That penicillin allergy label you’ve had since you were 5 years old? You may not need it anymore.
“Back then, we didn’t know that these allergy labels go away. Now, we do. For example, we know that in just ten years, most people lose their penicillin allergy label,” said Rajan Ravikumar, MD, assistant professor of internal medicine and assistant medical director of the University of Michigan Medical Group at the Medical School.
Evaluating allergy labels to ensure patients receive the best care possible is the goal of Michigan Medicine’s Beta-Lactam Allergy Evaluation Service, initiated in July 2021.
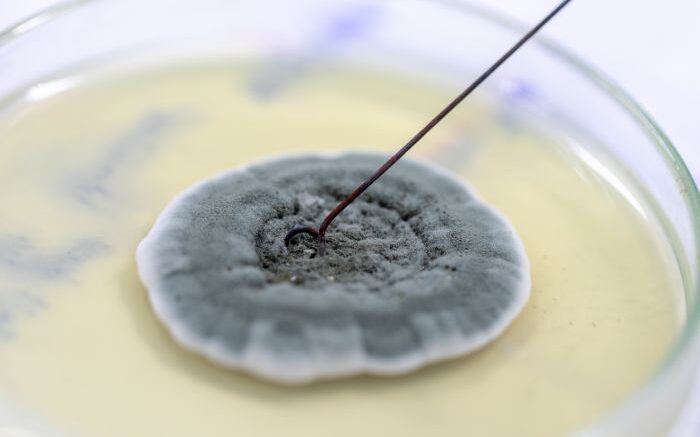
The service uses various methods to test patients labeled as allergic to drugs in the Beta-Lactam family, including penicillin. This family of drugs is the first line of treatment for many common ailments, including ear infections in children and sinus infections in adults. Many patients who are “allergic” were labeled as such due to reactions they had as children, or because of other reactions in their family history. However, patients who don’t have these allergy labels addressed can be at higher risk of complications in the hospital if an alternative medication is needed during their care – for instance, patients who get alternatives rather than beta-lactam antibiotics are more likely to get surgical site infections and are in the hospital longer because of more treatment failures.
This, Ravikumar says, is why it’s so important to have these labels evaluated.
If you’re determined a good candidate for the Beta-Lactam Allergy Evaluation Service, nurse practitioners Becka Hanson, FNP, and Lauren Barhitte, FNP, will help inpatient teams address a beta-lactam allergy label on your chart, determine if the allergy is still real, and then remove the label when necessary.
You’ll be asked various questions about the label including how long ago it was given to you and your allergy history. You can receive a test dose of a medication or, depending on the severity of the allergy history, a skin test first before getting the test dose. You’re then monitored every 15 minutes for an hour, and the label can be removed if you experience no symptoms during that time. Results are quickly shared with your primary care team, and you receive testing cards with information about your evaluation. If you remain allergic to the drug, it’s recommended that you continue avoiding it, but have your label evaluated again in a few years.
The service has seen great success: in its first year alone, over 700 patients were evaluated, and about 99% passed their test dose and had the allergy label removed.
The relabeling rate is low – only about 5% of people have their label put back. Michigan Medicine teams are in contact with these patients when it happens – a patient is often relabeled simply because they forgot they’d been evaluated for the allergy.
Ravikumar says the existence of this program not only teaches people that some allergies can go away with time, but also serves as a reminder for patients to have their allergy labels evaluated – especially if it’s an allergy they aren’t very familiar with or a label they were given as a child – to avoid impacting their future care.
“The goal really is to get people off agents we know don’t work as well, or that lead to more infections and have more side effects,” Ravikumar said. “We’re trying to remove those barriers to get people on first line treatment, get them better and out of the hospital faster, and make sure that when they are in outpatient, they can receive these antibiotics without any concern.”
Source: Michigan Medicine - University of Michigan