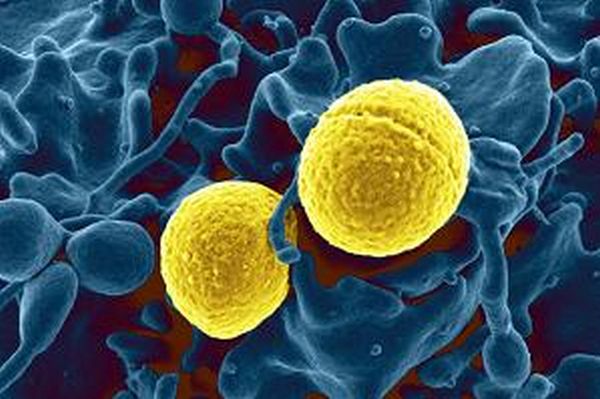
Coagulase-Negative Staphylococci (CoNS) are opportunistic and nosocomial pathogens. The excessive use of antimicrobial agents, including antiseptics, represents one of the world’s major public health problems. This study by Hefzy, et al. (2023) aimed to test the susceptibility of CoNS to antiseptics.
Out of 250 specimens collected from different sections of the hospital, 55 samples were identified as CoNS, categorized into three groups based on their sources: environmental samples (n = 32), healthcare worker carriers samples (n = 14), and clinical infection samples (n = 9). Isolates were examined for susceptibility to antibiotics and antiseptics, such as benzalkonium chloride (BC), cetyltrimethylammonium bromide (CTAB), and chlorhexidine digluconate (CHDG). Mupirocin and antiseptic resistance genes, as well as the mecA gene, were detected using polymerase chain reaction. CoNS isolates with notable resistance to antiseptics and antibiotics were identified using the API-Staph system.
A high frequency of multidrug resistance among CoNS clinical infection isolates was observed. Approximately half of the CoNS isolates from healthcare workers were susceptible to CHDG, but 93% were resistant to BC and CTAB. The frequency of antiseptics and antibiotics resistance genes in CoNS isolates was as follows: qacA/B (51/55; 92.7%), smr (22/55; 40.0%), qacG (1/55; 1.8%), qacH (6/55; 10.9%), qacJ (4/55; 7.3%), mecA (35/55; 63.6%), mupB (10/55; 18.2%), and mupA (7/55; 12.7%). A significant difference in the prevalence of smr gene and qacJ genes between CoNS isolates from healthcare workers and other isolates was reported (P value = 0.032 and ˂0.001, respectively). Four different CoNS species; S. epidermidis, S. chromogene, S. haemolyticus, and S. hominis, were identified by API.
The researchers concluded that CoNS isolates colonizing healthcare workers showed a high prevalence of antiseptic resistance genes, while clinical infection samples were more resistant to antibiotics. CHDG demonstrated greater efficacy than BC and CTAB in their hospital.
Reference: Hefzy EM, et al. Antiseptics and mupirocin resistance in clinical, environmental, and colonizing coagulase negative Staphylococcus isolates. Antimicrobial Resistance & Infection Control. Vol. 12, article number 110 (2023).