Nearly 39 million people worldwide are carriers of human immunodeficiency virus (HIV), and 1.3 million people contracted HIV in 2022[1]. Forty years after the virus was discovered at the Institut Pasteur, HIV research is still active – the aim is to elucidate the mechanisms of infection so that the virus can be eradicated. A concerted global effort has led to considerable progress in knowledge. The conference "40 years of HIV science," held November 29 to December 1 at the Institut Pasteur in collaboration with ANRS | Emerging Infectious Diseases, was an opportunity to look back at the major advances that are now raising hopes of remission and a cure for HIV.
For the past 40 years, since HIV was identified at the Institut Pasteur, scientists have been working to describe the virus and to understand the different stages from initial infection to integration in the host cell genome. This knowledge has led to considerable scientific and medical progress to slow infection, and has also improved the life expectancy and quality of life of people living with HIV. The participants in the opening session of the conference "40 years of HIV science" share the observation that although there have been major breakthroughs, the battle against HIV is not over, even if they have high hopes of finding avenues for remission and a cure.
"I salute all these years of research, medical progress and activism, but there are still many challenges to overcome. Despite all the progress made, 630,000 people died from AIDS in 20221 and new infections continue to occur. The fight against HIV is not over. This international battle continues, and no one will be left behind," said Stewart Cole, president of the Institut Pasteur.
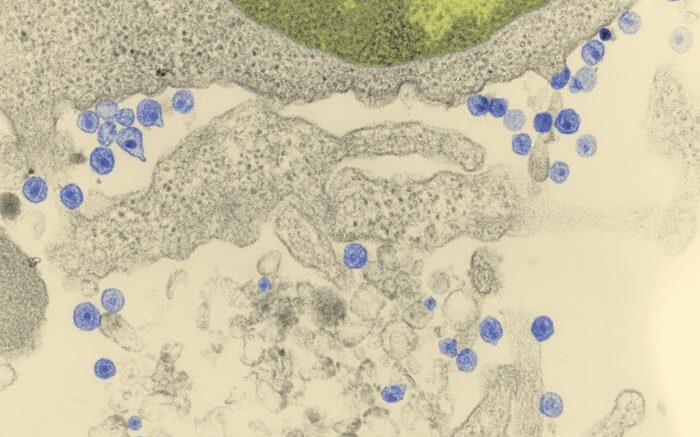
In response to these challenges, several different fields of investigation are being actively explored, especially to elucidate the molecular mechanisms that underpin HIV replication and viral integration into the host cell genome. State-of-the-art techniques have led to the surprising discovery that the virus targets the cell nucleus. It exploits host cell mechanisms to multiply its genome and produce viral particles that infect other cells. This discovery that HIV targets the cell nucleus opens new avenues for tackling viral replication and persistence. Another approach under exploration is innate immunity, in other words the body's defenses, which can be harnessed to block the virus as soon as it enters the cell. It may be possible to stimulate this natural response by developing immunotherapy treatments.
Removing the virus from all the cells in the body where it is present is crucial to avoid viral persistence. Scientists are using new technologies to understand how the virus evades the immune system and antiretroviral treatments to remain in reservoirs, and to determine the location of these viral reservoirs. Lymph nodes and intestines are among the reservoirs that scientists are investigating closely.
How is it that some people are able to suppress HIV without antiretroviral treatment, by slowing its progression or preventing the reactivation of viral reservoirs? These people are able to control HIV infection because of an optimal immune response that neutralizes the virus. One strategy that is being explored as a novel therapeutic solution to overcome HIV infection is to attempt to reproduce the particularities of the immune cells responsible for this optimal response.
"The identification of HIV control in some individuals has significantly boosted hopes of remission and cure and has given us a unique opportunity to study the underlying mechanisms," explains Asier Sáez-Cirión, Head of the Institut Pasteur's Viral Reservoirs and Immune Control Unit.
Scientists are also interested in people who, despite repeated exposure to HIV, have never been infected because they have a genetic mutation that stops the virus from entering their cells. This mutation could be induced by gene therapy. Developing molecular scissors to make the body resistant or targeting the virus to eliminate it after its integration in the cell are fields of study that might pave the way to a long-term cure.
As well as the challenges in medical research to improve our understanding of the mechanism of action of HIV infection, there are also societal challenges. Patient organizations, scientists and researchers in social sciences have been working together for the past 40 years to change attitudes to HIV and AIDS by tackling discrimination and the stigma attached to people living with HIV and by calling on authorities to help improve prevention and early diagnosis. The availability of rapid diagnostic tests is one of the tangible results of this collective effort. Therapeutic innovation alone is not enough – it needs to go hand in hand with targeted, relevant programs that will reach people at risk of HIV infection. The aim of the community-based research that has developed as part of the fight against HIV is to complement existing knowledge to reduce inequalities in access and to tailor strategies to patients' real-life circumstances. 9.2 million people living with HIV still did not have access to antiretroviral treatment in 2022. Access to antiretroviral treatment and infection prevention methods like PrEP (pre-exposure prophylaxis) is also a social battle that is being fought by stakeholders in the war against HIV.
To achieve the goal of eradicating HIV, the members of the international community that attended the conference confirmed that we need to double down on our efforts to explore all the scientific avenues that are opened with each new discovery related to the virus, and to step up work on prevention and access to therapies.
Source: Institut Pasteur