Researchers at Washington University School of Medicine in St. Louis have identified central routes that two deadly viruses take to invade human cells and have designed decoy molecules that block the infections.
The discoveries — published this week in two separate studies — set the stage for developing new prevention and treatment strategies for yellow fever virus and tick-borne encephalitis viruses, members of a group of viruses that includes Zika, dengue, West Nile and Japanese encephalitis viruses. With shifting climate conditions, such viruses are expanding their ranges, increasing the threats they pose to public health.
The study on yellow fever virus appears in Nature, and the study focused on tick-borne encephalitis viruses is published in PNAS.
“There are no treatments for these viral infections, so there is an urgent need for new strategies to prevent and treat these infections, which continue to cause severe disease and death in far too many cases,” said Michael S. Diamond, MD, PhD, senior author of both studies and the WashU Medicine Herbert S. Gasser Professor of Medicine. “Our studies showing how these viruses get into cells creates opportunities to disrupt those routes, stopping viral infections from jumping animal species — both wild and domesticated — and spreading through populations of people.”
Yellow fever virus is spread by mosquitoes and is common in parts of Africa and South America. Many people infected experience flu-like symptoms and recover. According to the World Health Organization, about 15% of infections are severe, causing high fever, liver failure, internal bleeding and toxic shock. About half of cases that come to clinical attention — which number in the tens of thousands each year — end in multi-organ failure and death. Vaccination can protect against yellow fever, but the sole vaccine available uses a live virus, so people with weakened immune systems, including infants and older adults, cannot take it.
Tick-borne encephalitis virus is spread by several tick species, and different versions of the disease occur across parts of Europe, Russia and Northern and Eastern Asia. Severe forms of the infection cause inflammation of the brain and spinal cord, leading to neurological disease and death. An inactivated vaccine exists for only one subtype of this virus and is most often recommended for travelers at high risk of exposure to ticks in endemic areas.
Over a century of studying these viruses, scientists had not understood how they infect cells. Knowing the infection route is a crucial step to impeding viral entry.
“Vaccine development for both of these viruses first started in the 1930s; in the case of yellow fever, we are still using the same live-attenuated vaccine developed in 1937 by Max Theiler, who later won a Nobel Prize for the discovery,” said co-author Daved Fremont, PhD, a professor of pathology and immunology, of biochemistry and molecular biophysics, and of molecular microbiology at WashU Medicine. “Our new studies are a step toward the development of a new generation of vaccines and antiviral strategies for active infections. This work exemplifies the remarkable expertise that the WashU Medicine community can bring to bear on a significant biomedical issue.”
The researchers used genetic techniques, including CRISPR gene editing technology, to identify a family of cell-surface proteins called low-density lipoprotein receptors (LDLR) as the main route these viruses use to enter cells. The researchers focused on these particular receptors because of their own and others’ past work identifying them as important entry receptors for other types of viruses, including alphaviruses such as Venezuelan equine encephalitis virus.
In Nature, the researchers are the first to report that yellow fever virus latches onto LDLR receptors LRP1, LRP4 and VLDLR.
In PNAS, they showed that tick-borne encephalitis viruses enter cells via a different family member, LRP8 — a finding similar to that from a recent study by another group that implicates the same receptor.
The researchers found that genetically eliminating these receptor proteins from the surfaces of cells blocked the viruses from infecting those cells. They also found that adding abnormally high numbers of these receptors to cells allowed more virus to enter.
The specific receptors they identified may explain why the viruses have different impacts on different organs in the body. For example, high amounts of LRP1 are found on the surface of liver cells, and yellow fever virus infection can cause severe liver disease. Likewise, LRP8 is found primarily on the surface of cells in the nervous system, helping explain the severe neurological symptoms characteristic of tick-borne encephalitis virus.
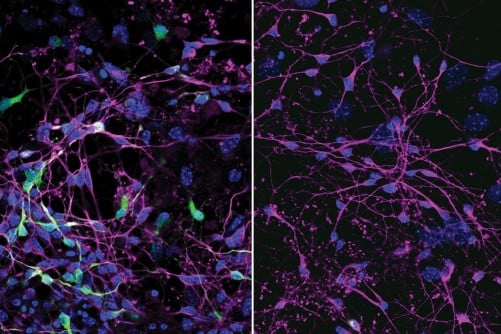
In both studies, the team designed “decoy” molecules that include a piece of an antibody attached to the entry receptors, which are not embedded in cells — a strategy that tricks the viruses into latching on to the decoys rather than the cells, thereby protecting cells from infection. The decoy molecules prevented infection in human and mouse cells in the lab. They also protected immunodeficient mice from what is typically a lethal dose of yellow fever virus, compared with mice receiving a placebo decoy. The receptor decoys also prevented liver cell damage in mice engrafted with human liver cells.
According to the researchers, this antiviral strategy is appealing because the decoy is based on a human protein that won’t evolve, rather than a viral protein that will always be a moving target, adapting to evade therapies targeted against it. In theory, if the virus mutates to evade the decoy, it is also adapting away from its ability to bind the human protein, making it less infectious, according to Diamond, also a professor of molecular microbiology and of pathology and immunology.
Reference: Chong Z, Hui S, Qiu X, Palakurty S, Sariol A, Kaszuba T, Nguyen MN, Li P, Raju S, Hall PD, Nelson CA, Baltazar-Perez I, Price DA, Rothlauf PW, Crowe JE, Whelan SPJ, Leung DW, Amarasinghe GK, Bailey AL, Fremont DH, Diamond MS. Multiple LDLR family members act as entry receptors for Yellow Fever virus. Nature. Oct. 29, 2025. DOI: 10.1038/s41586-025-09689-2.
Source: Washington University in St. Louis