A team at Sandia National Laboratories has developed a faster and more comprehensive way of testing personal protective equipment, or PPE. The basic principle: modeling a device to fit the human form and human behavior.
When COVID-19 hit, PPE testing became an urgent need. In March 2020, when the country went into lockdown, many people turned to Sandia for PPE testing support. They were trying to bring new masks to the market, provide quality assurance for imported masks and vet cleaning processes for reuse of single-use PPE.
“Whether using in-house or commercial filter test systems, we found the testing process was very time-consuming and not as efficient as it could be,” said Michael Omana, an aerosol scientist at Sandia.
The team, which includes engineers Todd Barrick and Brad Salzbrenner, was determined to find a better solution. They were trying to think of ways that respirators could be tested rapidly, not destructively, and have other testing capabilities introduced, including going beyond testing the filtration material.
The current method for testing PPE involves attaching a mask to a flat plate inside a box, using hot wax or putty, and then introducing a test aerosol to measure penetration levels. To achieve certification from the National Institute for Occupational Safety, 20 masks of the same type must be tested. That has proven to be time-consuming. During the pandemic, it resulted in a massive testing backlog for the respirator industry.
However, the team said time was just one issue. The current process doesn’t take into account other factors in mask use.
“All you are doing is testing the filter media itself,” explained Barrick. “It doesn’t test geometry, how the respirator fits on a face, how it’s moved on and off multiple times, how the straps perform, how the nose bridge performs, how the mask can wear over time.”
There was also the issue of reuse of PPE. With such a worldwide shortage, frontline workers were forced to reuse respirators designed for single use. However, there was no standard method of testing mask reuse.
“I think there were a lot of lessons learned with everyone suddenly looking at what the industry standards were,” Omana said.
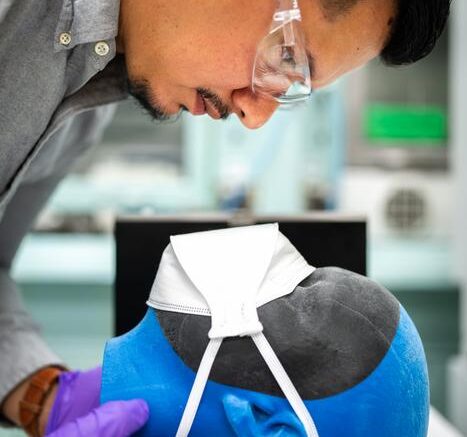
The team had a new idea to speed up the process and make it more effective. They started by creating a model of a human face that could be loaded into a commercial filter test system.
“We wanted quicker testing and to look at more features, like how does the mask fit on a face,” Salzbrenner said. “We used 3D printing capabilities to make it more pliable, like skin.”
Once the mask is affixed to the form, the tester applies pressure to give an airtight seal and then introduces the aerosol.
But the team agreed even more could be done. The current testing standards don’t take into account how a real person might wear a mask and the gaps or flaws that a mask might present in real-life conditions. So, they developed a more complex version using a complete human head.
Once the mask is affixed, the entire head is put in an airtight box that is then placed in the machine and tested, allowing for a more natural flow of air over the mask and what they believe is a more realistic picture of mask performance.
The mechanical engineers on the team then took things one step further to help address the reuse of PPE, something there is currently no testing standard for.
“We developed the chamber version to automate donning and doffing (the putting on and taking off of an item) to test respirator function over time, a predominant factor in wear on a mask. It also mimics how a mask is set on the face and shows you any gaps that air and particles can get past,” Salzbrenner said.
The team said this can be used in addition to the other testing models they created or developed to be an all-in-one tester. All of which would be a big advance in the way PPE is tested in the U.S. as well as other countries.
“I call it holistic testing,” Omana said. “It takes into account all of the aspects of the mask. Aerosols are like electricity and take the path of least resistance. Even if the filter media is doing great, if another subcomponent is failing, the PPE can be rendered useless. Current testing standards do not quantitatively test PPE in a real-use capacity. This emulates the real-world use of PPE.”
The team is now working to further test their approach with the help of $100,000 in funding from Sandia’s Technology Maturation Program. The goal is to license out the science to a company that can produce it on a commercial level. That is part of Sandia’s tech transfer initiative.
The saying “Necessity is the mother of invention” is no truer than in this instance. This invention was created during one of the most impactful pandemics in history, at a time when countless lives were at stake. And like so many times before, when the world has a problem, those at Sandia try to tackle it.
“Without the diverse capability of people at Sandia, a project like this would not have happened.” Salzbrenner said. “If you look at the background of each of the people on this team, everyone comes from a different discipline or walk of life. It was a combination of all these people who made these things happen.”
“As a national lab, we are fortunate to have some of the brightest minds, and with that expertise we felt it was our responsibility to do something to help the community,” Barrick added.
The team said one of the best parts of this project is that it happened organically.
“Everyone just jumped in to help,” Barrick said. “When we needed an answer, someone would say, ‘I know who can answer that.’ We would contact that someone and they would get involved. The amazing thing about this is that people donated their time. People worked more than was asked of them, to help solve this problem. It really was out of the goodness of their hearts. This was a call to action.”
Source: Sandia National Laboratories