Throughout the COVID-19 pandemic and when maximum protection is needed against air-born infections, the N95 respirator has remained the gold standard of personal protective equipment. However, it is also much more difficult to produce and obtain than a standard surgical mask.
But a recent study published in PLOS ONE demonstrates that a simple modification to a surgical mask using rubber bands can improve its protective seal against particle exposure to the level of an N95 respirator.
To achieve N95-level protection, the respirators should demonstrate a minimum score of 100 on a standardized battery of tests – the Occupational Safety and Health Administration’s passing threshold – against the passage of particles that would potentially expose an individual to disease. Standard surgical masks are not as protective because they don’t seal around the wearer’s face, allowing particles to bypass the filter peripherally.
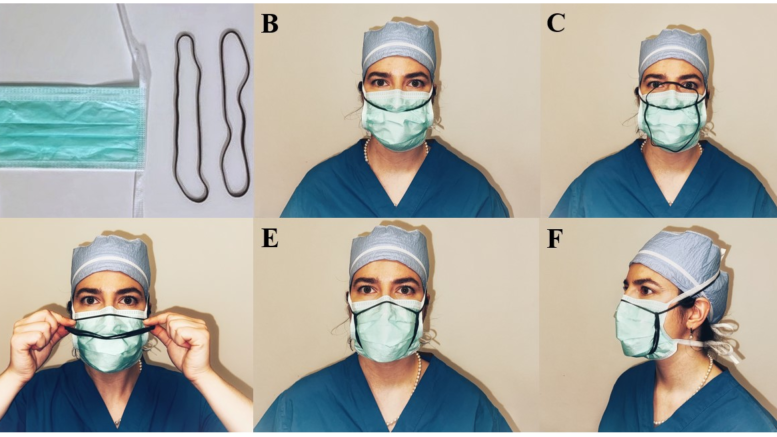
A research team led by a Michigan Medicine surgeon worked with 40 healthcare workers to test standard surgical masks modified with two 8-inch rubber bands over the crown of the subject’s head, bridge of the nose, around the cheeks and under the chin within the boundaries of the mask.
Thirty-one of the subjects, or 78%, had modified masks that passed a fit test with a score of greater than 100. The passing masks scored an average of 151, a significantly better fit than an unmodified surgical mask score of 3.8 but lower than a properly fitted N95 mask’s score of 199. By the last day of investigation, all of the modified masks passed the N95 threshold, suggesting that greater experience with the banding improved fit and performance.
This easy modification could address N95 respirator shortages worldwide and provide health care workers and individuals in under-resourced regions – or even in a resourced area like the U.S. when production demands can’t properly meet needs in a pandemic – a practical means for increased personal protection, said Jaimo Ahn, MD, PhD, FACS, senior author of the paper and professor of orthopaedic surgery at University of Michigan Medical School.
“While not a vaccine, this approach emphasizes prevention rather than treatment,” Ahn said. “While not sophisticated, it has the potential to save lives and preserve wellness. Its effect will last as long as there are respiratory diseases and PPE demand exceeds supply. It is immediately impactful and sustainable, yet simple and cheap.”
Additional authors include Agnes Z. Dardas, M.D., Viviana M. Serra Lopez, M.D., Lauren M. Boden, M.D., Taras Grosh, M.D., Daniel J. Gittings, M.D., Kevin Heym, and Emily Koerber, all of the University of Pennsylvania at the time the study was performed.
Reference: “A simple surgical mask modification to pass N95 respirator-equivalent fit testing standards during the COVID-19 pandemic,” PLOS ONE. DOI: 10.1371/journal.pone.0272834