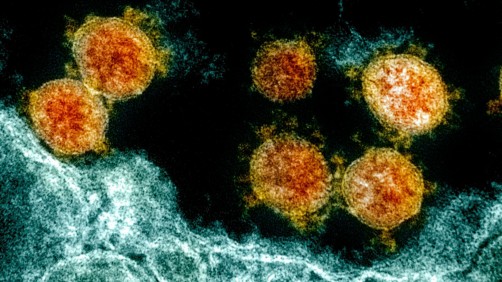
If you’re wondering why after two vaccination doses and a booster shot, you still got sick from the omicron strain of the virus that causes COVID-19, one possible answer may have been found in a recent study by researchers at Johns Hopkins Medicine and the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health (NIH).
The research findings, first posted online April 7 in the Journal of Clinical Investigation Insights, suggest that while fully vaccinated and boosted people produce a high level of antibodies that work against the original strain of SARS-CoV-2, the same tiny defenders don’t do as well in preventing the omicron strain from attacking healthy cells.
“Previous research has shown vaccine-induced antibodies respond to the original strain of SARS-CoV-2 by inhibiting the virus’s ability to bind to angiotensin-converting enzyme 2 [commonly known as ACE2], the receptor on a cell’s surface through which SARS-CoV-2 gains entry,” says study senior author Joel Blankson, MD, PhD, professor of medicine at the Johns Hopkins University School of Medicine. “Our study suggests those same antibodies yield less ACE2 inhibition with the omicron strain, opening the door to a breakthrough COVID-19 infection.”
To conduct their study, Blankson and his colleagues analyzed both the humoral (SARS-CoV-2 specific antibodies circulating in the bloodstream and produced by B lymphocytes, or B cells) and cellular (direct attack on the virus by T lymphocytes, or T cells) immune responses in 18 healthy and fully vaccinated people, ages 23 to 62 (mean age of 30), who experienced breakthrough infections within 14 to 92 days (median of 50 days) after receiving a booster COVID-19 vaccine. Fourteen participants received a booster of the Pfizer-BioNTech messenger RNA (mRNA) vaccine, one was boosted with the Moderna mRNA vaccine and the remaining three had an mRNA booster following their initial dose of the Johnson & Johnson viral vector vaccine.
The humoral and cellular immune responses of those participants with breakthrough infections were compared with those from a control group of 31 participants, ages 21 to 60, who received similar COVID-19 vaccinations and boosters, and had no prior infection with SARS-CoV-2.
Although the researchers were not able to document that the breakthrough infections were from the omicron strain, they say it’s a strong probability because the omicron variant accounted for more than 90% of the COVID-19 cases treated at The Johns Hopkins Hospital (where the study was conducted) during the time when the study participants became symptomatic.
“When we tested antibody-mediated inhibition of SARS-CoV-2 spike protein binding to ACE2, we found that serum from study participants with breakthrough COVID-19 — most likely the result of omicron infection — had antibodies that strongly stopped binding by the original strain virus as expected but didn’t carry out that function as well when responding to the omicron strain,” says Blankson.
The levels of antibodies that inhibited spike protein binding to ACE2 — high for original strain virus but reduced for omicron — were similar for both the participants with breakthrough infections and those in the control group.
The specific reduction in ACE2-inhibiting antibodies responding to omicron, Blankson says, differs from what was seen in previously studied breakthrough infections with the alpha variant. In those cases, infected individuals were found to have lower overall antibody levels to the original virus strain.
However, the level of cellular immunity — as measured by the amount of responding T cells documented — remained strong in the breakthrough and control groups for both the original and omicron strains. This was shown in a second recent study, also co-authored by Blankson, looking at the blood plasma of 15 mRNA vaccine recipients.
“The comparable strong T cell responses for the original and omicron strains in both studies could explain why people, like our study participants, who have breakthrough COVID-19 cases typically experience only mild symptoms during the course of their illness,” he explains.
The study was supported by the Johns Hopkins COVID-19 Vaccine-related Research Fund, by funds from the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health (NIH), and three NIH awards: National Cancer Institute grant U54CA260491 and NIAID grants K08AI156021 and U01AI138897.
Along with Blankson, the members of the study team from Johns Hopkins Medicine are lead author Bezawit Woldemeskel and co-authors Tihitina Aytenfisu, Andrea Cox, Alexander Damanakis, Arbor Dykema, Nicole Frumento, Caroline Garliss, Trevor Johnston, Andrew Karaba, Heba Mostafa, Desiree Wright and Andrew Yang. Team members from NIAID are Evan Beck and Oliver Laeyendecker.
Source: Johns Hopkins Medicine