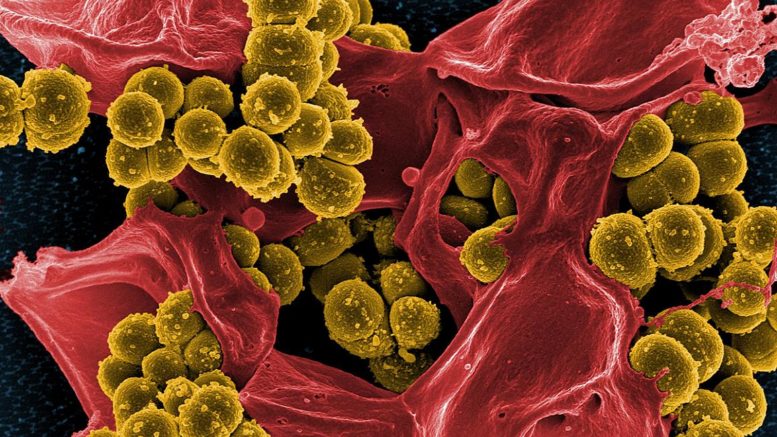
Although there is a growing concern and policy regarding infections or colonization caused by resistant bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), the prognosis of MRSA infections compared to that of methicillin-susceptible Staphylococcus aureus (MSSA) infections remains controversial. Moreover, there have not been any studies comparing both the burden of disease and its impact on the healthcare economy between MRSA infection and colonization while adjusting for confounding factors, Hirabayashi, et al. (2024) say. These comparisons are crucial for developing effective infection control measures and healthcare policies. The researchers aimed to compare the disease and economic burden between MRSA and MSSA infections and between MRSA infection and colonization.
The researchers retrospectively investigated data of 496 in-patients with MRSA or MSSA infections and of 1178 in-patients with MRSA infections or MRSA colonization from a university hospital in Japan from 2016 to 2021. They compared in-hospital mortality, length of stay, and hospital charges between in-patients with MRSA and MSSA infections and those with MRSA infections and MRSA colonization using multiple regressions. They combined surveillance data, including all microbiological test results, data on patients with infections, treatment histories, and clinical outcomes, to create the datasets.
There was no statistically significant difference in in-hospital mortality rates between matched MRSA vs. MSSA infections and MRSA infection vs. colonization. On the contrary, the adjusted effects of the MRSA infection compared to those of MSSA infection on length of stay and hospital charges were 1.21-fold (95% confidence interval [CI] 1.03–1.42, P = 0.019) and 1.70-fold (95% CI 1.39–2.07, P < 0.00001), respectively. The adjusted effects of the MRSA infection compared to those of MRSA colonization on length of stay and hospital charges were 1.41-fold (95% CI 1.25–1.58, P < 0.00001) and 1.53-fold (95% CI 1.33–1.75, P < 0.00001), respectively. Regarding confounding factors, hemodialysis or hemofiltration was consistently identified and adjusted for in the multiple regression analyses comparing MRSA and MSSA infections, as well as MRSA infection and MRSA colonization.
MRSA infection was associated with longer length of stay and higher hospital charges than both MSSA infection and MRSA colonization. Furthermore, hemodialysis or hemofiltration was identified as a common underlying factor contributing to increased length of stay and hospital charges.
Reference: Hirabayashi A, et al. Comparison of disease and economic burden between MRSA infection and MRSA colonization in a university hospital: a retrospective data integration study. Antimicrobial Resistance & Infection Control. Volume 13, article number 27 (2024).