Recent SARS-CoV-2 variants such as BA.4 and BA.5 developed abilities missing from the first Omicron variants that allowed them to overcome humans’ innate immunity, according to research from University College London (UCL).
The study, published in Nature Microbiology, examined viral evolution in eight Omicron variants to better understand how the virus has reacted since the introduction of vaccinations1. It found that earlier Omicron variants such as BA.1 lost mechanisms to overcome innate immunity but that later variants regained this ability, suggesting a common evolutionary strategy that has implications for pathogen surveillance.
Since the beginning of the COVID-19 pandemic, new variants of concern emerged independently from the first wave SARS-CoV-2 virus. Alpha, Delta and then Omicron in turn became the dominant variants in circulation.
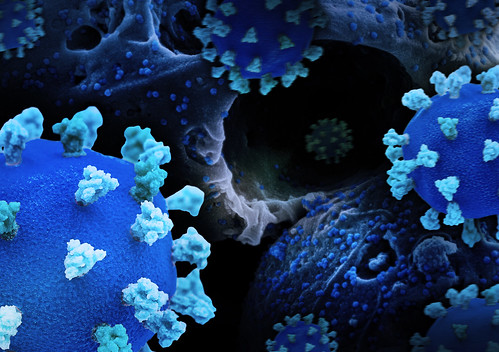
Previous work showed that Alpha and Delta evolved to overcome human innate immunity, our first line of defense against infections, by jamming the cellular signaling in the airways that triggered our antiviral immune response. This buys the virus time to establish itself in the body and overwhelm our second line of defense, the adaptive immunity developed as a result of prior infection or vaccination. If it is successful, viral particles will enter cells and replicate, causing illness in the host.
Unlike Alpha and Delta, the evolution of SARS-CoV-2 Omicron was driven by the pre-existing immunity in the global population as a result of vaccination and prior infection. This adaptive immunity creates antibodies that recognize features on the virus’ spike protein, and protects cells from infection in a process called neutralization.
In this study, researchers at UCL and the University of Glasgow used cell models to observe how eight different SARS-CoV-2 Omicron sub-variants interacted with their human host.
They found that the earliest Omicron variants, BA.1 and BA.2, were less able to overcome human innate immunity than Alpha or Delta. More recent Omicron variants, such as BA.5 and XBB, have relearned how to overcome human innate immunity and have done so in the same way as Alpha to Delta.
Dr. Ann-Kathrin Reuschl, first author of the study from UCL Division of Infection & Immunity, said, “We were surprised to find that early Omicron subvariants were relatively bad at evading innate immunity compared to Alpha and Delta. This seemed like a backward step in SARS-CoV-2 evolution and may explain reports of reduced disease severity when these variants were dominant. Like Alpha to Delta, we found that the most recent Omicrons have increased the amount of innate immune antagonist proteins that they make, for example nucleocapsid and Orf6. The fact that later Omicron variants evolved in the same way as Alpha and Delta underlines how the innate immune system really is an effective gatekeeper for SARS-CoV-2 variant success.”
To overcome innate immunity these later Omicron variants produce greater quantities of certain viral proteins, such as nucleocapsid and Orf6, that help to jam the cellular signaling pathways that triggers our antiviral response.
Professor Greg Towers, a senior author of the study from UCL Division of Infection & Immunity, said, “This study helps us understand how a pandemic coronavirus adapts to its new human host and suggests how the virus will evolve in the future, fine tuning immune escape by changing its spike and protein levels to maximize human-to-human transmission. The success of BA.1 and BA.2 without the same capacity to overcome innate immunity suggests that avoiding innate immunity may be less important than avoiding neutralizing antibodies for SARS-CoV-2 human-to-human transmission, but that it remains an important part of the virus’ strategy.”
The findings help to explain why SARS-CoV-2 remains so capable of infecting people despite existing immunity from vaccines and prior infection. An effective way to avoid infection is to wear FFP3 masks or similar that can protect from virus breathed out by infected individuals.
Professor Clare Jolly, a senior author of the study from UCL Division of Infection & Immunity, said, “With SARS-CoV-2 we’ve had a unique opportunity to observe how a virus evolves to overcome our defenses in real time, giving us an opportunity to predict what a virus with pandemic potential needs to do to be successful. This may help us to assess the risk posed to humans by emerging viruses or new variants of existing viruses. It will be important to continue to monitor the virus as it continues to evolve.”
Source: University College London