The demand for donated organs has already exceeded supply, with patients waiting months and sometimes years for a donor. With so many people testing positive for SARS-CoV-2, a new study published in the Transplant Infectious Diseases could provide help for the shortage of donated organs by using an organs from a SARS-CoV-2-positive donor.
To evaluate the safety of transplants from SARS-CoV-2-positive organ donors, Providence Swedish researcher Jason Goldman, MD, MPH, who is an infectious disease physician at the Organ Transplant and Liver Disease Center at Providence Swedish Hospital in Seattle, led a group of more than two dozen national experts from the Organ Procurement and Transplantation Network (OPTN) ad hoc Disease Transmission Advisory Committee to conduct the largest study on the question of whether it was safe to receive an organ from a SARS-CoV-2 positive donor.
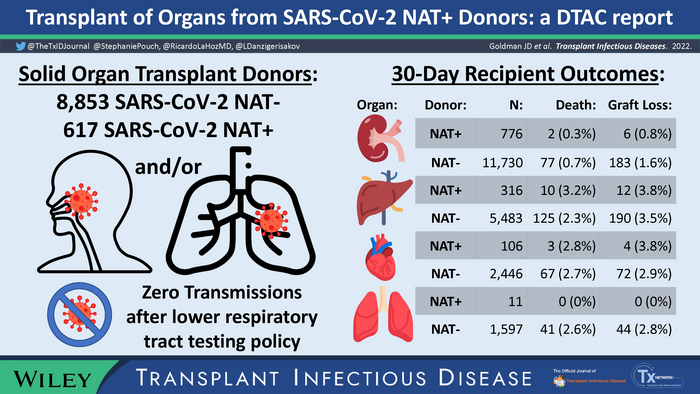
The study involved an investigation of data including all U.S. donors and transplant recipients in the national database, as well as cases referred to the committee for review of possible transmission from donor to recipient. Their review assessed 30-day outcomes for 1,241 transplant recipients from a donor testing positive for SARS-CoV-2, and 21,948 organ donors without a positive virus test. The analysis found that non-lung transplant recipients from positive donors have 30-day graft and patient survival rates like those using donors negative for SARS-CoV-2.
The researchers also evaluated the impacts of a 2021 emergency policy requiring Organ Procurement Organizations to conduct lower respiratory track (LRT) testing for SARS-CoV-2. The policy was launched in late May 2021 after the Centers for Disease Control and Prevention (CDC) and the Disease Transmission Advisory Committee identified three cases where SARS-CoV-2 was passed to lung transplant recipients from the donor, after upper respiratory tract testing failed to identify the donors’ COVID-19 infections.
A retrospective analysis of all donors recovered and recipients transplanted in the U.S. looked at the national data between May 27, 2021, when the new LRT policy took effect, and January 31, 2022. Not only did the research team find that no probable or proven cases of COVID-19 transmission had occurred to recipients of non-lung organs (such as kidneys, livers and hearts), they also found zero transmissions of COVID-19 to lung transplant recipients after the new policy requiring lower respiratory track testing in lung donors took effect.
“Our findings are particularly heartening for patients and providers grappling with the dual challenges of an organ shortage and uncertainty about the safety of organ transplants during the COVID-19 pandemic,” explains Goldman. “Early guidance for transplant programs recommended avoiding donors who recently tested positive for SARS-CoV-2. However, this study provides key evidence that in most cases, transplants from SARS-CoV-2-positive donors can be used with excellent short-term outcomes.”
Source: Providence Swedish