandemic of the 21st century. It would not be the last. Nor would it be the deadliest. As of April 24, 2020, there are nearly 3 million confirmed cases of SARS-COVID-19 in the world and nearly 200,000 deaths.
It was during that “little” pandemic in 2003, that hospitals first started planning for the “surge” that never materialized. Disaster preparedness became the focus of table-top drills and dealing with the “what if” scenarios. Then disaster planning centered around risk-assessments and contingencies that never materialized.
Crises come in two forms: normal and novel. A “normal” crisis would call for Hospital Incident Command System (HICS) planning in the event of natural disasters such as hurricanes, tornadoes, earthquakes, ice/snowstorms, floods, etc. Novel crises are those risks that exhibit unusual frequency and impact. Organizations typically don’t have plans for such events. Novel crises may be a confluence of two or three events that strike at the same time. Or they may simply be too big or unusual to be imagined.
The wave/surge of COVID-19 patients overwhelmed some hospitals, particularly New York City, while other hospitals were planning for the possibility of more patients than their ICU-bed capacity could accommodate.
A novel crisis places strains on leadership. In the EVS department, leadership is especially important for a safe, clean and disinfected environment for patient care. Here are some of the essential elements for EVS leaders during these days of staffing shortages, PPE, supply chain disruptions, isolation room processing and high patient census.
Lead decisively: As Max De Pree noted, “the first responsibility of a leader is to define reality.” Leaders must wade into the mire in order to learn precisely what is happening at any given moment and to make sense of current conditions. A leader’s visible presence during times of crisis inspires confidence and gives others a sense of security. Certainly, the ability of leaders to control their own emotions is paramount during crisis. The EVS leader might be directing a resource-challenged department but that is a hurdle they must clear. The leader and the leadership team must be visible, approachable and leading by example as they approach the novel crisis head on. It’s not uncommon to make mistakes, so it’s important to be flexible and back up, change course, adjust and go forward again.
Continuously frame the crisis: Rather than holding fast to the first impression and analysis of what is happening in the ED or the ICU, be flexible to embrace new information as it comes along. If new analysis suggests a remake of the original plan, remake the plan. One of the most important things for any EVS leader is to identify what the situation on the ground is and to constantly look at that identification every couple of hours, days and weeks because crises can change, and they can become multiple events. What you thought was unimportant yesterday can become extremely important tomorrow.
During a crisis, make it a point to withdraw from everything momentarily to list out your top concerns. Then assemble the core leadership team, gather their input, and amend the list accordingly. Putting the main issues on paper helps to wrap your mind around the crisis and to stay focused amid chaos.
Actively communicate: During a crisis, it’s important to constantly communicate up to leaders and down to employees and vendors. It’s also critical to keep a record of the facts through hand-off reports required of all shift leaders. It is extremely important to actively communicate up and down in an organization, as well as to internal customers and employees. Honesty and transparency are critical.
Be ready for the unexpected: Under extreme pressure, the EVS leader should understand that individuals may act differently than during normal circumstances, and that the usual organizational roles may not apply during a crisis. This can further add to the unpredictability of day-to-day, shift-to-shift operations. Have a plan for what the operations look like when 10 percent to 20 percent of your staff are off the schedule due to being quarantined for 14-days because they have been exposed to COVID-19.
Drive toward actionable intelligence: During a crisis, leadership must often navigate confusing data and intelligence. It’s important to cast a wide net, as crucial information can come from a range of sources, including your professional membership group. But those sources must be qualified, as misinformation can be as prevalent as information. It’s important to consider sources carefully. The CDC is an essential resource when it comes to cleaning and disinfection.
Manage the crisis lifecycle, not just the event: The timeliness and effectiveness of your department’s response in a crisis often determines how it fares afterward. Front-loading a crisis management approach with a strong emphasis on readiness, preparation and follow-up can help departments more effectively stay ahead of potential threats.
What’s important is to think of crisis management in terms of a cycle—moving from preparation to response to recovery and then around again—applying lessons learned from one stage to the plans and processes that support the other stages. Infection prevention and control are the essential elements of the EVS department’s mission. EVS workers are essential to the mission of the healthcare institution of providing state-of-the art compassionate care to their public. But EVS leaders are essential to both missions.
Reference: Crisis Leadership: Five Principles for Managing the Unexpected. Wall Street Journal. July 6, 2015. https://deloitte.wsj.com/riskandcompliance/2015/07/06/crisis-leadership-five-principles-for-managing-the-unexpected/
Technology No Match for an Educated and Engaged EVS Staff
By J. Darrel Hicks, BA, MESRE, CHESP
This column originally appeared in the April 2020 issue of Healthcare Hygiene magazine.
My wife and I spent three nights in a very up-scale vacation club hotel in Orlando, Fla recently; along with those fantastic accommodations we had to endure the two-and-a-half-hour sales pitch from the sales team. I’m sure you have probably done something similar, so I won’t go into detail about the experience.
The salesman asked us a rhetorical question, “What is the most expensive room in a hotel?” My wife took the words out of my mouth, “Penthouse suite.”
“No, it’s an empty room,” replied the salesman. From there, he expounded on how we could capitalize on the need of hotels and resorts to “sell” those empty rooms.
Let me ask you, what is the greatest cost to your environmental services (EVS) department? Is your highest cost labor? Expenses? Contracted services?
I would like to make a case that it is none of these. Instead, the greatest cost to your department and to providing a safe, clean and disinfected environment for patient care is this: Uneducated and Unengaged cleaning professionals.
What is the cost of not providing a safe, clean environment? It could be millions of dollars and a loss of confidence by the community a hospital serves. A court awarded $13.5 million to the family of a patient who died of flesh-eating bacteria that she contracted during chemotherapy treatment. In a separate case, a patient was awarded $2.58 million because he contracted methicillin-resistant Staphylococcus aureus (MRSA) in a hospital. Although cleaning and hygiene issues may not always be the subject of dramatic litigation, there is little doubt that poorly cleaned facilities are contributing factors to serious disease transmission.
In the business of providing healthcare to more than 35 million inpatients and performing 51 million-plus procedures annually,1 it is critically important that everyone – from hospital executives down to front-line workers – understands and embraces patient and employee safety. If a culture of safety is not at the heart of the organization, the health of patients, employees and the organization’s bottom line can all be adversely affected.
Additionally, long-term care facilities continue to send many of their residents to hospital emergency departments and most of them end up becoming inpatients. In those long-term care facilities, “…between 1 million and 3 million residents get a healthcare-associ¬ated infection and up to 380,000 succumb to those infections.”
Beyond patient and employee safety, there is also the financial risk to hospitals from loss of Centers for Medicare and Medicaid (CMS) and insurance reimbursement. A healthcare-acquired infection (HAI) could potentially add 19 days to the average 4.8 day length of stay,2 and possibly, at the expense of the hospital.
When hospitals want to compete in their market, leaders often look to the latest 128-slice, 3D CT scanner, a DaVinci robot to perform surgeries, recruit the best surgeon, or begin a new service line with the best ROI. While these capital expenditures and improvements might attract publicity for a fleeting moment, the board of directors needs to consider a different, low cost option that provides the best chance to improve patient satisfaction, reduce HAIs and improve the bottom line: the environmental services department.
When it comes to keeping pathogenic organisms at a safe level on environmental surfaces, the least educated and lowest paid people in the hospital must eliminate those dangerous bacteria. “This is the level in the hospital hierarchy where you have the least investment, the least status and the least respect,” says Jan Patterson, MD, past-president of the Society for Healthcare Epidemiology of America (SHEA).
That’s because hospitals have consistently held a low regard for the EVS department. Too often, housekeepers or environmental service workers are thought to be expendable (anyone knows how to clean a toilet and mop a floor, right?) and difficult to educate because English may not be their first language. The thought is, “What if I educate and train them and they leave?” But, worse than that, what if you don’t educate and train them and they stay?
Could the lack of educating and certifying your staff be costing your facility between $1 million and $3 million in extended stays associated with unsanitary patient-care environments? Has the safety of patients and staff been compromised to the point of loss of life? Shouldn’t you consider educating and certifying your EVS workers?
When it comes to technology as it relates “cleaning robots” or room disinfection systems, in a recent study researchers concluded that although UV disinfection was found to significantly lower bacteria counts, it provided the greatest benefit by supplementing the least efficient cleaning solutions, disinfectants, and cleaning professionals. The researchers and I believe, an educated and engaged EVS staff who are properly trained in proper cleaning protocols is the best defense against hospital pathogens.
In an increasingly more inclusive and employee-friendly healthcare industry, employee engagement has been catapulted to the forefront for many in the C-suite. Employees are surveyed more often to gauge their satisfaction with management, senior leadership, supplies, pay, and a host of other items deemed important by administration.
EVS worker engagement isn’t the problem; it’s a symptom of poor leadership. If a department or organization's leadership is complacent about creating a great place to work, then why should they have the expectation that their employees will be anything but complacent about their day-to-day responsibilities?
How much does this complacency cost your organization? According to Gallup, disengaged employees have 37 percent higher absenteeism, 18 percent lower productivity and 15 percent lower profitability. When that translates into dollars, you're looking at the cost of 34% of a disengaged employee's annual salary, or $3,400 for every $10,000 they make.
Let’s look at the math as it applies to a hypothetical EVS department with 50 frontline workers averaging $30,000 annually: 34 percent of $30,000 = $10,200
Using the Achievers data (which states that only 21 percent of employees are engaged), we can calculate that around 29 of those 50 employees are disengaged and complacent in their work.
That means that employee complacency cost your department $295,800 (29x$10,200) out of a labor budget of $1.5 million If 90 percent of your staff were fully engaged, the cost of complacency drops to just $51,000 for a savings of $244,800.
But much greater than the financial impact of complacency in the EVS department is the cost in human lives. The stakes are too high to allow the rooms of residents or patients to be cleaned by a person who is not properly educated and engaged. The EVS professional must be properly compensated, regarded as a part of the facility’s multi-modal infection prevention program, be well trained in the nuances of cleaning and disinfection, allotted the time to do the necessary tasks, equipped with the best-in-class tools to clean and disinfect surfaces and educated about the prevention and transmission of disease.
The Learning Objectives for Certifying your Cleaning Professionals (CPs)
• Define infection prevention as environmental services’ No. 1 job
• Equip the front-line cleaning professional (CP) with knowledge of infection prevention as it relates to their daily tasks
• Analyze the CP’s role in patient satisfaction
• Support the CP with practical “how to” tips for cleaning and disinfecting
• Introduce cleaning and disinfecting strategies that effectively break the chain of infection
• Convert the CP into a certified environmental services technician
An educated, engaged and certified EVS tech will be viewed as a knowledgeable professional working amongst other healthcare professionals who are certified or registered in their field. Knowledge leads the environmental services worker to be proud of the profession they have chosen and respected by those they work alongside of. In short, a fully engaged cleaning professional.
A closing thought: One well-trained, well-equipped, engaged certified environmental services technician, given the proper tools and an adequate amount of time to clean and disinfect a patient’s room can prevent more infections than a room full of doctors can cure.
J. Darrel Hicks, BA, MREH, CHESP, is the owner/principal of Darrel Hicks, LLC and the author of the book Infection Prevention for Dummies. He is also a board member and acting president of the Healthcare Surfaces Institute.
References:
1. Centers for Disease Control and Prevention (CDC). Hospital Utilization (in non-Federal short stay hospitals), Hospital Inpatient Care-Number of Discharges; Procedures Performed, May 14, 2015; http://www. cdc.gov/nchs/fastats/hospital.htm
2. Agency for Healthcare Research and Quality (AHRQ). Healthcare-Associated Infections Greatly Increase the Cost of Hospital Stays. AHRQ News and Numbers, August 25, 2010;
http://archive.ahrq.gov/news/newsroom/news-and-numbers/082510.html
Managing Hospital Waste
By Ed Barr
Editor's note: This column originally appeared in the March 2020 issue of Healthcare Hygiene magazine.
One of the challenges for hospitals is the expense and expertise needed to manage multiple waste streams. These waste streams pose a challenge, as most are governed by multiple governmental agencies.
The average hospital will deal with the following waste streams:
Municipal Solid Waste (MSW): MSW or trash is the largest form of waste by volume and weight. To manage this stream the waste is normally deposited in a compactor and the cost is based on the tonnage generated and the distance transported for disposal. Haulers can range from national companies to local “mom and pop” companies.
Regulated Medical Waste (RMW): RMW is known by several names i.e. Infectious, biohazardous, red bag trash etc. This waste stream poses several challenges as it is heavily regulated and consists of blood saturated items, sharps, trace chemotherapeutic and pathological. RMW is often mis-characterized and can cost a hospital money if placed in the MSW waste stream. Also, since it is normally disposed of by the pound it can be quite costly. Special training must be provided to employees to handle the waste and to sign manifest for shipment.
Recycling: Recycling is a waste stream that poses a challenge for most hospitals to manage. The types of items recycled include: Corrugated or cardboard, office paper, aluminum cans, plastic and glass food and beverage containers, packaging, toner cartridges are among the items commonly recycled. Separate handling and shipment are required and if not done properly can lead to contamination which causes a hospital to pay additional costs for disposal.
Hazardous Waste: Hospitals have several sources of chemicals coming from clinical and research labs as well as waste generated during clinical usage including bulk chemotherapy. Other waste in this category includes industrial grade and phone batteries.
Pharmaceutical Waste: Hospitals are now required to collect and separately dispose of their drugs. This requires separate collection boxes in the main and satellite pharmacies as well as clinical areas.
Electronic Waste: This waste consists of computers, televisions and other devises used in the institution. If the information has patient information covered by HIPAA you need to ensure that information is wiped out and not accessible to any unauthorized individuals.
Bulk Waste: Any waste too large to be disposed of in a compactor must be placed in an open top dumpster. This includes old furniture, hospital beds and other medical equipment
Construction Debris: Hospitals continually upgrade their facilities and the debris from the construction must be removed and disposed of. Some jurisdictions require separate handling of this material.
Radioactive Waste: Any radioactive waste used in the treatment of patients or research must be separately stored and disposed of.
Kitchen Grease: Grease collection from commercial kitchens are quite common and hospitals are no exception.
Each of these items requires time, labor and considerable expense to manage. Most are regulated by local, state and the federal government.
When managing waste streams, it is important to partner with vendors who can provide services for your institution. Some questions you may want to ask are:
- How long have they been in business?
- How many hospitals are they providing service for?
- What is the emergency plan for equipment failure during nights and weekends?
- Do they provide the service directly or do they subcontract the work?
- How does their program comply with local, state and federal regulations?
- How do they provide proof of destruction?
Regardless of the answers you want to make sure that you follow the trail of the waste to endure destruction. For example, if you have a company that removes your electronic waste you want to make sure you can prove destruction not just holding an invoice with the information.
For RMW, the stakes are higher if the waste is not properly disposed of. For example, if RMW is placed in your MSW waste stream and shows up at a landfill or transfer station the hospital is liable for removal and proper disposal. In addition, the waste provider will report the incident to the state department of environmental protection which can result in an investigation or fines for the hospital.
- If you decide to treat your waste onsite there are several things to consider:
- The capital costs associated to purchase onsite treatment frequently must compete with a limited pool capital dollar
- How long has the company been in business? Is this the company’s first install? Do they have a proven list of customers?
- How complicated is the equipment? What type of skills are needed to operate and maintain the equipment?
- What support does the company offer for ongoing preventive maintenance and repair issues?
- How does the equipment disinfect or sterilize the RMW? How do you know the waste has been treated?
Managing waste is a complicated process. However, the good news is there help and information out there to help you protect your institution and our planet.
 Ed Barr, CHESP is a director of environmental services for Sodexo. He has been active in the field of waste management and recycling for more than 30 years having run programs for a major academic medical center as well as serving as program manager for hospitals in the Mid-Atlantic region. He has served as president of the Greater Philadelphia Recycling Council and president of Greater Philadelphia AHE.
Ed Barr, CHESP is a director of environmental services for Sodexo. He has been active in the field of waste management and recycling for more than 30 years having run programs for a major academic medical center as well as serving as program manager for hospitals in the Mid-Atlantic region. He has served as president of the Greater Philadelphia Recycling Council and president of Greater Philadelphia AHE.
Contaminated Air and Surgical Infection Associated With Implant Procedures
By Sue Barnes, RN, CIC, FAPIC
Surgical Site Infection (SSI) Risk for Patients Who Have Implant Procedures
Patients undergoing surgical procedures which involve an implant such as prosthetic joint replacement, are at risk of post-operative infection caused by the very smallest bacterial inoculum.1 This is due to the surface of the implant on which biofilm can expediently develop, and also due to the patient’s immune system focusing initially on the implant versus any bacteria that might have adhered to its surface. Consequently, the number of organisms required to cause an infection when an implant is involved is reduced by a factor of 100,000.2
The Impact of Implant-Associated SSI
A common implant procedure in the United States is total hip replacement, of which there are approximately 300,000 performed annually. The average SSI rate for these procedures is 2.18 percent.3 While this is a low rate it still represents 8,400 patients, each experiencing pain, suffering and for some lost wages and impact on family and quality of life.4 For each patient the range of cost for treatment of the infection is between $389,307 and $474,004, and is associated with a mortality rate of between 2 percent and 7 percent.5,6 In addition to prosthetic joint replacement, many other types of surgical procedures now involve implants including, breast, plastics, orthopedic, spine, general (hernia mesh), gynecology (pelvic floor mesh), cardiac (pacemaker, stent, valve, internal atrial defibrillator).
Air Contamination and SSI
The direct correlation of bacteria laden particulates in operating room air to surgical infection risk has been reported for decades in peer reviewed studies.7-9 These particulates can become transiently airborne during a case, settle in the open incision and adhere to the implant.10 These may originate from any one of several sources, including respiratory aerosols of the surgical team which can escape from the surgical mask, especially in the presence of an upper respiratory tract viral infection.11,12 Another potential source of transiently airborne pathogens in operating rooms is the skin of surgical team members and/or patient. Skin scales are constantly shed from the human body, to which bacteria are often attached.13 Illustrating this risk, is a documented outbreak involving eight SSI reported after modified radical mastectomy in a tertiary-care hospital, caused by Group A streptococci (GAS). The source was found to be a surgeon colonized (skin) with GAS.14
A third potential source of transient airborne contamination in operating rooms is equipment which includes a water reservoir. The outbreak of Mycobacterium chimaera SSI after cardiac surgical procedures demonstrates this risk. In this outbreak, the water tanks on the heater-cooler devices used in open heart surgery were found to be the source for the airborne transmission of M. chimaera resulting in more than 100 SSI cases since 2013 in Europe and the U.S.15,16
Current State of Air Quality in U.S. Operating Rooms (OR) versus Compounding Pharmacies
In the OR, surgical procedures involve an incision (sterile space), which remains open to the OR air. In compounding pharmacies sterile solutions are prepared to be introduced into the sterile vascular system. Regulations governing these two spaces are not equivalently protective. On the one hand, U.S. compounding pharmacies must comply with International Standards Organization (ISO) class 5 standards for air quality.17 However, there is no requirement for air quality testing in US operating rooms, where it is assumed to be sufficient as a result of the engineering controls (positive air pressure, increased air changes, temp and humidity control and high efficiency particulate air filter or HEPA).18 However, it has been demonstrated that those controls can be defeated by door openings and room traffic during cases.19-21
Adjunctive Air Decontamination Technology
Technologies designed to improve air quality in operating rooms fall into three primary categories – air filtration, air disinfection and combined filtration plus disinfection. This adjunctive technology is arguably most crucial in the outer area of the OR beyond the OR table, which is protected with directional air flow and HEPA air filtration. In this outer area of the OR, there is typically less effective air flow, increased human activity, door openings and floor contamination. Consequently, the air in this surrounding area can potentially contaminate instrumentation, implants, gloves, surgical team members, surgical drapes, and tables which are in direct communication with the patient. Employing an adjunctive technology for the outer area of operating rooms, which provides air disinfection plus filtration of particulates, would seem prudent. Innovative portable devices which combine ultraviolet (UV) technology and HEPA filtration to eliminate particulates and microorganisms are in use in increasing numbers of ORs. These devices have been reported in peer reviewed studies to reduce transiently air bacteria in operating rooms by 50 percent to 60 percent and reduce overall rates of prosthetic joint infection (p<0.042).22-29
TO VIEW "REDUCED OCCURRENCES OF PJI" TABLE CLICK ON THIS LINK: PJI table
Conclusions
Current standard methods for ensuring adequate OR air quality are limited to positive air pressure, 20 air changes per hour, surgical attire, traffic control (and HEPA filtration in some ORs). These methods alone have been proven insufficient to prevent contaminated air associated SSI as demonstrated by multiple outbreaks including the M. chimera outbreak in cardiac surgery associated with heater cooler devices. Air decontamination technology (UV + HEPA) can serve as an adjunct to standard methods for ensuring safe air quality for ORs, especially where implant procedures are performed.
Sue Barnes, RN, CIC, FAPIC is an independent clinical consultant, Board certified in Infection Control and Prevention, a Fellow of APIC (FAPIC) and co-founder of the National Corporate IP Director Network. She currently provides marketing and clinical consultation to select industry partners who seek to support infection prevention with innovative products. Disclosure: The author provides consulting services for Aerobiotix, Inc.
References:
- Petrova OE and Sauer K, Sticky situations: key components that control bacterial surface attachment. J Bacteriol, 2012. 194(10): p. 2413-25.
- Zimmerli W, Trampuz A, Ochsner P. Prosthetic-Joint Infections. N Engl J Med. Oct. 14, 2004; 351:1645-1654.
- Kurtz SM, Economic burden of periprosthetic joint infection in the United States. J. Arthroplasty 2012.27:61-65.e61.
- Total Hip Replacement - Information from American Academy of Orthopedic Surgeons. Accessed at: https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/.
- Parisi TJ. What is the Long-term Economic Societal Effect of Periprosthetic Infections After THA. Clin Orthop Relat Res. April 7, 2017.
- Tande AJ, Patel R. Prosthetic Joint Infection. Clinical Microbiology Reviews. 2014;27(2):302-345. doi:10.1128/CMR.00111-13.
- Eickhoff, T. C. (1994). Airborne nosocomial infection: a contemporary perspective. Infect Control Hosp Epidemiol. 15(10): 663-672.
- Durmaz G et al. The relationship between airborne colonization and nosocomial infections in intensive care units Mikrobiyol Bul. 2005 Oct;39(4):465-71.
- Kowalski W. Ultraviolet Germicidal Irradiation Handbook. Springer Verlag, Berlin 2009. pp 399-418.
- Owers KL, James E, Bannister GC. Source of bacterial shedding in laminar flow theatres. J Hosp Infect. 2004 Nov;58(3):230-2.
- Stein R. Super-spreaders in infectious diseases. International Journal of Infectious Diseases. Vol 15 (2011) e510-e513.
- Mora M, Mahnert A, Koskinen K, Pausan MR, Oberauner-Wappis L, Krause R, et al. Microorganisms in Confined Habitats: Microbial Monitoring and Control of Intensive Care Units, Operating Rooms, Cleanrooms and the International Space Station. Front Microbiol. 2016;7:1573.
- Hardin W. and Nichols R. (1995). Aseptic Technique in the operating room. Surgical Infections. D.E. Fry, Ed., Little Brown & Company Boston 109-117.
- Qing-Zeng C, Yun-Bo S, Shi-Hai L, et al. Outbreak of Infections Caused by Group A Streptococcus after Modified Radical Mastectomy. Surgical Infections. 2013;14(4):385-388.
- Van Ingen J et al. Global outbreak of severe Mycobacterium chimaera disease after cardiac surgery: a molecular epidemiological study. Lancet Infect Dis. 2017 Oct;17(10):1033-1041.
- Balsam LB et al. Mycobacterium chimaera left ventricular assist device infections. J Card Surg. 2017 Jun;32(6):402-404.
- ISO documents (n.d.) https://www.terrauniversal.com/cleanrooms/iso-classification-cleanroom-standards.php.
- ASHRAE 170: https://www.techstreet.com/ashrae/standards/ashrae-170-2017?gateway_code=ashrae&product_id=1999079
- AORN Recommended Practices for Traffic Patterns in the Perioperative Practice Setting. AORN Journal. March 2006. Vol. 83, No. 3, Pages 681-684, 686.
- HICPAC Guidelines for Environmental Infection Control in Health-Care Facilities. MMWR June 6, 2003 / 52(RR10);1-42.
- Lynch R et al. Measurement of Foot Traffic in the Operating Room: Implications for Infection Control. Am J Medical Quality. Vol. 24, No. 1, Jan/Feb 2009.
- Bischoff W et al. Impact of a novel mobile air purification system on the bacterial air burden during routine care. Oral presentation SHEA Conference. Spring 2018.
- Curtis G et al. Reduction of particles in operating room using UV air disinfection and recirculation units. Journal Arthroplasty. (2017) 1-5.
- Davies GS, Bradford N, Oliver R, Walsh WR. The effects of a novel decontamination-recirculating system in reducing airborne particulate: A laboratory-based study. Oral presentation: The European Bone & Joint Infection Society Conference. Sept 7-9, 2017.
- Gannon C et al. Reduction of total and viable air particles in the OR setting by using ultraviolet in-room air disinfection and recirculation units. American Association of Hip and Knee Surgeons Conference. Nov. 4, 2017.
- Kirschman D, Eachempati S. Airborne bacteria in the operating room can be reduced by HEPA/Ultraviolet air recirculation system (HUAIRS). Presented at the Surgical Infection Society (SIS) 37th annual meeting. May 2-5 2017.
- Messina G et al. A mobile device to reduce airborne particulate and prevent surgical site infections. European Health Association Conference. Nov. 20-23, 2019.
- Parvizi J et al. Environment of care: is it time to reassess microbial contamination of the operating room air as a risk factor for surgical site infection in total joint arthroplasty? Am J Infect Control. 2017 Nov 1;45(11):1267-1272.
- Walsh WR et al. The Effect of a Novel Air Decontamination Recirculation System on Viable Airborne Particulates. Oral Presentation European Bone and Joint Infection Society (EBJIS) 36th annual meeting. September 7-9 2017.
10 Commonly Asked Questions Relating to Environmental Hygiene
By J. Darrel Hicks, MREH, CHESP
This column originally appeared in the February 2020 issue of Healthcare Hygiene magazine.
1: To what extent does the environmental surfaces cleaning affect contamination levels in hospitals?
The role of the hospital environment as a reservoir of infection is poorly understood. But this is certain; one well-trained hygiene specialist (housekeeper or environmental services professional) can prevent more disease transmission than a room full of doctors can cure.
2: Is there a way to measure the efficacy of a cleaning program?
There are four ways to measure the efficacy of a cleaning program. They are: (A) Visual assessment-not a reliable indicator of surface cleanliness. (B) ATP bioluminescence-measures organic debris (each unit has own reading scale) will give you a reading within seconds. (C) Microbiological methods-can be costly and pathogen specific. (D) Fluorescent marker to ensure that cleaning processes have been adequately performed.
3: What is the difference between disinfectants and sanitizers?
Sanitizers can be used in cafeterias, kitchens and food preparation surfaces to keep certain (short list) microorganisms at a safe level. But, if you want those same microorganisms ELIMINATED, you would need to use a disinfectant such as a quaternary ammonium compound (quat), phenolic, accelerated hydrogen peroxide or other the U.S. Environmental Protection Agency (EPA)-registered disinfectant.
4: Knowing that surfaces nearest the patient harbor the greatest number of pathogens, what is the best method to reduce or eliminate those pathogens?
Washing or scrubbing a surface physically removes soil and organic material such as blood and body fluids and takes with it the disease-causing pathogens. The guiding principle is always to remove germs, if possible, rather than kill them, and then when necessary, use the least amount of the mildest chemical that will do the job, because stronger often means more toxic to people.
5: Is microfiber that much better than cotton when it comes to mops and cloth wipers?
Yes. Microfiber helps physically remove the food and moisture necessary for microorganisms to survive, but better grades of microfiber (those with very dense weaving and fiber configuration) can even remove large quantities of microbes, including hard-to-kill spores.
6: Is it necessary to disinfect floors in hospitals?
A: Floors aren’t a high-touch surface, but some cleaning professionals and healthcare experts suggest that they should be included in disinfection processes. The other school of thought is to simply use a neutral floor cleaner since floors are quickly re-contaminated as soon as somebody walks on them or something is dropped on them.
7: How long must a surface, wetted with disinfectant, remain wet?
This question deals with exposure time or contact time. Each disinfectant has a label with directions for contact time. The U.S. Centers for Disease Control (CDC) guideline recommends a contact time of 1 minute at a minimum. If the label states different contact times for different organisms, the highest contact time listed must be used because one doesn’t know the contents of the soil being cleaned.
8: Is it possible to perform ‘green disinfection’?
Disinfectants -- used properly and wisely -- are designed to protect public health. In many situations—and especially in healthcare and other critical facilities—there is no substitute for disinfectant cleaning. That being said, there are some old technologies (i.e., copper or silver impregnated surfaces, steam vapor devices, spray-and-vac technology) and some new, emerging technologies that hold great promise (i.e., UVC (short wave or germicidal light) photons damage DNA and Hydrogen Peroxide (HP). Both UVC and HP technologies are meant to supplement, not replace routine disinfection.
9: What are “superbugs” and why should we be concerned about them?
Some pathogens have gotten the reputation for being “superbugs” because of their ability to survive on environmental surfaces for up to 56 days after contamination on common hospital materials. Methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococci (VRE) are two of the most talked about “superbugs” that have been implicated in transferring from hospital surfaces to previously uninfected patients.
10: Is it true that quats (quaternary ammonium disinfectants) are inactivated by cotton mops and cloths?
True, once cotton mops or wipers are introduced into a fresh solution of quat disinfectant, the cotton binds the available, active ingredients of the disinfectant within minutes. To avoid this, use a synthetic microfiber cloth or man-made spun material (no cellulose) in quat disinfectants.
J. Darrel Hicks, BA, MREH, CHESP, is the owner/principal of Darrel Hicks, LLC and the author of the book Infection Prevention for Dummies. He is also a board member of the Healthcare Surfaces Institute.
Moving Out of the Cul-de-sac
J. Darrel Hicks, MREH, CHESP
This column originally appeared in the January 2020 issue of Healthcare Hygiene magazine.
For more than 50 years, I’ve lived in suburbs where cul-de-sacs abound. City designers abandoned dense urban grids for garden communities with meandering streets and cul-de-sacs in the 1930s. These new cul-de-sac neighborhoods were thought to be safer and more private alternatives to the pollution, poverty and overcrowding of traditional cities.
For the past four months I’ve been working as the interim environmental services director in a hospital in California. One of my frustrations has been in getting the infection control committee’s approval of a new EPA-registered disinfectant. In tandem with the new disinfectant, I was seeking approval of a total room disinfection technology.
In the past two years before my arrival, the infection control committee approved a hospital-wide disinfectant with a tuberculocidal claim that meets OSHA’s bloodborne pathogen standard for disinfecting surfaces contaminated by blood or other potentially infectious materials. The product must remain wet for 5 minutes. But, for all contact-isolation rooms, a product that requires 3 minutes of contact on pre-cleaned surfaces is used.
Currently, the infection control committee is living happily on the cul-de-sac where it is safe to the through traffic. The cul-de-sac is where the kids can safely play in the circle and neighbors get to have the occasional “block party.” But the cul-de-sac is not where new and better solutions to the problems the hospital faces lives.
The “cul-de-sac” mentality is not isolated to a hospital in California. This mentality thwarts new and innovative products and processes from improving environmental hygiene. Decision-makers and stakeholders too often hide behind questions such as “Who else is using it?” and “What does it kill?” or make statements such as “We don’t switch disinfectants unless there’s a problem that isn’t being addressed.”
It’s at this juncture that feels like quitting this pursuit for a “better, more efficacious” way of room disinfection. Instead of quitting, entrepreneur Seth Godin says, “One should rededicate or try ‘an invigorated new strategy designed to break the problem apart.’”
Godin goes on to say, “I like to call this the pivot. It's an adjustment, a strategic relocation, a change in direction that you make while keeping your eye on your goal. You're like an airplane making constant course corrections until it reaches its final destination.”
I will continue building a relationship with the infection control nurse and infectious diseases physician to identify areas of common agreement. I will implement new and better cleaning and disinfection tools for the EVS staff to more thoroughly clean the patient’s room. Education and retraining will get done in short order. And, I’ll work with the infection control nurse on doing fluorescent marking of rooms before daily or terminal cleaning. This will allow us to begin building data and confidence in “the program” that will ultimately take us off the cul-de-sac and onto the interstate of better outcomes.
Check your calendar. It’s not only a new year, but it’s a new decade, too.
If you find yourself or your organization comfortably living on the cul-de-sac while infection rates remain stagnant and patient satisfaction scores are slightly above the 50th percentile, perhaps it’s time to move out of the cul-de-sac and onto the interstate.
J. Darrel Hicks, BA, MREH, CHESP, is the owner/principal of Darrel Hicks, LLC and the author of the book Infection Prevention for Dummies. He is also a board member of the Healthcare Surfaces Institute.
Hand Grenades and Horseshoes
By J. Darrel Hicks, BA, MREH, CHESP
This article originally appeared in the December 2019 issue of Healthcare Hygiene magazine.
Few people remember that it was baseball great Frank Robinson who first said, "Close don't count in baseball. Close only counts in horseshoes and hand grenades." The quote appeared in Time magazine (July 31, 1973). But what does that phrase mean? It means that the world is usually binary -- you win/you lose, you hit/you miss. If you lose a baseball game 12–11, you only lost by one run, but you lost. Think of “Close but no cigar.” This phrase gives an example of being close and uses alliteration at the same time.
In order for a chemical to claim disinfection it must attain a 6-log reduction of specific organisms, in a prescribed amount of time. While sterilization means at least a 6+ log reduction while leaving no growth or viable survivors.
It is important to understand what log reduction is and why it is important to the process of surface disinfection, surface sterilization and surface decontamination. Scientists and other professionals who are responsible, or even legally responsible, for preventing illness and contamination are concerned with log reduction or elimination of pathogenic bioburden.
The term “log” is short for logarithm, a mathematical term for a power to which a number can be raised (e.g., using 10 as the given number, a log-2 increase can be shown as 10ˆ2 or 10 x 10=100). Alternatively, a log reduction is taking the power in the opposite direction. For example, a log reduction of 1.0 log is equivalent to a 10-fold reduction. Or, stated another way, moving down one decimal place, a 90 percent reduction.
Healthcare surfaces can be contaminated with pathogenic organisms (bioburden), and only achieving a log reduction below 6-log means dangerous viruses, bacteria, fungi and Clostridium difficile (C. diff) spores can or will survive and repopulate surfaces within the treated area. The literature has shown that bioburden can be spread around to contaminate patients and/or grow new bacterial and fungal colonies on new surfaces.
A disinfectant kills microbes; however, depending on the pathogen, preventing the microbes from getting a foothold by removing food and moisture (two essentials for sustaining living organisms) may, in the long-term, be as effective as a chemical disinfectant. In fact, most chemical disinfectants can’t do their job when greater than 5 percent organic soil is in the way. Soil can absorb the active ingredient, provide more places for the germs to hide, and change the chemical nature of the disinfectant.
The number of bacterial survivors is very important because they can quickly increase their populations exponentially/logarithmically. For example, Staphylococcus aureus (under ideal conditions) doubles in 24-30 minutes. This means 1,000 or 10ˆ3 or Log 3, bacterial survivors would increase to 2,000 after 30 minutes, after 60 minutes they would increase to 4,000, after two hours to 16,000 and then increase to over one million after 5 hours or more if the growing environment is right.
When it comes to disinfection of environmental surfaces, close doesn’t count. Not only do “Survivors” replicate quickly and efficiently, but they can also become resistant to disinfectants. To improve outcomes of room disinfection, disinfectants should only be applied to pre-cleaned surfaces according to the Environmental Protection Agency (EPA) and the Centers for Disease Control and Prevention (CDC). These agencies require that any hospital cleaning process that claims efficacy against C. diff spores must achieve no growth, which means no survivors that can multiply and create new bacterial colonies.
There is nothing about the EPA’s use of the AOAC Use-Dilution Test. The AOAC Use-Dilution Test is far removed from "real-life" use of disinfectants. The most glaring separation from "real life" product usage is that contaminated surfaces are submerged in excess disinfectant for the entire contact time (up to 10 minutes). Add to that the fact that sterile water is used for application of the disinfectant. The role of professional cleaning staff in hospitals is dependent on the best disinfectant products that have been vetted in real world conditions of damaged furniture and finishes, water hardness, and education about the prevention and transmission of disease. That’s the challenge confronting the environmental services department.
In closing, if the healthcare surfaces are to be safe, clean and disinfected, we must have better products, processes and staff education about their role in infection prevention. Being “close” just isn’t good enough.
Darrel Hicks, BA, MREH, CHESP, is the owner/principal of Darrel Hicks, LLC and the author of the book Infection Prevention for Dummies. He is also a board member of the Healthcare Surfaces Institute.
Challenging Variation of Hospital Cleaning with a Simple Four-Step Protocol
By Kelly M. Pyrek
This article originally appeared in the November 2019 issue of Healthcare Hygiene magazine.
Variation in environmental hygiene interventions is compounding the challenge of understanding the potential impact that cleaning and disinfection has on infection rates.
While recommendations exist, mainly in the medical literature as well as from professional organizations, there is not one single, standardized protocol for U.S. hospitals.
“There is no accepted cleaning protocol because there is still insufficient evidence for healthcare cleaning and how it should be done,” says Stephanie J. Dancer, BSc, MB BS, MSc, MD, FRCPath, DTM, a medical microbiologist at NHS Lanarkshire and professor of microbiology at Edinburgh Napier University in the UK. “It is difficult to agree a universal process without a robust evidence base. The current debate is skirting around the edges by arguing over cleaning and/or decontamination methods and risk assessment of specific patient areas.”
Dancer adds, “Cleaning is not sexy; it is underpaid, undervalued and viewed through a prism of social class. There is little commitment to produce standardized guidelines, particularly if implementation is going to cost more. People who could make it happen do not understand the importance of cleaning because they may not have had to do it for themselves.”
Variability in cleaning practices is problematic, Dancer says, because “Different methods, types, application and frequencies of cleaning destroy any chance of collating scientific evidence. In addition, cleaners are people who will clean differently every shift depending on how they feel. Cleaners cannot be standardized. Nor should they be.”
One might think that basic guidance for environmental cleaning and disinfection could be construed as naïve in this age of sophisticated interventions, but as Dancer and Kramer (2018) emphasize, “repeated application of a sequential cleaning system would offer a time-efficient and effective method for decontaminating a bed space in the healthcare environment.”
They add further, “It is already known that surfaces are regularly missed during cleaning, and that time spent cleaning does not correlate with thoroughness of cleaning. Cleaning an area in a methodical pattern establishes a routine so that items or areas are not missed during the cleaning process. A practical guideline would improve cleaning of high-risk near-patient sites and could impact on HAI risk. Secondly, an explanatory guide would help cleaning staff to understand what they should do, when they should do it, and why they should do it. The principles focus on the occupied bed space because a vacant bed space receives so-called ‘terminal’ or ‘discharge’ cleaning, for which there is already comprehensive guidance. An unoccupied bed space is easier to clean as it lacks patient, visitors, clinical equipment and personal belongings. However, while there remains a small HAI risk for cleaning staff from the terminally cleaned bed space, the risk is arguably greater with a patient in situ. Patients themselves continually touch high-risk sites, without hand hygiene reminders or opportunities.”
Lack of compliance with infection prevention practices in hospitals is well documented in the literature and can be explained away by everything from deficits in resources, to time pressure and gaps in healthcare personnel knowledge about the imperatives of environmental hygiene. Barriers to optimal practice must be overcome, Dancer says, but consensus is lacking as to how precisely that can be achieved.
“The most intractable barrier to implementing a standardized protocol (other than lack of evidence) is usually due to lack of managerial commitment and support,” she says. “In addition, cleaning staff require a salary and more resources might be needed for a new cleaning process. Plus, no agreement on methods means that consumable costs could terminate any willingness to restructure the cleaning service. How do hospitals in low income countries afford expensive disinfectants or automated devices?
Dancer continues, “Another barrier is the fact that it is difficult to measure both the cleaning process and surface cleanliness. Even monitoring the impact of a cleaning intervention by using patient parameters such as hospital-acquired infection (HAI) is challenging. This is because there are multi-factorial reasons for HAI occurrence outside the outbreak situation. So, hospital authorities cannot easily audit the benefits from their newly implemented universal cleaning protocol.”
To help address the lack of standardization, Dancer and Kramer (2018) outlined a systematic process by which each component of environmental hygiene is placed within an evidence-based and ordered protocol. But when conducting their literature search, the authors hit a barrier of their own – they could not identify any papers providing an evidence-based practical approach to systematic cleaning in hospitals, and therefore proposed their own, simple four-step guide for daily cleaning of the occupied bed space.
Their schematic is as follows: Step 1 (LOOK) describes a visual assessment of the area to be cleaned; Step 2 (PLAN) argues why the bed space needs preparation before cleaning; Step 3 (CLEAN) covers surface cleaning/decontamination; and Step 4 (DRY) is the final stage whereby surfaces are allowed to dry.
That the protocol has only four steps is by design, Dancer says, to help overcome challenges relating to the overall complexity of cleaning disinfection tasks, the skill and comprehension levels of environmental services professionals, and the immense pressure of room-turnover times.
“Why not keep it simple,” Dancer emphasizes. “Domestic workers clean because they need a job; and/or may not have the qualifications to do anything else. So, a four-step protocol is more easily assailable; easier to teach; easier to monitor; easier to understand. Cleaners might not speak the language of the country in whose hospitals they are working, and a practical four-step process could be transmuted into a visual guideline with pictures, diagrams and photographs to explain each step.”
She continues, “People need to know exactly what they have to do; how they should do it; where and when they should do it; how often they should do it; and what the risks are, for themselves as well as patients. They also need to know the value of what they do, even if this does not translate into a generous pay packet. In addition, standardization of the process lends itself to monitoring and feedback, both of which guarantee a better outcome.”
As Dancer and Kramer (2018) observe, “Cleaners themselves receive little or no training for what they do, and any teaching initiatives may be compounded by time, language and literacy problems. Universally poorly paid, they are expected to perform a physically arduous and repetitive job with additional personal risks from cleaning materials as well as exposure to infected patients. Cleaning staff would likely welcome a systematic aid to good practice with in-built risk assessment for themselves, as well as staff and patients.”
The four-step guide proposed by Dancer and Kramer (2018) targets primarily environmental services personnel rather than nursing staff, and as such prioritizes bed-space items and furniture and not clinical equipment.
Let’s examine each of the four steps:
Step 1: LOOK
The process begins with a visual assessment. As Dancer and Kramer (2018) advise, “Every cleaner should inspect the area to be cleaned and consider overall conditions and degree of visual contamination before beginning a cleaning task.”
Step 2: PLAN
This step explains why and how the area to be cleaned needs to be prepared for cleaning. Healthcare environmental services staff should survey the area to be cleaned, ascertaining the most appropriate level of cleaning, what should be cleaned and how, and being sure to use the proper tools and cleaning/disinfection chemistries.
Step 3: CLEAN
As Dancer and Kramer (2018) explain, “Cleaning refers to the removal of soil from surfaces by use of physical wiping or scrubbing; the chemical action of a surfactant or detergent; and water to wet, emulsify or reduce surface tension. The process removes both dirt and microorganisms from surfaces, thereby reducing the amount of organic bioburden. Cleaning should always precede disinfection because the presence of soil will impede disinfectant activity. Some hospitals use detergents for routine cleaning, while others choose products that either inactivate or kill living microorganisms. This is termed ‘disinfection’ or ‘hygienic’ cleaning … Cleaning and disinfection become inextricably intertwined when wipes are impregnated with disinfectant as the overall effect is a combination of disinfectant activity and physical removal of soil.”
They emphasize some of the best practices relating to cleaning and disinfection:
- Clean from high to low, then clean sites nearest to the patient first, then sites furthest from the patient (e.g. door handle, sink, bathroom.
- Make high-touch/ hand-touch sites a priority.
- Clean a site from least visually dirty to obviously dirty.
- Wipes should be used according to manufacturers' instructions. Use one wipe for each site; some sites may require several wipes (e.g. bed frame). Unfolding the wipe and using it flat on the surface maximizes the area cleaned and minimizes the amount of hand contact. Wipe in one direction without retracing the area already cleaned; apply the ‘one wipe; one site; one direction’ principle.
- Be aware that microbes may be transferred between surfaces (via gloved hands, cloths, etc.)
- Always remove visible soil with detergent and water before the use of disinfectant.
- The physical removal of soil and microbiocidal activity from disinfectant may be achieved by use of a disinfectant-containing wipe.
-The researchers emphasize, “Sites such as bed rails, bed control (if electric-bed), nurse call bell, bedside locker and bed table constitute the highest priority for cleaning because they are frequently touched and readily provide a reservoir for hospital pathogens. There is a two-way direction of transmission between these surfaces and hands, which can only be disrupted by targeted cleaning and hand hygiene. Given that cleaning usually occurs just once per day, and hand hygiene depends on a multitude of factors, it comes as no surprise that infections are readily acquired from bed-space sites.
Step 4: DRY
The final stage encompasses physical drying of surfaces. As Dancer and Kramer (2018) note, “The cleaning process is not complete until all surfaces are completely dry. Contact time is usually considered critical to disinfection, but it can be difficult to fulfill in a time-pressured healthcare environment.” They add, “This fourth stage should also include the cleaner's own assessment as to overall cleanliness of the bed space or room. If they are satisfied that the process is complete, the area can be signed off verbally or by written notification, labeling or use of a checklist. Further monitoring helps to maintain, and improve, the quality of cleaning but it is not necessarily mandatory and will depend upon available resources …When leaving the patient area, the gloved hand should be subjected to hand disinfection if the cleaner has to fulfill further duties before the next cleaning objective. Otherwise, gloves and any other protective apparel may be removed, and hands washed and dried before further duties.”
Reference: Dancer SJ and Kramer A. Four steps to clean hospitals: LOOK, PLAN, CLEAN and DRY. J Hosp Infect. December 2018.
From Wheels Up, To Wheels Down
By J. Darrel Hicks, BA, MREH, CHESP
This column originally appeared in the November 2019 issue of Healthcare Hygiene magazine.
As I sat buckled into my seat ready for takeoff, one of the cockpit officers was making his usual announcements, and then said, “It’ll be three hours and five minutes from wheels up to wheels down in St. Louis.”
One can’t help but wonder, “How can he be so precise? How does he know exactly how long it’ll take?”
In the business of cleaning and disinfecting the patient-care environment, the environmental services (EVS) department is asked to perform processes that change a “soiled” room into a “patient-ready” room.
Perhaps the soiled room was a Trauma Room in the Emergency Department that just treated a victim of a car accident. Or, the 500 sq. ft. surgical suite that was used to do a quadruple bypass on person who suffered a heart attack.
The process has different names depending on where the soiled room is. Names such as “turnover,” “between-case-cleaning,” “terminal cleaning,” or “end-of-day cleaning.” But the most important thing to know about the “process” is, this is the best opportunity to break the chain of infection from one patient to the next.
An EVS worker who is educated about infection prevention, equipped with the right products and processes, and given enough time for the task, will prevent more infections than a room full of doctors can cure.
The process involves using a clean, micro-denier cloth and the hospital-approved disinfectant to remove the bioburden and disinfect the surfaces that are wiped. Do you know how long the process will take?
The co-pilot seemed to know how long it would take to travel from San Jose to St. Louis. To process a patient’s room where the occupant with Clostridium difficile stayed for 24 days, does it take 35, 45 or 55 minutes? Is the process the same for an isolation room as the trauma room or the operating room? Are these processes defined? Are they the same in every hospital? Are there benchmarks for how much time to allow for each situation?
Let’s assume for the moment that the national benchmark states that the terminal process for the isolation room should take 55 minutes. Is the national benchmark 55 minutes still in play when the charge nurse says, “This room is a STAT! Hurry up, the ER patient is on the way”? Would you put your mother in a STAT room that was improperly processed by an EVS technician who spent 30 minutes in the room.
When time is placed above patient safety in turnovers, terminal cleanings, and between-case cleanings, the chain of infection may remain unbroken. As leaders in environmental services, risk management and infection prevention, we need to speak with one voice for the safety of patients who are undeserving of a healthcare-acquired infection (HAI).
To be sure, we should use the tools at our disposal to ensure that we are working efficiently. Some of those tools include:
- Checklists (there are some good ones available, but some are so long they are unrealistic)
- Team cleaning (identify what needs to be processed, use color coding so each team member knows what their responsibility is)
- Observations by leaders (environmental services or nursing)
- Competency assessments
- Measuring the effectiveness of people, products and processes
By the way…the co-pilot was right. We landed three hours and five minutes from wheels up to wheels down.
- Darrel Hicks, BA, MREH, CHESP, is the owner/principal of Darrel Hicks, LLC and the author of the book Infection Prevention for Dummies.
A Carrier Platform to Test Microbial Decontamination of High-Touch Environmental Surfaces by Wiping
By Syed A. Sattar, PhD; Bahram Zargar, PhD; and Saeideh Naderi, PhD
This article originally appeared in the October 2019 issue of Healthcare Hygiene magazine.
Introduction
High-touch environmental surfaces (HITES) can spread pathogens in healthcare and other settings (Carling 2016, Weber et al., 2013), and wiping is crucial for HITES decontamination except with no-touch technologies. However, routine decontamination by wiping remains suboptimal (Carling 2016; Sattar and Maillard 2013) and may spread pathogens over a wider area (Ramm et al. 2015). In addition, methods for pre-market testing of environmental surface disinfectants are either qualitative or devoid of any wiping action (Sattar 2010). We report here a quantitative and ‘dynamic’ (combining the physical and chemical action of wipes) test protocol to better reflect the field use of disinfecting wipes.
Materials and Methods
Acinetobacter baumannii (ATCC 19606), a common healthcare-associated pathogen (Howard et al., 2012), was used for the testing. Trypticase soy broth (TSB) and Trypticase soy agar (TSA) were used, respectively, to grow (20±2 h) and recover (48±2 h) it from the test and control samples at 36±1°C.
A Teflon-based platform with perforations (Figure 1; 30.0 cm x 60.0 cm x 0.5 cm) held nine sterile disks (1 cm in diam.) of brushed stainless steel (AISI 430) as archetypical hard, non-porous HITES. The platform was sterilized by autoclaving. Each sterile disk on one platform received 10 µL of the microbial suspension in a soil load (Sattar et al. 2007) and the inoculum dried. To maintain a uniform pressure during wiping, the operator first practiced the wiping with the platform placed on a digital read-out scale. The platform was then wiped with either Product A (2,600 ppm quaternary ammonium compound; (QAC) or Product B (250 ppm sodium hypochlorite (SH) at neutral pH; Product C, the control, was a microbicide-free fabric (J-Cloth; E.D. Smith Foods, Ltd.) dampened with normal saline with a detergent (0.1% polysorbate-80). The used wipe was immediately applied on another platform with clean disks to assess transfer of any viable organisms.
A custom-built retriever simultaneous collected the disks from a given platform into separate vials with 10 mL of an eluent/neutralizer in each. The eluates were individually membrane-filtered (0.22 µm pore diam.) and each filter placed on a TSA plate to recover colony-forming units (CFU) and calculate log10 reductions. Each type of wipe was tested three times under ambient conditions (RH at 45±5%; air temp. 22±2°C). After wiping, the platforms were left undisturbed for 5 minutes.
Results
As shown in Table 1, Product A reduced the contamination by >4 log10 (>99.99%) with virtually no detectable transfer of CFU to clean disks. This suggested that the contamination was either inactivated or sequestered in the applicator itself. Product B achieved a >2 log10 (>99.00%) reduction in the viability of the test microbe while transferring a higher level of CFUs as compared to Product A. Product C (J-Cloth) achieved <1 log10 (<86.2%) reduction in the test microbe’s viability while transferring >1% of the contamination. In this instance, the reduction in the level of viability was entirely due to mechanical removal of the contamination. The level of transfer from the control fabric was also higher due to the absence of any microbicidal activity.
The concentration of SH (neutral pH) in this study was kept deliberately low to enhance workplace safety while also reducing the chemical loading of the environment. Higher levels of SH would most likely perform as well as the QAC-based wipe.
Discussion
QACs and SH continue to be among the most common microbicides in HITES wipes. However, their respective concentrations in prewetted wipes can vary widely along with the nature of the applicator itself. In the case of the SH-based wipe tested in this study, the fabric was a microfiber cloth as supplied by the wipe manufacturer.
The results showed the ability of the platform to assess HITES decontamination as well as the ability of the used wipes to transfer contamination to clean surfaces. Predictably, such microbial transfer was the highest with the control wipe wetted with a buffer.
The platform and the disk retrieval system are simple, generic in design, and capable of handling most types of HITES as well as all major classes of human pathogens known to spread via HITES.
The findings reported here further reinforce the applicability of the platform in assessing disinfecting wipes in a field-relevant manner. The platform can not only test prewetted wipes but also spray-and-wipe systems. Teflon was chosen to make the platform for its high heat- and chemical-resistance as well as easy cleanability between uses.
With additional experimentation using a wider variety of pathogens and wipe technologies, the system has the potential to become an international standard, such as that for ASTM International (www.astm.org).
Acknowledgements
This study was supported in part with funding from the Healthcare Surfaces Institute (www.healthcaresurfacesinstititute.org).
References:
ASTM International (2011). Standard quantitative disk carrier test method for determining the bactericidal, virucidal, fungicidal, mycobactericidal & sporicidal activities of liquid chemicals (E-2197-11). ASTM, West Conshohocken, Penn.
Carling PC. (2016). Optimizing Health Care Environmental Hygiene, Infect Dis Clin North Am. Sept; 30(3):639-660.
Howard A, O’Donoghue M, Feeney A and Sleator RD. (2012). Acinetobacter baumannii, an emerging opportunistic pathogen. Virulence. 3(3): 243-250.
Ramm L, Siani H, Wesgate R, Maillard J-Y. (2015). Pathogen transfer and high variability in pathogen removal by detergent wipes. Am J Infect Control. 43(7):724-728.
Sattar SA and Maillard J.-Y. (2013). The crucial role of wiping in decontamination of high-touch environmental surfaces: review of current status and directions for the future, Am J Infect Control. May; 41(5 Suppl):S97-104.
Sattar SA. (2010). Promises & pitfalls of recent advances in chemical means of preventing the spread of nosocomial infections by environmental surfaces. Am J Infect Control 38: S34-S40.
Springthorpe VS and Sattar SA. (2007). Application of a quantitative carrier test to evaluate microbicides against mycobacteria. J. AOAC Int. 90:817-824.
Weber DJ, Anderson D, Rutala WA. (2013). The role of the surface environment in healthcare-associated infections. Curr Opin Infect Dis. 26(4):338-344.
Table 1. Summary of data on the quantitative assessments of CFU reductions and transfer of Acinetobacter baumannii by three types of wipes using a platform developed at CREM Co Labs.
Test # % Reduction % Transfer Mean Percent ±
Standard Deviations
Reduction Transfer
Product A
1 99.9994 0.00058 99.994± 0.0085 0.0095± 0.0083
2 99.9844 0.011
3 99.998 0.017
Product B
1 98.78 0.086 99.318± 0.5038 0.0490± 0.0317
2 99.39 0.032
3 99.78 0.030
Product C (control)
1 92.65 1.350 86.242±12.1884 1.075±0.5313
2 93.88 1.410
3 72.19 0.460
Figure 1:
Stainless steel disks embedded in the contaminated and transfer Teflon platforms being wiped.
Syed A. Sattar, PhD, is professor emeritus of microbiology at the University of Ottawa, Ottawa, ON, Canada, and affiliated with CREM Co Labs of Mississauga, ON, Canada. Bahram Zargar, PhD, and Saeideh Naderi, PhD, are affiliated with CREM Co Labs.

Is It Time to Rethink Air Quality in the OR?
By Kathy Warye
Over the last decade, U.S. healthcare institutions have made significant strides in reducing healthcare-associated infection (HAI) through a combination of vertical strategies, targeted toward the reduction of device or organism specific infection and horizontal strategies aimed at mitigating infection risk across the continuum of care. Strong financial incentives established as part of the Affordable Care Act continue to pressure hospitals to find new ways of reducing HAIs. Despite these measures, HAIs continue to be among the most prevalent and costly adverse events in US healthcare institutions.1
In 2010, Weber, et al. found that in the case of several of the more critical organisms present in hospitals, that patient-to-patient transmission was directly proportional to the level of environmental contamination.2 The emergence of MDROs that persist in the environment, combined with a growing body of evidence correlating contaminated surfaces to HAI, heightened awareness of the environment as a transmission risk in institutions.
As a result, cleaning and disinfection of the patient environment became a core, horizontal infection prevention strategy. The Joint Commission and CMS require hospitals to have rigorous environmental cleaning policies and procedures in place which are subject to routine audit for accreditation. And with this new standard of care, a virtual tsunami of products and services emerged to support these efforts.
Today, the hospital surface disinfectant market alone is projected to be worth $1.2 billion by 2024.
Up to this point, however, infection prevention efforts and investment aimed at reducing the risk of environmental transmission have focused almost exclusively on hard surfaces. With the exception of isolation of patients with serious respiratory infection, hospital air quality has received comparatively little attention. This can be explained, in part, by several factors: Sampling and measurement of viable aerosolized bacteria has been both costly and burdensome. And until recently, there has been an absence of innovation in technology for hospital air quality management. With limited evidence and no new solutions on the horizon, it is understandable that other infection prevention concerns took priority over air.
In the U.S., the importance of airborne transmission to HAI generally is a matter of considerable debate. However, in the case of SSI, there are many reasons why healthcare institutions should consider air quality the next frontier for reduction.
SSIs are complex and multifactorial, yet 30 years of studies demonstrate the contribution of aerosolized bioburden to SSI. As far back as the 1980s, Lidwell found that most bacteria contaminating surgical wounds are likely to have reached it by the airborne route. Whyte found that 98 percent of bacteria in patients' wounds after surgery in a conventionally-ventilated operating room came directly or indirectly from the air.3-4 The recent outbreak of M. chimaera found to be epidemiologically linked to aerosolized bacteria from contaminated heater-cooler units used in cardiac surgery is a more recent reinforcement of the airborne route in SSI.5
While progress has been made in SS reduction, the Agency for Healthcare Research and Quality (AHRQ) reported no decrease, between 2014 and 2017, in a core group of SSIs subject to reporting to NHSN.1 SCIP, SIP and other initiatives aimed at standardization of best practice yielded improvement and new evidence may lead to identification of additional process improvement opportunities, however, the low-hanging fruit in process and practice has likely been harvested.
So, where do we go from here? Rethinking air quality in the OR may be the place to start. Sweden and the Netherlands have promulgated standards in the last two years which limit bacterial colony forming units (CFUs) in key areas of the hospital based on patient risk.6 In the OR, air quality must be maintained at no greater than 10 CFUs per cubic meter (<10CFU/m3). Additional European nations and Australia are considering similar requirements, and the WHO recently issued a conditional recommendation that laminar airflow ventilation systems should not be used to reduce SSI risk for patients undergoing total arthroplasty surgery.7
Requirements for air quality management date to the 1970s and focus on the mechanism of air management not the efficacy of those controls. This is understandable given the absence of innovation in air quality management technology. Since the 1970s, architectural controls have been the only viable approach; however, there is a steady flow of research which calls the efficacy of these controls into question. For example, studies have demonstrated that air exchanges and positive air pressure are easily thwarted by door openings and traffic.9-11
Rethinking OR air quality may be particularly important as the population ages and demand for surgery with implants increases. A recent study predicted exponential growth in total hip and knee arthroplasty (THA/TKA) procedural volume between 2020 and 2030. With no abatement in the rate of infection, by TKA/THA prosthetic joint infections will increase by 14 percent.12
A postoperative infection in a clean surgical wound requires a microbial burden of 105 CFUs, whereas when a foreign body, such as an implant, is present an infection can occur with as few as 10 to 50 CFUs.13-14 A prospective randomized multicenter study showed that joint replacements in rooms with over 50 CFU bacteria were 2.6 times as likely to have postoperative infection than those with 10-20 CFU.15
Infection prevention strategy begins with a risk assessment. Bacterial levels as high as 150 (CFU)/m3 have been documented in U.S. ORs, yet despite the known risk of infection, there is no requirement for bacterial testing or particulate counts in the nation’s operating rooms.16 We have little understanding of the risk or the extent to which air may be undermining our efforts to reduce SSI. New, less costly and easier to use air quality measurement technology is entering the market which will help make routine assessment of aerosolized bioburden viable.
Is it time for the US to consider more rigorous standards of care for air quality in the operating room? While there are considerable open research questions, aerosolized bacteria is a known contributor to SSI. And with process and practice measures exhausted, infection prevention stakeholders must look to other ways of mitigating risk. Ten years ago, environmental disinfection was the new frontier in infection prevention, but air was absent from the scope of that effort. In light of new evidence, new technology and the challenge of achieving further reductions in SSI, infection prevention stakeholders may want to consider broadening the scope of environmental disinfection strategy to OR air quality, gain a better understanding of the level of contamination and relative risk their ORs and embrace the potential of enhanced air management strategies to further protect patients from SSI.
References:
1- 2016 National & State Healthcare-Associated Infections Progress Report, Agency for Healthcare Quality and Research
2- Weber, D., & Rutala, W. (2011). The Role of the Environment in Transmission of Clostridium difficile Infection in Healthcare Facilities. Infection Control & Hospital Epidemiology, 32(3), 207-209. doi:10.1086/658670
3-Lidwell, O.M., Lowbury, E.J.L., Whyte, W., Blowers, R., Stanley, S.J. & Lowe, D.(1983). Airborne contamination of wounds in joint replacement operations: the relationship to sepsis rates. Journal
of Hospital Infection, 4(2),111-131.
4 -Whyte, W., Hodgson, R. & Tinkler, J. (1982). The importance of airbornebacterial contamination of wounds. Journal of Hospital Infection, 3(2),123-135.
5-Sax H, et al, Prolonged Outbreak of Mycobacterium chimaera Infection After Open-Chest Heart Surgery Clin Infect Dis. 2015: 61 (1); 67-75.
6- Swedish Standards Inst., Teknisk specification SIS-TS 39:2015
7- WHO. Global guidelines on the prevention of surgical site infection. Available from: http://www.who.int/gpsc/ssi-guidelines/en/. Accessed February 13, 2017.
8- 31-WHO. Global guidelines on the prevention of surgical site infection. Available from: http://www.who.int/gpsc/ssi-guidelines/en/.
9- Perez, et al, Door openings in the operating room are associated with increased environmental contamination, Am J Infect Control, Volume 46, Issue 8, Pages 954–956
10-Teter, et al, Assessment of operating room airflow using air particle counts and direct observation of door openings, Am J Infect Cont., Volume 45, Issue 5, Pages 477–482
11- Birgand, G., Azevedo, C., Rukly, S., Pissard-Gibollet, R., Toupet, G., Timsit, J., & Lucet, J. (2019). Motion-capture system to assess intraoperative staff movements and door openings: Impact on surrogates of the infectious risk in surgery. Infection Control & Hospital Epidemiology, 40(5), 566-573. doi:10.1017/ice.2019.35
12- Wolford H et al, The projected burden of complex surgical site infections following hip and knee arthroplasties in adults in the United States, 2020 through 2030. Infect Cont Hosp Epi (2018), 39, 1189–1195 doi:10.1017/ice.2018.184
13-Edmiston CE. Prosthetic device infections in surgery. In: Nichols RL, Nyhus LM, editors. Update surgical sepsis. Philadelphia (PA): J.B. Lippincott Co.; 1993.pp. 196-222.
14-Parvisi et al, Environment of care: Is it time to reassess microbial contamination of the operating room air as a risk factor for surgical site infection in total joint arthroplasty? Am J Infect Cont, Vol 45, Issue 11, 1267 – 1272.

The following article is from the Environmental Hygiene column published in the October 2019 issue of Healthcare Hygiene magazine.
Cleaning and Disinfection in the 21st Century
By J. Darrel Hicks
Although cleanliness may be next to Godliness, it's also very closely related to disinfection. In fact, cleaning may avert the need to disinfect in some situations because clean and dry surfaces can't harbor microbial growth for very long.
In view of the evidence that transmission of many healthcare-acquired pathogens (HAPs) is related to contamination of near-patient surfaces and equipment, all hospitals are encouraged to develop programs to optimize the thoroughness of high-touch surface cleaning as part of terminal room cleaning at the time of discharge or transfer of patients. In view of this fact, isn't it time to get rid of Spaulding's classification of those near patient surfaces and equipment as "non-critical"?
Numerous studies have demonstrated the role of the environment as a reservoir and in the transmission of human pathogens. However, the precise role of environmental cleaning and disinfection in preventing acquisition of healthcare-acquired infections (HAIs) is uncertain in part, because of variations in assessment methodology and lack of randomized control studies. This standard relies on the available scientific evidence for effective cleaning and disinfection practices in order to minimize the risk of pathogen transmission to patients and protect patient health.
How do we define "clean" or "cleaning," "disinfection" or "disinfecting" for the environmental services (ES) technician to insure a safe, clean and disinfected environment?
Personally, I prefer the definition that Michael Berry, PhD, promotes for "clean" and "cleaning." Clean is a condition free of unwanted matter that has the potential to cause an adverse or undesirable effect.
Cleaning is the fundamental management process of putting unwanted matter in its proper place to achieve a clean condition. Cleaning professionals will understand these definitions and be able to deliver the desired outcomes.
In my professional opinion, along with "Spaulding's non-critical" classification for near patient surfaces, we need to get rid of the term "visibly soiled." There are more than enough C. difficile spores in the size of a pinhead to transmit the pathogen. When the ES technician is given the instruction to clean "visibly soiled" surfaces, are they looking for soil the size of a pinhead? No, they don't have time...they have eight more patient rooms to clean in the next two hours before they clock out.
Cleaning and disinfection have shown benefits in infection prevention and control, and as the research continues to evolve, more clarity emerges. The challenge to research in this area is the lack of clinical trials. This is further compounded by the difficulty in conducting cleaning and disinfection research clinical trials in healthcare facilities.
The following are the more traditional, time-worn definitions for consideration:
- Cleaning agent — a substance, or mixture of substances, that physically removes foreign material (e.g., dust, soil, food) and patient-derived material (e.g., blood, secretions, excretions, microorganisms) from environmental surfaces and inanimate objects due to the detergent or enzymatic properties of the formulation. See One-Step Cleaning Agent Disinfectant, Detergent.
- Cleaning — the physical removal of foreign material (e.g., dust, soil, food) and patient-derived material (e.g., blood, secretions, excretions, microorganisms). Cleaning physically removes rather than kills microorganisms. It is accomplished with water, detergents and mechanical action.
Notes:
1. The terms decontamination” and “sanitation” may be used for this process in certain settings, e.g., central service or dietetics.
2. Cleaning reduces or eliminates the reservoirs of potential pathogenic organisms. Cleaning agents are the most common chemicals used in housekeeping activity”.
3. Organic material present on objects that are being disinfected can hinder the action of some disinfectants. Gross (visible) contamination on any surface needs to be removed (cleaned) even if using a one-step cleaning agent/disinfectant.
- Contamination — the presence of an infectious agent on hands or on a surface such as clothes, gowns, gloves, bedding, toys, surgical instruments, patient care equipment, dressings or other inanimate objects.
- Decontamination — the process of cleaning, by use of physical and chemical means, to remove, inactivate, or destroy, followed by the inactivation of pathogenic micro-organisms, in order to render an object safe for handling.
- Disinfectant — a substance, or mixture of substances, capable of destroying or irreversibly inactivating pathogenic (disease-causing) and potentially pathogenic (opportunistic) microorganisms, but not necessarily bacterial spores, present on environmental surfaces and inanimate objects due to the antimicrobial action of the active ingredient(s). A disinfectant shall have an EPA registration number.
- Disinfection — the inactivation of disease-producing microorganisms to a level previously specified as being appropriate for a defined purpose on the equipment or surface after the cleaning process has been properly completed. Disinfection does not destroy all bacterial spores. Note: Disinfection typically involves chemicals, heat, ultraviolet light, ozonated water or self-disinfecting materials.
- Environmental services (ES) — the department primarily responsible for the development and implementation of the environmental cleaning and disinfection programs, policies and SOPs for the healthcare facility including but not limited to: environmental surfaces; furniture; mobile shared non-invasive equipment; portable electronic devices; waste management; and the development and applications/inspections of its program operations;
Notes:
1. In general, the healthcare facility ES department has this responsibility -- although other departments and services (e.g., nursing, physiotherapy, dental) -- can also be accountable for following the cleaning and disinfection standards.
2. Environmental services and housekeeping services are often used interchangeably.
- Fomites — inanimate objects in the environment that may become contaminated with microorganisms and serve as vehicles of transmission.
The fact is, surfaces appearing to be clean might not necessarily be clean when scientifically quantified or qualified. Remember, what you can't see, can hurt you. The ES technician should be educated and trained to strive for health-based or hygienic cleaning (cleaning for a healthier environment and not just for appearances). That means cleaning AND disinfecting
A hospital-approved disinfectant kills microbe of importance to a facility. ES leaders should choose disinfectants in concert with infection preventionists, pharmacy leaders and infectious disease physicians.
However, depending on the pathogen, preventing the microbes from getting a foothold by removing food and moisture (two essentials for sustaining living organisms) may, in the long-term, be as effective as a chemical disinfectant. In fact, chemical disinfectants can't do their job when high levels (greater than 5 percent which is required for EPA-registration) are in the way. Soil can absorb the active ingredient, provide more places for the germs to hide, and change the chemical nature of the disinfectant.
Cleaning and disinfection are NOT interchangeable terms, but many treat them as if they were. Cleaning and disinfection are two distinct operations that those doing the daily processing of patient care areas must understand. That's why both the EPA and the CDC guidance calls for the application of disinfectants to pre-cleaned surfaces. A surface that has not been cleaned effectively cannot be said to be properly disinfected.
I'd like to leave you with this truth: One engaged ES technician given the right tools, education and enough time to perform the process of cleaning and disinfection, can prevent more infections than a room full of doctors can cure.
 J. Darrel Hicks, BA, Master REH, CHESP, Certificate of Mastery in Infection Prevention, and a Certified Expert Trainer -- is the owner/principal of Darrel Hicks, LLC. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. Hicks authored Infection Prevention for Dummies, a 43-page, pocket-size book that deals with the role that proper cleaning and disinfection plays in saving lives.
J. Darrel Hicks, BA, Master REH, CHESP, Certificate of Mastery in Infection Prevention, and a Certified Expert Trainer -- is the owner/principal of Darrel Hicks, LLC. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. Hicks authored Infection Prevention for Dummies, a 43-page, pocket-size book that deals with the role that proper cleaning and disinfection plays in saving lives.
“I’m an EVS Technician and I Save Lives…What’s Your Super-Power?”
By J. Darrel Hicks
Environmental Services Week, Sept. 8-14, 2019, is a week to join all national and international healthcare environmental services (EVS) professionals to celebrate the outstanding work of these specialists and teams. Every year this week represents a special opportunity to acknowledge the outstanding efforts of your housekeeping team and thank them for a job well done.
Simple cleaning of the environmental surfaces may be one of the key defenses in the future battle against infectious disease. With antibiotic-resistant organisms proliferating on common touchpoints for up to 56 or more days, the study of cleaning and measuring cleanliness is becoming all-important.
“Compliant cleaning and disinfection of environmental surfaces and medical equipment is a critical first line of defense against all pathogens in the healthcare environment, and especially those that are resistant to antibiotics,” says Sarah Bell-West, PhD, senior scientist at Clorox Healthcare.
EVS workers play an essential role in prevention of healthcare-acquired infections (HAIs). Studies have demonstrated significant improvements in cleaning through interventions directed at environmental services workers. For optimal effectiveness, such interventions require that environmental service workers be knowledgeable about the prevention and transmission of disease and well trained with the best practices that keep patients safe.
When it comes to keeping pathogenic organisms at a safe level on environmental surfaces, the least educated and lowest paid people in the hospital must eliminate those dangerous bacteria.
“This is the level in the hospital hierarchy where you have the least investment, the least status and the least respect,” says Jan Patterson, MD, past-president of the Society for Healthcare Epidemiology of America (SHEA).
It’s time to certify Environmental Service Workers
When hospitals want to compete in their market, leaders often look to the latest 128-slice, 3-D CT scanner, a Divinci robot to perform surgeries, recruit the best surgeon, or begin a new service line with the best return on investment (ROI). While these capital expenditures and improvements might attract publicity for a fleeting moment, the board of directors needs to consider a different, low cost option that provides the best chance to improve patient satisfaction, reduce HAIs and improve the bottom line: The Environmental Services Department.
The literature is replete with articles and studies in infection prevention annals extolling the virtues of various environmental hygiene Products, Processes and Programs to reduce HAIs in healthcare. The one missing “P” is the People who work hard, do a dirty (sometimes disgusting) and repetitive job, and make $10 an hour while providing a safe, clean and disinfected environment for patients and staff; the people of the EVS department.
In an article titled, “Clean Sweep: Hospitals Bring Janitors to the Front Lines of Infection Control” (Aug. 15, 2012 Scientific American), Maryn McKenna wrote, “It hasn’t been that long ago the poster bug for nasty bacteria that attack patients in hospitals was MRSA. Because MRSA clings to the skin, the chief strategy for limiting its spread was thorough hand washing. Now, however, the most dangerous bacteria are the ones that survive on inorganic surfaces such as keyboards, bed rails and privacy curtains. To get rid of these germs, hospitals must rely on the staff members who know every nook and cranny in each room, as well as which cleaning products contain which chemical compounds.”
Having been a leader in several different hospital EVS departments over a period of 33 years, I interviewed candidates for front-line positions. When I asked, “Why do you want to work here?” the common reply was, “Because, you pay more than I make now.” The EVS tech job would pay her 25 cents more an hour than she made stuffing hamburgers in bags at Burger King.
This young lady went from working the window at the corner fast food restaurant to cleaning the operating room in two weeks for a quarter more an hour. The comparison of job roles and responsibilities is obviously not close to being similar. It’s time to educate and certify environmental services workers so, in this case, the young lady understands that better, more thorough cleaning and disinfection, saves lives. It’s time to turn that young lady into a Certified Environmental Services Technician (CEST).
Why don’t hospitals value the EVS technician? Too often, housekeepers or environmental service workers are thought to be expendable (anyone knows how to clean a toilet and mop a floor, right?) and difficult to educate because English may not be their first language. The thought is, “What if I educate and certify them and they leave?” But, worse than that, what if you don’t educate and certify them and they stay?
The Learning Objectives for the CEST
• Define Environmental Services #1 job as Infection Prevention
• Equip the frontline cleaning professional with knowledge of infection prevention as it relates to their daily tasks
• Analyze the cleaning professional’s role in patient satisfaction
• Support the cleaning professional with practical “how to” tips for cleaning and disinfection
• Introduce cleaning and disinfection strategies that effectively break the chain of infection (i.e., 7 Steps of Cleaning, daily duty lists, daily checklists, florescent marking of high touch surfaces, employee engagement, etc.)
• Convert the cleaning professional into a Certified Environmental Services Technician
The stakes are too high to allow the rooms of residents or patients to be cleaned by a person who is not a CEST. The CEST must be properly compensated, regarded as a part of the facility’s multi-modal infection prevention program, be well trained in the nuances of cleaning and disinfection, allotted the time to do the necessary tasks, equipped with the “Best in Class” tools to clean and disinfect surfaces and educated about the prevention and transmission of disease.
In closing, an educated and Certified E.S. Tech will be viewed as a knowledgeable professional working amongst other healthcare professionals who are certified or registered in their field. Knowledge leads the environmental services worker to be proud of the profession they have chosen and respected by those they work alongside of.
A closing thought: One well-trained, well-equipped, conscientious Certified Environmental Services Technician, given the proper tools AND an adequate amount of time to clean and disinfect a room patient’s room can PREVENT more infections than a room full of doctors can CURE.
I encourage you to keep the recognition going and celebrate your EVS superstars 365 days a year, this special week is a great excuse to focus on your team and reward them for doing an excellent job!
I am a Certified Environmental Services Technician and I save lives… what’s your super-power?
 J. Darrel Hicks, BA, Master REH, CHESP, Certificate of Mastery in Infection Prevention, and a Certified Expert Trainer -- is the owner/principal of Darrel Hicks, LLC. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. Hicks authored Infection Prevention for Dummies, a 43-page, pocket-size book that deals with the role that proper cleaning and disinfection plays in saving lives.
J. Darrel Hicks, BA, Master REH, CHESP, Certificate of Mastery in Infection Prevention, and a Certified Expert Trainer -- is the owner/principal of Darrel Hicks, LLC. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. Hicks authored Infection Prevention for Dummies, a 43-page, pocket-size book that deals with the role that proper cleaning and disinfection plays in saving lives.
Environmental Services Staff: The First Line of Defense in the War Against Preventable HAIs

By George Clarke
A fundamental problem in the healthcare industry is the opinion that environmental services (ES) staff serves as “just the cleaner, the janitor or the housekeeper.” This couldn’t be further from the truth. In fact, the healthcare ES staff – we prefer the designation Environmental Hygiene Specialist – are a crucial, yet all too often unheralded, factor in preventing drug-resistant infections.
According to the Centers for Disease Control (CDC), on any given day, one in 31 hospital patients has at least one healthcare associated infection (HAI). A recent study in the American Journal of Infection Control shows that Clostridium difficile infection (CDI), just one of many types of superbug infections, can result from the bacteria found on hospital environmental surfaces. Without proper cleaning of such surfaces, cross-contamination can occur, resulting in a preventable HAI (pHAI). The study showed that, with the proper ES protocols in place, CDI rates fell to zero over the course of 1,000 patient days. This is just the latest in a growing body of research highlighting the role played by ES staff in reducing HAIs.
Moreover, new standards and regulations from the Center for Disease Control and Prevention (CDC) and Association for the Healthcare Environment encourage hospitals to agree to and implement ES cleaning programs and total facility cleaning standards to clean and disinfect all high-touch surfaces.
In response to such research and recommendations, leading healthcare organizations are starting to recognize the importance of ES staff as part of an enterprise-wide multimodal intervention plan to combat such infections. As a result, all types of healthcare facilities – from acute-care hospitals to assisted living facilities – are elevating the role of cleaning and disinfecting processes to ensure the health and safety of patients, caregivers and their staff.
Below are the crucial factors in any ES program.
ES Staff Training and Recognition
Texas State University clinical microbiologist Rodney E. Rohde, PhD, says that distinguished ES Hygiene Specialists as among one of the most important “behind-the-scenes” professions in combatting HAIs and superbugs in healthcare systems and the community at large. In A Secret Weapon for Preventing HAIs, Rohde wrote that ES comprises the “first-line-of-defense specialists whose training has included learning best practices for effective infection prevention.”
Training programs recognize the science of cleaning and disinfecting that ES performs – both the clinical function of removing and inactivating/killing HAI-producing microbes, and the practical function of cleaning. ES staff training should include:
• Proper use of high-performance, reusable textile products and ergonomic tools
• Color-coded, one-per-room methodologies that simplify training, help reduce chemical usage, and – most important – offer a straightforward and elegant way to eliminate the risk of cross-contamination
• Improved cleaning thoroughness and enhanced cleaning methods of high-touch surfaces
More and more, healthcare management is acknowledging and rewarding ES staff that have undergone extensive in-service training in which participants learn best practices for infection prevention and hygiene management in the patient room, OR and throughout the healthcare facility. Such recognition serves as a significant employee morale boost. Once ES staff complete training, senior management supported and attended events offer an opportunity to present a certificate, pin or other designation, recognizing the ES staff members efforts and commitment to providing safe patient environments.
High-Performance, Reusable Products
High-performance, reusable textiles benefit from ongoing research and development of innovative fibers and materials. They deliver unrivaled performance, including absorbency, extremely high wet strength and far more versatility. The uncontested benefit of high-performance, reusable micro-denier fiber products is their ability to remove everything that can be physically removed from an environmental surface – some have the proven ability to remove the endotoxins released by bacteria when killed with disinfectant.
Such reusable micro-denier textiles usually are processed by experienced hospital linen processors, either on-premises or outsourced – following ARTA, CDC, OSHA, Healthcare Laundry Accreditation Council (HLAC) or TRSA recommended laundry processes. To counter a fictitious claim frequently made by disposable manufacturers, if recontamination were an issue with reusables, then hospitals would be overwhelmed with contaminated sheets, scrubs, incontinence pads, sheets, etc., that often are grossly contaminated with human excrement, vomit and BBP’s (blood borne pathogens). The fact is, according to the CDC, contamination of the patient environment from laundered textiles rarely, if ever, happens.
Disposable mops and wipers, on the other hand, provide limited performance in removing pathogens from an environmental surface. The majority are made from 100 percent polyester fiber imported from China and are primarily used as a vehicle to get the disinfectant/chemical onto a surface.
Moreover, depending on the disposable product selected, the increase in cost ranges from three to more than twelve times that of using a reusable wiper.
Disinfectants to Support the Healthcare Wiper Cycle
An oft-overlooked topic is the disinfectants being used and how they are incorporated throughout the healthcare cleaning cycle. The mop or wiper cycle is repeated every day in every healthcare facility. This is the typical scenario:
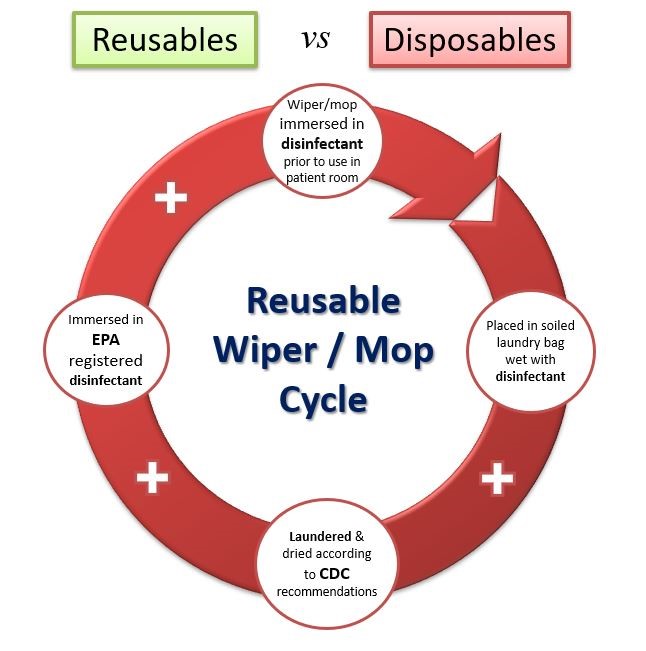
• The standard practice for a reusable mop or wiper is the “dip and wring” method. Clean products are folded and stacked in a pail and immersed in an EPA registered disinfectant. The wiper is then used in the patient room – ideally, following a color-coded methodology.
• Products are put damp (or still wet) in a closed soiled laundry bag with other damp wipers and transported to the laundry. Often, they wait many hours, if not days, to be laundered — thus far exceeding any recommended dwell time for any disinfectant.
• Then, the reusables are laundered by an experienced healthcare laundry, typically processing to CDC and/or OSHA recommendations for blood borne pathogens, then dried at recommended temperatures.
• Before going back into any patient room, the flat mops and wipers are again immersed in an EPA-registered disinfectant.
Given this process, how is it possible that any viable organism survived this entire cycle and re-contaminated a patient room? The only conclusions possible are, either the disinfectant is not living up to its efficacy claims or, most likely, the disposable manufacturers have intentionally neglected to take the disinfectant into consideration.
Currently, bleach-free, EPA-registered sporicidal disinfectants are available that achieve CDI sporicidal disinfection in four minutes or less. As they are not bleach products, they do not corrode hard surfaces and are safer for workers due to their low Hazardous Materials Identification System (HMIS) health rating of one. Such solutions — effective against a broad range of microorganisms including CDI spores, hepatitis B, TB and norovirus — are easier for ES staff to use, more sustainable with packaging, a longer shelf life, and very economical.
A Final Thought: Key Considerations to Support ES Staff
In the best healthcare settings, C-suites are beginning to grasp the difference a highly trained ES staff member can make not only in the lives of patients, but also in the facility’s reputation, goodwill and financial health.
ES staff serves as the first line of defense in ensuring safe environments in hospitals and long-term care facilities, thereby helping protect the broader community. Those who recognize this by investing in these unsung heroes will improve patient outcomes, boost financial health, increase satisfaction rankings and support the community at large. Some key points to keep in mind:
• Adopt an enterprise wide multi-modal approach to reducing pHAIs
• Invest in proper training of ES staff
• Engage with and recognize ES staff for their critical role in infection prevention
• Leverage high-performance, proven textiles and disinfectants for cleaning and infection prevention
Overcoming the lack of knowledge of the unheralded ES professional is critical in the battle against antibiotic resistant superbugs. The next time you’re in a healthcare facility, take a moment to recognize those who are keeping the environment safe via proper cleaning and disinfection protocols. They are as important as doctors and nurses in maintaining your public health and safety.
 George Clarke is CEO of UMF Corporation.
George Clarke is CEO of UMF Corporation.
