Antibiotic overuse can lead to antibiotic resistance, but classic antibiotic resistance might not completely explain why antibiotics sometimes fail. Sub-populations of bacteria called persister cells are capable of surviving in the presence of lethal doses of antibiotics for prolonged periods. Although persister cells have been intensively researched, evidence linking them to poor patient outcomes has been limited.
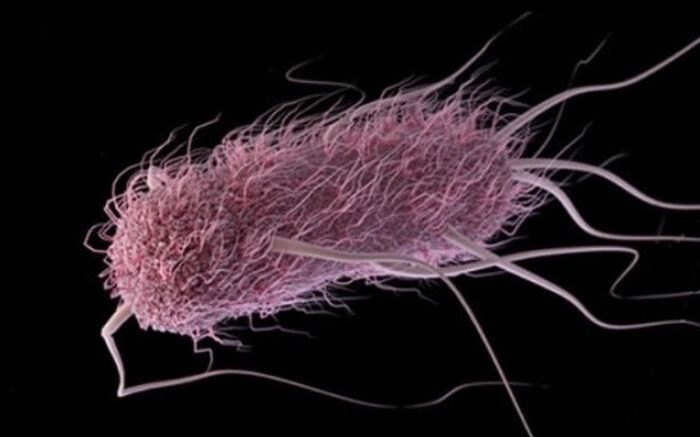
Scientists led by UNC School of Medicine microbiologist Brian Conlon, PhD, and Duke School of Medicine infectious diseases fellow Josh Parsons, MD, PhD, have now shown that E. coli can evolve in patients to produce increased persister cells and this leads to increased survival to antibiotics. Publishing their work in the Proceedings of the National Academy of Sciences (PNAS), Conlon and colleagues used a combination of patient data, clinical isolates and animal models to show that persister cells contribute to antibiotic failure when classic antibiotic resistance does not explain such failure.
“For decades, many scientists around the world have studied persister formation, and we have continually been challenged to provide evidence for real-world importance,” said Conlon, senior author and associate professor of microbiology and immunology. “We think our paper is the strongest evidence supporting the importance of persister cells in the clinic.”
Scientists and doctors have been sounded the alarm that overusing antibiotics – especially when doctors are not certain a patient is suffering from a bacterial infection – is making our arsenal of antibiotics less effective, leading to what we call antibiotic resistance, a global concern.
But some scientists have long thought antibiotic failure might not be that simple and that additional factors were required to understand antibiotic treatment failure, particularly where antibiotic resistance was not identified. Some of these scientists study persister cells, which are sub-populations of bacteria that can withstand antibiotics for a prolonged period of time. Despite a wealth of scientific literature on the subject, Conlon said it remained unclear how much, if at all, this persister phenomenon contributed to antibiotic treatment failure in the clinic. Through a collaboration with Duke researchers Josh Thaden, MD, PhD, and Vance Fowler, Jr., MD, Conlon’s lab decided to conduct stepwise research to investigate the possible role of persister cells in antibiotic failure.
Using clinical E. coli bacteremia isolates – bacteria from the blood of patients – Conlon, first author Joshua Parsons, MD, PhD, an infectious diseases fellow at Duke University, and colleagues found that high-persister mutants evolved in patients. The researchers then documented a 100-fold increase in persisters in one such mutant when challenged with the exact antibiotic doctors had used to treat patient from which the E. coli had been isolated.
The mutant bacteria showed no loss of fitness in a mouse infection model and displayed a 10-fold increase in survival following antibiotic challenge.
Importantly, Conlon said his team documented the infections and treatment protocols of patients who had been prescribed antibiotics to clear E. coli infections. In patients who did not clear infection with antibiotics, Conlon said that classical antibiotic resistance was not responsible for the poor outcomes.
“Because of this research, we think persister formation is likely a significant contributor to antibiotic treatment failure in patients,” Conlon said. “Our research strongly suggests that persister formation is an important metric to consider when treating patients with antibiotics.”
He also said that researchers should develop techniques to identify mutants that are likely to respond poorly to antibiotics because such information would influence treatment choices or duration of treatment. Additionally, the development of new therapeutic approaches to target and kill persisters may improve treatment outcomes in patients.
Along with Conlon and Parsons, authors of the PNAS paper are Ashelyn Sidders, Amanda Velez, Michelle Angeles-Solano, and Sarah Rowe at the UNC School of Medicine; Blake Hanson at the University of Texas Health Science Center; Felicia Ruffin, Joshua Thaden, and Vance Fowler Jr. at Duke University; and Cesar Arias at Cornell University.
Source: University of North Carolina Health Care System