The Centers for Disease Control and Prevention (CDC) has issued a Health Alert Network (HAN) health advisory to notify clinicians and public health authorities of a recent increase in pediatric invasive group A streptococcal (iGAS) infections.
In November 2022, CDC was notified of a possible increase in iGAS infections among children at a hospital in Colorado. Potential increases in pediatric iGAS cases in other states were subsequently noted by contributors to the Infectious Diseases Society of America’s provider-based Emerging Infections Network and by certain jurisdictions participating in CDC’s Active Bacterial Core Surveillance System (ABCs). This increased number of pediatric iGAS cases in some jurisdictions has occurred in the setting of increased circulation of respiratory syncytial virus (RSV), influenza viruses, SARS-CoV-2, and other respiratory viruses. While the overall number of cases has remained relatively low and iGAS infections remain rare in children, CDC is investigating these reports.
This Health Advisory highlights the recent rise in iGAS infections in children, the increased seasonal risk of iGAS disease for all age groups, and the importance of early recognition, diagnosis, and appropriate treatment of these diseases in children and adults.
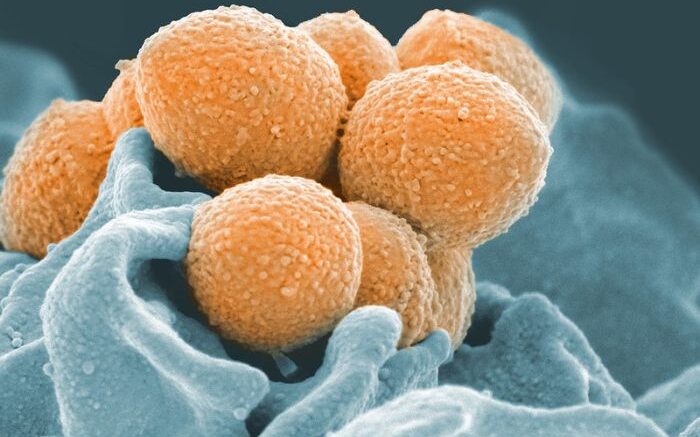
Group A Streptococcus (GAS) bacteria can cause a range of illnesses, from pharyngitis (i.e., strep throat) and skin and soft tissue infections to uncommon but severe diseases such as sepsis, streptococcal toxic shock syndrome, and necrotizing fasciitis. These severe and invasive diseases are associated with high mortality rates and require immediate treatment, including appropriate antibiotic therapy.
Similar to other agents spread primarily by the respiratory route, cases of GAS, including both iGAS and streptococcal pharyngitis (“strep throat”), tend to have a pronounced seasonal pattern with a peak in December through April in the United States. Strep throat is most common among school-aged children (i.e., 5–15 years of age), and exposure to someone with strep throat is a risk factor for iGAS infection. In addition, increased rates of iGAS infection have been noted during times of increased influenza activity. Seasonal influenza activity is currently high in the US and above the levels seen in recent years.
People with concurrent or preceding viral infections, such as influenza and varicella (chickenpox), are at increased risk for iGAS infection. Other groups at higher risk for iGAS include:
- People aged 65 years or older
- American Indian and Alaska Native populations
- Residents of long-term care facilities
- People with medical conditions such as diabetes, malignancy, immunosuppression, chronic kidney, cardiac, or respiratory disease
- People with wounds or skin disease
- People who inject drugs or who are experiencing homelessness
iGAS cases reported to ABCs, CDC’s active laboratory-and population-based surveillance system for invasive bacterial pathogens, were lower than usual among all age groups during the COVID-19 pandemic. This decrease started in April 2020 and was partly due to associated respiratory disease mitigation measures. A review of preliminary ABCs data from 2022 demonstrated a monthly increase in the number of confirmed iGAS cases in children between September to November, above what was seen in the same period in 2020 and 2021. However, it is too early to determine whether this rise is beyond what would be expected for pre-COVID-19 GAS seasonal patterns.
Recommendations for Healthcare Providers
- Offer prompt vaccination against influenza and varicella to all eligible persons who are not up to date.
- Consider iGAS as a possible cause of severe illness, including in children and adults with concomitant viral respiratory infections. Illness due to iGAS in persons with known viral infections may manifest as persistent or worsening symptoms following initial improvement.
- Educate patients, especially those at increased risk, on signs and symptoms of iGAS requiring urgent medical attention, especially necrotizing fasciitis, cellulitis and toxic shock syndrome.
- Obtain culture for suspected iGAS infections, including blood, wound, and pleural fluid cultures, as clinically indicated.
- Follow clinical practice guidelines for diagnosis and treatment of GAS pharyngitis.1
- Be mindful of potential alternative agents for treating confirmed GAS pharyngitis in children due to the shortage of amoxicillin suspension.
- Notify appropriate local or state public health departments as soon as possible about unusually aggressive or severe iGAS cases affecting children younger than 18 years of age or clusters of iGAS infections in persons of any age.
- Ask laboratories to hold iGAS isolates or send them to the state public health laboratory for temporary storage.
Source: CDC