Touting advancements in prevention and management of SARS-CoV-2 since the pathogen was initially identified in 2019, healthcare epidemiologists and infectious disease experts from eight institutions say now is the time to end policies mandating universal masking in the healthcare settings -- at least for now. The commentary is published in Annals of Internal Medicine.
“While critically important in the earlier phases of the pandemic, we’ve entered a more stable phase, with substantial population-level immunity, durable protection against severe disease, a series of less virulent variants, and other important and favorable changes,” said corresponding author Erica S. Shenoy, MD, PhD, medical director of Infection Control for Mass General Brigham and an infectious diseases physician at Massachusetts General Hospital (MGH). “As conditions change, we need to re-evaluate our infection prevention policies, including masking requirements in healthcare settings, and adapt.”
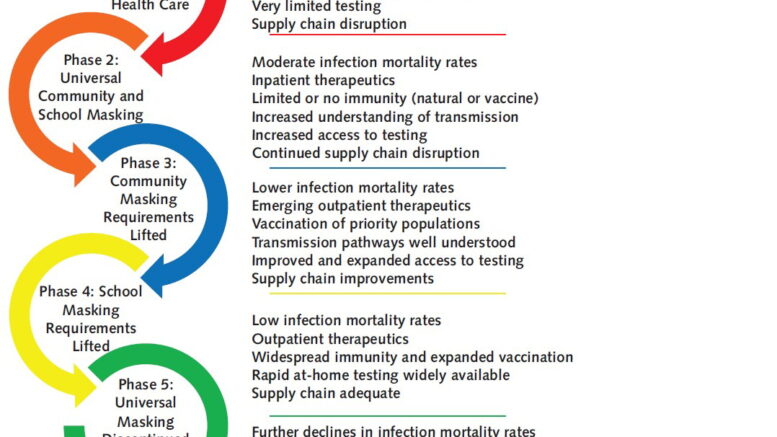
In the commentary, the authors emphasize different phases of the pandemic and describe that while universal masking was justifiable before medical countermeasures were available, advancements and population immunity have changed the appropriateness of the policy. Highlighting a theme of constant and ongoing change, they review the rationale for initially expanding mask use in healthcare settings, the reasons why de-escalation is needed, and conditions that could prompt reconsideration of use of masks more widely again.
“After three years of universal masking in healthcare, the risk-benefit calculation has shifted,” said Shira Doron, MD, chief infection control officer for Tufts Medicine health system and hospital epidemiologist at Tufts Medical Center. “Masks do have downsides, such as impaired communication and disrupted human connection. We are at a stage of the pandemic where it now makes sense to end mandatory masking.”
Given advancements, the authors advocate for managing SARS-CoV-2 in a similar way to how other respiratory viruses are managed in healthcare settings. This includes ensuring healthcare personnel use masks (and eye protection) when engaging in activities that could generate splashes or sprays and having patients mask if they have respiratory symptoms.
“As the pandemic moves into an endemic phase, we need to transition prevention efforts to incorporate all respiratory viruses. Performing risk assessments and applying lessons learned from COVID-19, including about how to apply masking, will permit a more flexible, durable response now and in future seasons,” said co-author Sharon Wright, MD, MPH, chief infection prevention officer at Beth Israel Lahey Health in Cambridge.
“The best evidence-based policy making is dynamic, and adapts to changing conditions, evidence, and contexts. As all these factors change, even policy goals may need to be updated,” said senior author Westyn Branch-Elliman, MD, MMSc, an infectious diseases specialist and clinical investigator at VA Boston Healthcare System. Since 2020, she explained, society has been living in a constant state of change during which we have achieved major preventative and therapeutic advancements and the infection fatality rate has fallen dramatically. She continued: “At the same time, we know universal masking is not without costs, even in healthcare. Given these realities, it is time to update policies once again, recognizing this is unlikely to be the last update. Change and adaptation are expected. That does not mean ‘the science has changed’, but almost everything around it has.”
The authors say that throughout the pandemic, widespread use of universal masking in healthcare settings was justifiable for reducing the risk of transmission between health care personnel, patients, and visitors, and preserving the healthcare workforce to maintain operations during surges. Universal masking was one element of a larger bundle of strategies implemented to limit transmission during a time when little was known about the pathogen and effective interventions had not yet been identified. Since then, the burden of SARS-CoV-2 has been mitigated through access to testing, substantial population-level immunity acquired over time, emergence of less virulent variants, and widespread availability and use of vaccines and treatments.
This means the time has come to manage SARS-CoV-2 as other endemic respiratory viruses using correct and consistent application of Standard and Transmission-based Precautions. These include healthcare personnel use of masks and eye protection when engaging in activities that generate splashes or sprays to the face, regardless of patient symptoms, and masking of patients when symptoms are present, among other precautions.
In addition to ending universal masking, the experts suggest that other pandemic-era strategies, such as asymptomatic testing and contact tracing, should be reconsidered in the endemic era.