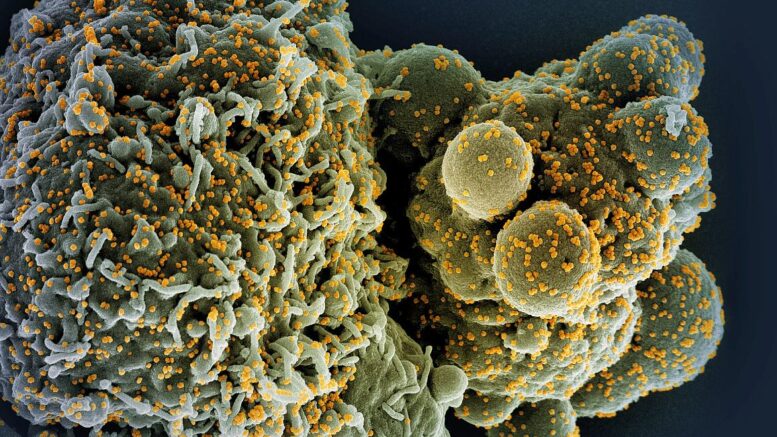
Severe COVID-19 may cause long-lasting alterations to the innate immune system, the first line of defense against pathogens, according to a small study funded by the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. These changes may help explain why the disease can damage so many different organs and why some people with long COVID have high levels of inflammation throughout the body. The findings were published online in the journal Cell.
Researchers led by Steven Z. Josefowicz, PhD, of Weill Cornell Medicine in New York City examined immune cells and molecules in blood samples from 38 people recovering from severe COVID-19 and other severe illnesses, as well as from 19 healthy people. Notably, the researchers established a new technique for collecting, concentrating and characterizing very rare blood-forming stem cells that circulate in the blood, eliminating the need to extract such cells from bone marrow.
In these rare stem cells—the parents of immune-system cells—taken from people recovering from COVID-19, the scientists identified changes in the instructions for which genes got turned on or off. These changes were passed down to daughter cells, leading them to boost production of immune cells called monocytes. In the monocytes from people recovering from severe COVID-19, the changes in gene expression led the cells to pump out greater amounts of molecules called inflammatory cytokines than monocytes from people who were healthy or had non-COVID-19 illnesses. The researchers observed these changes as much as a year after the participants came down with COVID-19. Due to the small number of study participants, the scientists could not establish a direct association between the cellular and molecular changes and health outcomes.
The investigators suspected that an inflammatory cytokine called IL-6 might play role in establishing the changes in gene-expression instructions. They tested their hypothesis both in mice with COVID-19-like disease and in people with COVID-19. In these experiments, some of the subjects received antibodies at the early stage of illness that prevented IL-6 from binding to cells. During recovery, these mice and people had lower levels of altered stem cell gene-expression instructions, monocyte production and inflammatory cytokine production than subjects that didn’t receive the antibody. In addition, the lungs and brains of mice that received the antibodies had fewer monocyte-derived cells and less organ damage.
These findings suggest that SARS-CoV-2 can cause changes in gene expression that ultimately boost the production of inflammatory cytokines, and one type of those cytokines perpetuates the process by inducing these changes in stem cells even after the illness is over. Additionally, the findings suggest that early-acting IL-6 is likely a major driver of long-term inflammation in people with severe COVID-19. These findings shed light on the pathogenesis of SARS-CoV-2 infection and may provide new leads for therapies. The results also underscore the importance of staying up to date with recommended COVID-19 vaccines, which are proven to protect against serious illness, hospitalization and death.
Reference: JG Cheong et al. Epigenetic memory of coronavirus infection in innate immune cells and progenitors. Cell DOI: 10.1016/j.cell.2023.07.019(link is external) (2023).
Source: National Institutes of Health (NIH)