Patients who are dependent on marijuana may face higher infection rates following knee and shoulder arthroscopy, according to a study presented at the Scientific Forum of the American College of Surgeons (ACS) Clinical Congress 2022.
Using PearlDiver, a national insurance claims database, researchers from the University of Chicago performed a retrospective study of patients with marijuana dependence who underwent knee or shoulder arthroscopy for the postoperative complications of deep vein thrombosis (DVT), pulmonary embolism (PE), and infection.
“Marijuana has been gaining so much popularity, but it’s a risk factor we aren’t really catching,” said lead study author Sarah Bhattacharjee, MD, who conducted the research while she was a medical student at the University of Chicago. Bhattacharjee is now a surgical resident in orthopaedic and sports medicine at the University of Washington. “The higher infection rate found by this new study should raise a ‘red flag’ for patients and providers and should be discussed along with other risk factors before an arthroscopic procedure.”
Although the effect of marijuana use has been studied in pain management and cardiovascular health, few studies have looked at the potential effects of marijuana use by patients who are undergoing surgery. More states are legalizing marijuana, and the size of the cannabis market is predicted to reach $91.5 billion by 2028.1 Given that trend, the team of researchers from the University of Chicago set out to determine if marijuana-dependent users face an increased risk of complications following knee or shoulder arthroscopy.
“There’s so much information out there on smoking, alcohol, and other substances, but not on marijuana use,” said study coauthor Jason Strelzow, MD, assistant professor of orthopaedic surgery, University of Chicago. “As providers and surgeons, we should be discussing marijuana use with our patients, something that we have traditionally shied away from.”
All patients undergoing knee or shoulder arthroscopy were identified retrospectively in PearlDiver. Next, patients who had a diagnostic code for marijuana dependence were also identified within each surgery category; this is a rigid definition requiring patients to three or more criteria, such as using marijuana longer than intended, difficulty in cutting down use, spending a lot of time in obtaining or recovering from marijuana, and high tolerance.
The rates of DVT, PE, and infection within 90 days were assessed for all patients. Univariate analyses of marijuana dependence on all outcomes were performed, followed by a multivariate logistic regression analysis controlling for known patient comorbidities (other medical conditions).
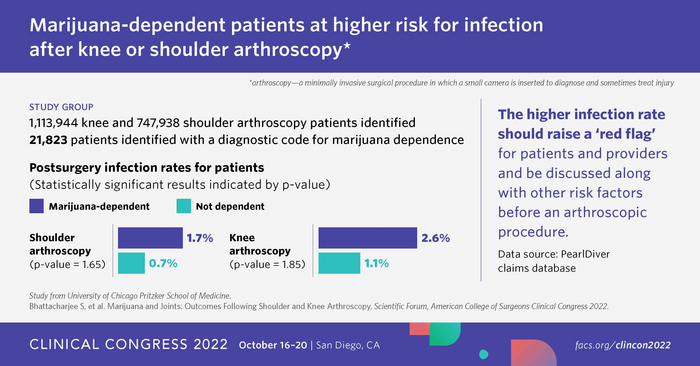
The researchers identified 1,113,944 knee and 747,938 shoulder arthroscopy patients. Out of those 1,861,892 patients, 21,823 patients had a diagnostic code for marijuana dependence.
Within both subgroups, the marijuana dependence cohort experienced increased rates of infection and DVT, while the PE rate stayed the same. For the shoulder arthroscopy group, the rates of infection increased from 0.7% to 1.7%, the DVT rate from 0.2% to 0.4%, while PE stayed at 0.2%. In the knee arthroscopy group, the rates of infection increased from 1.1% to 2.6%, the DVT rate rose from 0.2 to 0.3%, and PE stayed at 0.3%.
In the multivariate analyses controlling for a variety of patient risk factors, including tobacco use or a history of diabetes, marijuana dependence was identified as an independent risk factor for infection within both cohorts. In this study, a statistical measure called a p-value was used to determine if the detected relationship was due to chance (p-values of 0.001 or below) or did, in fact, exist (p-values above 0.001). For the knee group, the p-value was 1.85, and for the shoulder group it was 1.65.
(Note: The presenting author reported on updated data from the podium during the conference reflecting stable PE rates.)
Strelzow hopes surgeons will use the study results to help inform marijuana-dependent patients about risks, benefits, and available alternatives, such as reducing or eliminating marijuana use six months prior to an arthroscopic procedure.
Although the study focused on minimally invasive surgery, Strelzow said that “we would expect similar or larger effects with more open or invasive procedures.”
The study has identified the need for additional research to better understand the relationship between marijuana dependence and postoperative complications. In addition, given that the study used very rigid criteria for marijuana dependence, there are opportunities for future clinical studies to investigate how various levels of marijuana use impact postoperative complications. Strelzow said he plans to study the impact of marijuana dependence on fracture healing.
Reference: Bhattacharjee S, et al. Marijuana and Joints: Outcomes Following Shoulder and Knee Arthroscopy, Scientific Forum, American College of Surgeons Clinical Congress 2022.
Source: American College of Surgeons