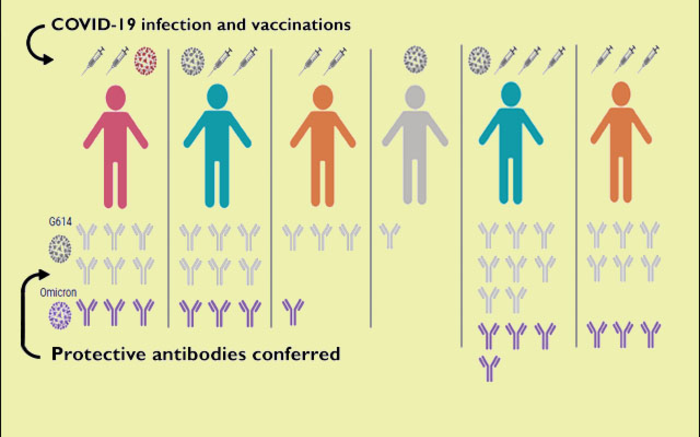
The number of exposures to the coronavirus spike protein, through infection or vaccination, influences the degree of antibody response. Courtesy of Veesler Lab
A recent study looked at the strength, durability and breadth of neutralizing antibody responses generated by breakthrough infections in individuals vaccinated against SARS-CoV2.
The findings are published this week in Cell. Alexandra Walls and David Veesler in the Department of Biochemistry at the University of Washington in Seattle led the project.
Characteristics of the Delta and Omicron coronavirus variants of concern include enhanced transmissibility and immune evasion even in non-immunologically naïve individuals, compared to the ancestral pandemic coronavirus.
These characteristics, and the waning of immunity from vaccines, have led to breakthrough infections in vaccinated individuals. For the most part, otherwise healthy people who are vaccinated against the SARS-CoV-2 usually do not have severe symptoms if they do end up contracting the virus.
The researchers wanted to understand what effect catching the virus after being vaccinated has on neutralizing antibodies, and to see how durable and broad these responses are. Their hope is that advancing such knowledge will help guide vaccination policies and pandemic mitigation strategies.
Through their project the researchers learned that the degree of antibody response depended on whether a person has had one, two, three, or four exposures to the spike protein through infection, vaccination, or a mixture of the two. The scientists also checked antibody responses in groups of individuals who had been vaccinated after having COVID-19, those who were previously vaccinated and experienced a breakthrough infection, those who were vaccinated only, and those who were boosted and therefore vaccinated three times.
Among their study subjects, those who had completed a three-vaccination protocol, and those who had been vaccinated after recovering from COVID-19, and those with a breakthrough infection after vaccination launched almost comparable neutralizing antibody responses, in terms of magnitude and breadth. Their serum binding and antibody neutralizing responses to the spike protein in the current pandemic coronavirus variants were much more potent and lasting than those generated by people who had received only two doses of COVID-19 vaccine or who had a previous infection not followed by vaccination.
This observation suggested that the increased number of exposures to SARS-CoV-2 antigens, either through infection and vaccination or triple vaccination, enhanced the quality of antibody responses.
The researchers also looked at how broad the elicited antibodies could be. They investigated neutralization of the divergent Omicron SARS-CoV-2 variant of concern, currently responsible for the majority of cases in the United States. Their findings showed that boosted individuals (or those that have a mixture of infection and double vaccination) have neutralizing antibodies at similar levels to subjects vaccinated twice against the original ancestral strain. This suggests a large amount of immune evasion, but that vaccine boosters can help close the neutralizing antibody gap caused by Omicron.
Looking outside of the SARS-CoV-2 family shows a similar pattern, where repeated and multiple exposures improves the otherwise weak neutralizing antibody response to SARS-CoV. Finally, the authors did not identify improvements in antibody binding to common cold causing coronavirus spike proteins like OC43 or HKU1. This suggests that repeated SARS-CoV-2 exposure does not improve spike reactivity to more divergent coronaviruses. These findings support the development of broader sarbecovirus or coronavirus vaccines to be prepared in the event of a future spillover event.
The study groups consisted of about 15 people, from the Hospitalized or Ambulatory Adults with Respiratory Viral Infections, or HAARVI, project at the UW in Seattle. HAARVI, led by UW Medicine infectious disease physician Helen Chu, looks at recovered COVID-19 patients to study immune responses over time, to understand the long-term consequences of the infection, and to compare immune responses from vaccines and natural infections.
Researchers from the Department of Medicine and the Department of Laboratory Medicine and Pathology at the UW School of Medicine, and from Humabs Biomed SA, a subsidiary of Vir Biotechnology, also helped conduct the study.