In their research article published in Eurosurveillance, von Schreeb et al. challenge existing assumptions regarding the relationship between the use of HIV pre-exposure prophylaxis (PrEP) and the incidence of bacterial sexually transmitted infections (STI). According to the concept of sexual risk compensation, the start of PrEP treatment – a drug regimen which effectively prevents acquiring HIV – is associated with rises in STI as people feel protected against HIV while using it. However, von Schreeb et al. argue that available studies that have looked into the empirical foundation for the concept of sexual risk compensation related to PrEP use, have reported mixed results.
And while von Schreeb et al. also describe an increase in overall STI incidence linked to PrEP use during their study in the Danish capital region, they claim that the association “is not indicative of risk compensation."
The specific Danish setting with a unique civil registration number of the study participants in combination with comprehensive databases of STI test results for incidence data both before and after PrEP initiation, provided a data infrastructure for this study that allowed the researchers to investigate the timing of changes in STI incidence in relation to PrEP initiation, in order to investigate possible causality.
In their prospective cohort study with 1,494 participants (99% self-reported cismen and less than 1% transgender or non-binary) from the Danish capital region, 1,326 started PrEP during the study period and had at least one follow-up STI test, with the majority of the participants being on a daily treatment regimen (only 0.6% on-demand PrEP use).
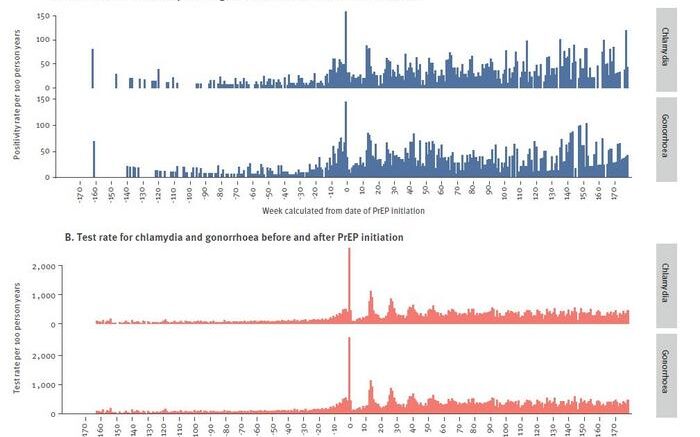
Von Schreeb et al. compared STI incidence before and after the initiation of PrEP and in their cohort, PrEP use was linked to a more than twofold increase in the incidence of chlamydia, gonorrhoea and syphilis: during the observation time and prior to starting PrEP, the incidence rate of any STI (gonorrhoea, chlamydia or syphilis) was 35.3 per 100 person-years, equivalent to 708 STI diagnoses, and the incidence rate rose to 81.2 STIs per 100 person-years (1,849 diagnoses) during reported use of the treatment.
Overall, PrEP was associated with a 35% higher risk of contracting any STI, which is consistent with findings from similar studies. The authors note that in Denmark, increases in STIs associated with PrEP start are associated to both older and younger individuals.
However, the authors highlight that their data indicate the detected rise in STI incidence happened before PrEP treatment was started, at around 10–20 weeks prior to it. This leads to their hypothesis that “if risk compensation was valid, we would expect STI incidence to increase when people feel protected against HIV. This increase could occur either immediately following the initiation of PrEP, or gradually over time, as they become more assured of the treatment’s protective effect. As no such increase was seen, an alternative interpretation to the association between PrEP and STIs is that changes in sexual risk-taking lead people to PrEP.”
Von Schreeb et al. conclude, based on their study results, that the “findings suggest that individuals frequently seek PrEP during periods when they are at increased risk of contracting STIs. This makes PrEP programmes a critical point of intervention, both for preventing HIV and STIs.”