Helicobacter pylori (H. pylori) is an infectious bacterium that resides in the gastric mucosa and causes persistent gastric damage. H. pylori can cause chronic gastritis, peptic ulcers, and iron deficiency anemia. If left untreated, it can also lead to the development of stomach cancer. The World Health Organization classifies H. pylori as a Class I carcinogen.
Recently, researchers from China conducted an exhaustive review of the clinical trajectories of various treatments (e.g., bismuth-containing quadruple therapy (BQT), dual therapy (DT), and standard triple therapy) that have historically been used to combat H. pylori infection. The review has been published in the Chinese Medical Journal, issue 1, 2023.
Senior author Xiuli Zuo, a distinguished professor at Qilu Hospital, Shandong University, China, says, “In recent years, the eradication rate of H. pylori has reached >90% using DT, which has been used not only as a first-line treatment but also as a rescue treatment. Compared with BQT, DT has great potential for H. pylori eradication; however, it has some limitations. This review summarizes the development of DT and its application in H. pylori eradication.”
To this end, the research team retrieved studies indexed on Pubmed. The articles cited by these studies were also scrutinized to ensure the inclusion of all the associated relevant studies.
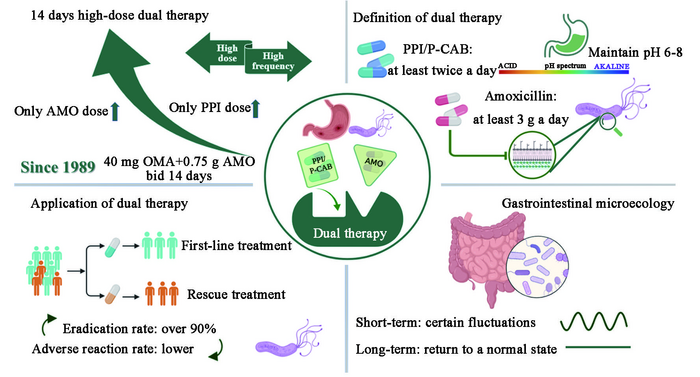
The history of DT dates back to 1989, when Swiss researchers conducted a double-blind pilot study. As part of this study, the clinicians began exploring the use of a combination of 40 mg omeprazole—a proton pump inhibitor (PPI) commonly used for treating gastroesophageal reflux disease and peptic ulcer disease—and 750 mg amoxicillin—a penicillin antibiotic. Patients were asked to take this combination twice a day, for a period of 14 days. The eradication rate was only 62.5%, but this trial laid the foundation for DT.
A German study conducted in 1993 was much more promising. Clinicians administered 20 mg omeprazole twice a day (bid) and 500 mg amoxicillin four times a day (qid) to patients with H. pylori-positive duodenal ulcers for a period of 14 days. The eradication rate of H. pylori increased to 78.9%, and, interestingly, the healing rate of duodenal ulcers was 100%. Thereafter, clinicians started opting for DT as the first-choice treatment for H. pylori eradication in patients with duodenal ulcers. In the year 1995, when clinicians increased the dose of amoxicillin to 750 mg (thrice a day; tid) and that of omeprazole to 40 mg (tid), they observed a 91% eradication of H. pylori infection in patients with duodenal ulcers. However, the team notes that this type of treatment has received limited attention.
Recent developments have shown significant promise. For instance, a meta-analysis based on 41 randomized controlled trials (RCTs) involving 14,119 patients showed that 14-day high-dose DT (concomitant high-frequency administration of at least one acid suppressor and 3,000 mg of amoxicillin) has good efficacy and patient compliance and few adverse events, making it the most ideal first-line treatment for H. pylori infection in the Asian population.
High-dose and high-frequency DT has several advantages. For instance, the elevated pH makes H. pylori more susceptible to being killed as it enters the reproductive phase. The increased PPI dosage and frequency also help address the issue arising from the variable CYP2C19-mediated PPI metabolism in the liver. Moreover, the acid-suppressing-medication and the antibiotic exhibit a synergistic effect, and jointly eradicate the H. pylori infection with a high degree of efficacy.
According to the review, amoxicillin is the most preferred antibiotic in DT owing to several reasons such as ultra-low H. pylori resistance rate, fewer adverse effects, and optimal excretion. Moreover, DT that is administered for 14 days produces remarkably better results than DT that is administered for shorter durations. In fact, multiple studies clearly demonstrate that high-dose DT has a higher H. pylori eradication rate and a lower incidence of adverse events among all other therapies.
Recent advances in medicine have also had a profound effect on DT. For instance, first-generation PPIs such as omeprazole are now being replaced with more efficacious second-generation PPIs, such as esomeprazole and rabeprazole. Furthermore, based on a 2022 meta-analysis including 668 patients with H. pylori infection and a few other studies, clinicians are also recommending the use of a combination of vonoprazan and amoxicillin (VA-DT) for a period of 14 days.
DT is a safe and efficacious therapeutic option; however, it has not been researched extensively outside Asia, especially in Europe and the United States. Moreover, DT cannot be recommended to patients who are allergic to penicillin. Although H. pylori eradication may causes certain fluctuations in the gastrointestinal microbiota, in the long term, the gastrointestinal microbiota eventually returns to its normal state. DT has also demonstrated good patient compliance.
Lead author Miao Duan, also from Qilu Hospital, Shandong University, concludes, “Overall, DT has a great prospect in clinical practice; however, studies with large sample sizes and multi-center clinical trials are needed to corroborate these findings.”