Dapper, et al. (2022) report that the first detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in Germany was reported in early February 2020. In addition, extensive control measures on the coronavirus disease 2019 (COVID-19) pandemic have been placed in Germany since March 2020. These include contact and travel restrictions, distance rules, mandatory wearing of face masks and respirators, cancellation of mass events, closures of day-care centers, schools, restaurants and shops, isolation measures, and intensified infection control measures in medical and long-term care facilities. The researchers note, "Changes in demand or access to healthcare services and intensified control measures can lead to changes in transmission dynamics and imply effects on the overall occurrence of infectious diseases in hospitals."
To analyze the impact of infection control measures implemented in public on infectious diseases in hospitals, surveillance data from Marburg University Hospital were analyzed retrospectively. The analysis was conducted from January 2019 to June 2021, referred to hospital occupancy and mobility data in the county of Marburg-Biedenkopf, and correlated to control measures in hospitals and the general population.
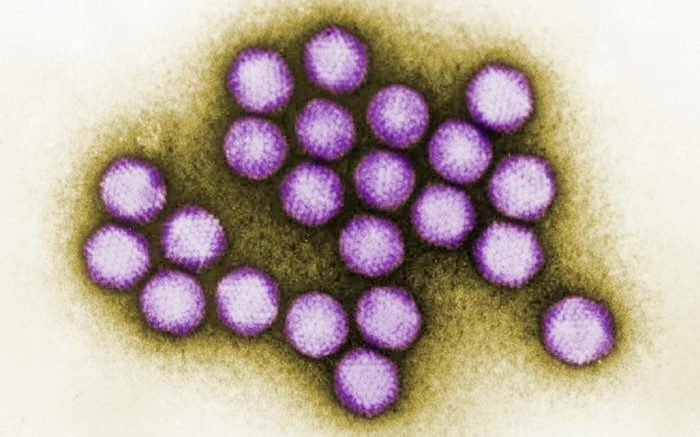
The COVID-19 pandemic and associated measures immediately impacted the occurrence of infectious diseases at the Marburg University Hospital. Significant changes were detected for virus-associated respiratory and gastrointestinal diseases.The massive drop in norovirus infections was significantly affected by the onset of the pandemic (P = 0.028). Similar effects were observed for rotavirus (up to − 89%), respiratory syncytial virus (up to − 98%), and adenovirus infections (up to − 90%). The decrease in gastrointestinal and respiratory virus detection rates was significantly affected by the decline in mobility (P < 0.05). Of note, since April 2020, there have been no detected influenza cases. Furthermore, Clostridioides difficile-related infections declined after late 2020 (− 44%). In contrast, no significant changes were detected in the prevalence of susceptible and drug-resistant bacterial pathogens. In particular, the detection rates of methicillin-resistant Staphylococcus aureus isolates or multidrug resistant (MDR) and extended drug resistant (XDR) bacteria remained constant, although the consumption of hand disinfectants and protective equipment increased.
The researchers note that the COVID-19 pandemic and associated public health measures had a significant impact on infectious diseases and the detection of pathogens at the Marburg University Hospital. Significant changes were observed for community transmissible infections, while no such effects on pathogens primarily associated with nosocomial transmission could be detected.
Reference: Dapper L, et al. Influence of public health and infection control interventions during the severe acute respiratory syndrome coronavirus 2 pandemic on the in-hospital epidemiology of pathogens: in hospital versus community circulating pathogens. Antimicrobial Resistance & Infection Control. Vol. 11, article number 140 (2022)