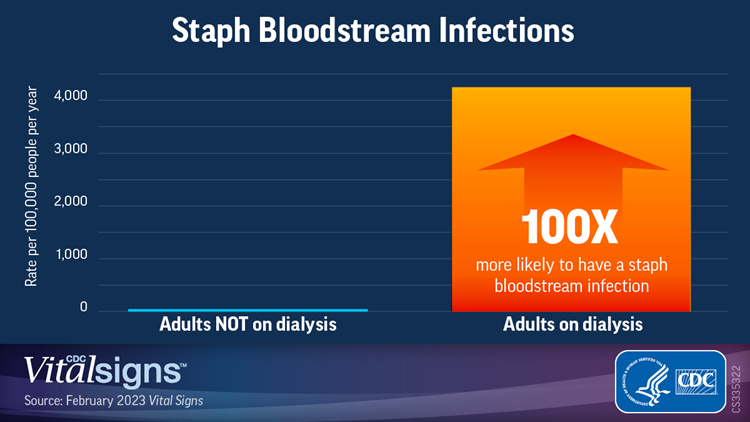
Adults on dialysis treatment for end-stage kidney disease were 100 times more likely to have a Staphylococcus aureus (staph) bloodstream infection than adults not on dialysis during 2017–2020, according to a new Vital Signs report released by the Centers for Disease Control and Prevention (CDC).
More than half of people in the U.S. receiving dialysis belong to a racial or ethnic minority group—about 1 in every 3 people receiving dialysis is Black and 1 in every 5 is Hispanic. CDC data found patients on dialysis in these groups have higher rates of staph bloodstream infections than White patients on dialysis.
Dialysis treatment, although necessary and lifesaving, comes with risks. Healthcare providers use needles or catheters to connect a patient to a dialysis machine, and germs, like staph, can get into a patient’s bloodstream. Staph bloodstream infections can be serious and even deadly. Some infections are resistant to some of the most common antibiotics used to treat them, making the drugs ineffective.
CDC data confirmed one of the key ways healthcare providers can reduce the risk of infection is by using lower-risk alternatives, such as fistulas and grafts, to replace central venous catheters to connect patients’ blood circulation to dialysis machines for treatment.
Hispanic patients on dialysis had a 40% higher risk of staph bloodstream infections than White patients on dialysis between 2017 and 2020. Other challenges for many patients on dialysis include:
• Lack of access to preventive care for conditions like diabetes and high blood pressure, which increase the risk of developing end-stage kidney disease.
• Lack of patient education about treatment options for end-stage kidney disease.
• Extended use of a central venous catheter to connect a patient’s blood circulation to a dialysis machine for treatment (also known as a vascular access type). Catheters have the highest risk of infection among all vascular access types.
• Socioeconomic factors, including poverty, household crowding, and lower education levels.
“Preventing staph bloodstream infections begins by detecting chronic kidney disease in its early stages to prevent or delay the need for dialysis,” said CDC Chief Medical Officer Debra Houry, MD, MPH. “Healthcare providers can promote preventative practices, including methods to manage diabetes and high blood pressure, as well as providing education on treatment options among all patients and particularly those at greatest risk, to slow the progression of chronic kidney disease.”
CDC researchers used data from the 2020 National Healthcare Safety Network (NHSN) and the 2017–2020 Emerging Infections Program (EIP) to describe bloodstream infections among dialysis patients. To examine associations with race, ethnicity, and social determinants of health, these data were linked to population-based data sources (CDC/ATSDR’s Social Vulnerability Index, United States Renal Data System, U.S. Census).
Key findings:
• In 2020, 4,840 dialysis facilities reported 14,822 bloodstream infections to NHSN; 34% were due to staph.
• In both NHSN and EIP systems, vascular access via central venous catheter was strongly associated with staph bloodstream infection.
• Among seven EIP sites in 2017–2020:
o The staph bloodstream infection rate was 100 times higher in dialysis patients than adults not on dialysis.
o Among patients on dialysis, staph bloodstream infection rates were highest in Black and Hispanic patients.
o Adjusting for state of residence, age, sex, and vascular access type, the staph bloodstream infection risk was highest in Hispanic patients and patients 18–49 years old.
o People in areas with higher poverty, household crowding, and lower education had more staph bloodstream infections.
“Dialysis-associated bloodstream infections are preventable—not inevitable,” said Shannon Novosad, MD, MPH, dialysis safety team lead in CDC’s Division of Healthcare Quality Promotion. “Our data show that use of a central venous catheter as a vascular access type had six times higher risk for staph bloodstream infections when compared to the lowest-risk access, a fistula. Prevention efforts that equitably promote lower-risk vascular access types and continued use of infection prevention and control best practices can save lives.”
The good news is that bloodstream infections in patients on dialysis have decreased since 2014 with the widespread use of proven practices to prevent and control infections. Preventing infections among patients receiving dialysis requires a broad and equitable approach to the prevention and care of kidney disease for people from all racial, ethnic, and socioeconomic groups. Healthcare providers and public health professionals should continue to:
• Encourage practices shown to prevent and slow the progression of chronic kidney disease.
• Counsel patients on the potential treatment options before they develop end-stage kidney disease.
• Coordinate efforts between patients, nephrologists, vascular access surgeons, radiologists, nurses, nurse practitioners, and social workers to reduce the use of central venous catheters for dialysis treatment.
• Increase the use of lower-risk vascular access types, such as fistulas and grafts, for people starting and currently on dialysis.
• Use proven practices to prevent and control infections in all U.S. dialysis facilities.
• Reduce barriers for patients receiving medical care by offering transportation assistance, insurance coverage expertise, social work services, and education resources in multiple languages.
To access this report, visit: www.cdc.gov/vitalsigns
Source: CDC