mRNA vaccines for COVID-19 generate adverse reactions such as fever and fatigue which are considered normal and are transient in nature. However, there has been a growing fear of taking the mRNA-1273 vaccine prevalent in Japan, due to these unpleasant effects. Now, there is sparse clinical evidence about the relationship between this incidence of fever and antibody counts, especially after the third dose of the vaccine. Professor Yorifuji Takashi and assistant professor Matsumoto Naomi colleagues from Okayama University have investigated this link over a period of time and recently published their findings in a short report in the Journal of Epidemiology.
mRNA vaccines mimic the surface structure of SARS-CoV-2 in the body. Immune cells then treat these as invading pathogens and produce antibodies against them. Thus, antibody counts can be used as a quantitative outcome of the immune system’s response to a vaccine. For their study, the researchers recruited 49 university staff and students as subjects. Only participants who had not previously suffered from COVID-19 (to the best of their knowledge) were selected.
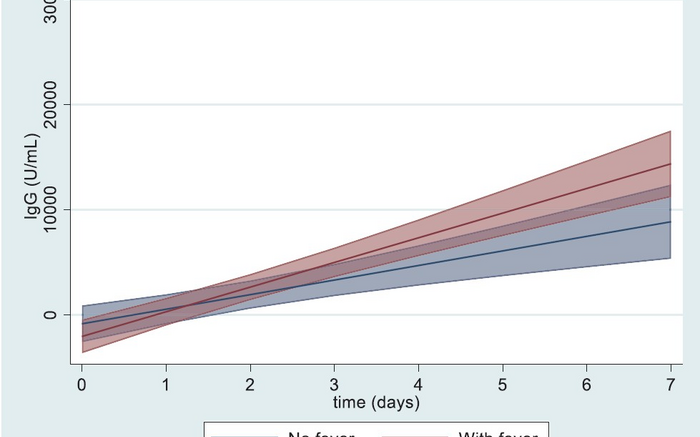
All subjects were surveyed for adverse reactions a week after they received the third mRNA-1273 vaccine dose. Simultaneously, antibody levels of all subjects were measured just before receiving the vaccine, three days after, about one week after, and finally one month after the dose. Using statistical modeling, correlations between the incidence of fever and antibody levels at various time points was stipulated. To account for factors contributing to the onset of fever post-vaccination, the team also looked at sex, age differences, a history of allergy, and the use of antipyretics (fever-reducing drugs) amongst the participants.
The subjects were then classified into a “fever” or “nonfever” group based on the survey results. It was found that the fever group was more likely to be younger (20 to 49 years-old) and had a past history of allergies. Next, antibody levels at different time points in the two groups were analyzed. At 1 week post vaccination, the fever group had substantially higher antibody counts than the nonfever group. However, at 1 month post vaccination there seemed to be no correlation between the incidence of fever and high antibody levels.
This is the first study to highlight associations between the induction of fever and antibody levels at various time points after the third dose of the mRNA-1273 vaccine. “Antibody titers after mRNA-1273 vaccination may be faster in the group with post-vaccination fever, but the difference may not be significant 1 month post-vaccination,” concludes the team. The researchers also suggest that while these contradictory observations may not have significant clinical relevance, a study with a larger sample size might provide better insights.
mRNA vaccines come with a set of instructions to produce viral proteins in our body. mRNA-1273 enters our cells and produces the spike protein — a protein found on the surface of SARS-CoV-2. Our immune cells then recognize this protein as a foreign object and produce antibodies against it, which will build over time. These are known as antibody titers. If a vaccinated individual is infected with SARS-CoV-2 in the future, the immune cells will immediately recognize the spike protein and ramp up production of these antibodies to fight off the infection.
Due to the extensive involvement of the immune system, mRNA vaccines tend to produce symptoms such as fatigue, fever, headaches, and body aches. There is also a theory that chemicals known as lipids, which protect and deliver the mRNA molecules, might aggravate the immune response. Since the onset of fever and an increase in antibody titers are both a function of vaccine-induced immune reactions, a link between the two might have important clinical significance.