Researchers at the Uniformed Services University in collaboration with University of Washington, have recently uncovered new details about how Nipah and Hendra viruses infect cells and the immune responses that can block them, which could ultimately lead to the development of new tactics to prevent and treat these deadly illnesses.
In this latest study published in Science, Dr. Christopher Broder, professor and chair of USU’s Department of Microbiology and Immunology, study lead and senior author Dr. David Veesler, associate professor of biochemistry at the University of Washington School of Medicine and a Howard Hughes Medical Investigator, together with other researchers, were able to determine a new three-dimensional structure of a critical component of the Nipah viruses’ infection mechanism – the G glycoprotein tetramer – as it interacted with a fragment of a broadly neutralizing antibody. Importantly, they also observed that a “cocktail” of antibodies worked better together to disarm both Nipah and Hendra viruses, and also helped keep escape mutants from emerging to sidestep the antibody response.
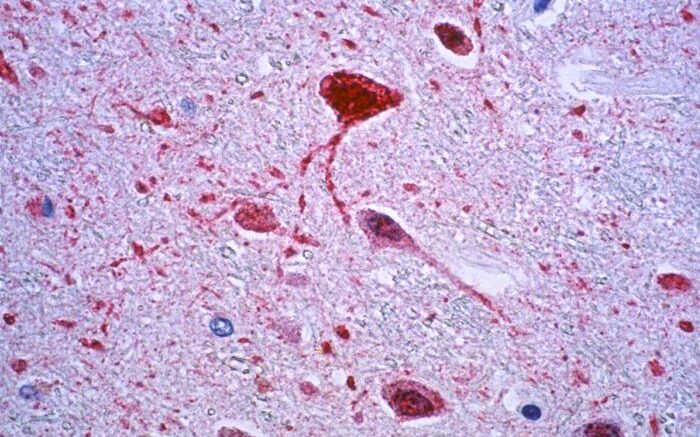
Both Nipah virus and Hendra virus – henipaviruses – emerged in the 1990s and are carried by bats native to certain parts of the world. They have jumped species and can infect many other mammals, including humans and have caused serious disease outbreaks in people and livestock in Australia, Malaysia, Singapore, Bangladesh and India. The viruses cause brain inflammation (encephalitis) and respiratory illness. Recent Nipah outbreaks have resulted in greater than 75 percent case fatality rates among people.
Nipah and Hendra viruses infect cells using attachment and fusion glycoprotein spikes, which work in a coordinated fashion to gain entry. These glycoproteins are also the key targets for the antibody defense system. Currently, there is a vaccine against Hendra virus approved for use in horses in Australia based on the attachment G glycoprotein (HeV-sG), and a modified version of this vaccine that is effective against Nipah virus has recently entered a human clinical trial, but there isn’t a henipavirus vaccine approved for human use.
New attempts to design life-saving preventives and treatments have become even more urgent after a new strain of Hendra virus was discovered a few months ago in Australia, where Hendra virus has caused outbreaks 65 times since its discovery in 1994. Outbreaks of Nipah virus have appeared nearly every year over the past two decades in Bangladesh, and Nipah virus disease has also been seen in India and the Philippines.
Broder’s lab has been studying the Hendra and Nipah virus glycoproteins for more than two decades, and his team’s earlier work includes the HeV-sG vaccine. Up until this study, the researchers said, it was unclear how the complete structure of a critical portion of these viruses elicited such a diverse antibody response.
“These findings provide additional critical and very detailed insights on the nature of what we think is the most important henipavirus vaccine component, and for producing the next-generation of vaccines to protect against these deadly viruses,” according to Broder. Ongoing henipavirus vaccine research led by Broder’s group will be able to incorporate these new findings going forward, and include new platforms designed for single dose vaccination that can be rapidly deployed in outbreak settings for protection of people and response personnel.
“We are delighted that our work informs vaccine and therapeutic design against these deadly pathogens," Veesler said.
The research took place in Veesler’s lab at the University of Washington and the Broder lab at Uniformed Services University. The lead author is Zhaoqian Wang, a University of Washington graduate student in biochemistry.
Source: Uniformed Services University of the Health Sciences