By George Clarke
A fundamental problem in the healthcare industry is the opinion that environmental services (ES) staff serves as “just the cleaner, the janitor or the housekeeper.” This couldn’t be further from the truth. In fact, the healthcare ES staff – we prefer the designation Environmental Hygiene Specialist – are a crucial, yet all too often unheralded, factor in preventing drug-resistant infections.
According to the Centers for Disease Control (CDC), on any given day, one in 31 hospital patients has at least one healthcare associated infection (HAI). A recent study in the American Journal of Infection Control shows that Clostridium difficile infection (CDI), just one of many types of superbug infections, can result from the bacteria found on hospital environmental surfaces. Without proper cleaning of such surfaces, cross-contamination can occur, resulting in a preventable HAI (pHAI). The study showed that, with the proper ES protocols in place, CDI rates fell to zero over the course of 1,000 patient days. This is just the latest in a growing body of research highlighting the role played by ES staff in reducing HAIs.
Moreover, new standards and regulations from the Center for Disease Control and Prevention (CDC) and Association for the Healthcare Environment encourage hospitals to agree to and implement ES cleaning programs and total facility cleaning standards to clean and disinfect all high-touch surfaces.
In response to such research and recommendations, leading healthcare organizations are starting to recognize the importance of ES staff as part of an enterprise-wide multimodal intervention plan to combat such infections. As a result, all types of healthcare facilities – from acute-care hospitals to assisted living facilities – are elevating the role of cleaning and disinfecting processes to ensure the health and safety of patients, caregivers and their staff.
Below are the crucial factors in any ES program.
ES Staff Training and Recognition
Texas State University clinical microbiologist Rodney E. Rohde, PhD, says that distinguished ES Hygiene Specialists as among one of the most important “behind-the-scenes” professions in combatting HAIs and superbugs in healthcare systems and the community at large. In A Secret Weapon for Preventing HAIs, Rohde wrote that ES comprises the “first-line-of-defense specialists whose training has included learning best practices for effective infection prevention.”
Training programs recognize the science of cleaning and disinfecting that ES performs – both the clinical function of removing and inactivating/killing HAI-producing microbes, and the practical function of cleaning. ES staff training should include:
• Proper use of high-performance, reusable textile products and ergonomic tools
• Color-coded, one-per-room methodologies that simplify training, help reduce chemical usage, and – most important – offer a straightforward and elegant way to eliminate the risk of cross-contamination
• Improved cleaning thoroughness and enhanced cleaning methods of high-touch surfaces
More and more, healthcare management is acknowledging and rewarding ES staff that have undergone extensive in-service training in which participants learn best practices for infection prevention and hygiene management in the patient room, OR and throughout the healthcare facility. Such recognition serves as a significant employee morale boost. Once ES staff complete training, senior management supported and attended events offer an opportunity to present a certificate, pin or other designation, recognizing the ES staff members efforts and commitment to providing safe patient environments.
High-Performance, Reusable Products
High-performance, reusable textiles benefit from ongoing research and development of innovative fibers and materials. They deliver unrivaled performance, including absorbency, extremely high wet strength and far more versatility. The uncontested benefit of high-performance, reusable micro-denier fiber products is their ability to remove everything that can be physically removed from an environmental surface – some have the proven ability to remove the endotoxins released by bacteria when killed with disinfectant.
Such reusable micro-denier textiles usually are processed by experienced hospital linen processors, either on-premises or outsourced – following ARTA, CDC, OSHA, Healthcare Laundry Accreditation Council (HLAC) or TRSA recommended laundry processes. To counter a fictitious claim frequently made by disposable manufacturers, if recontamination were an issue with reusables, then hospitals would be overwhelmed with contaminated sheets, scrubs, incontinence pads, sheets, etc., that often are grossly contaminated with human excrement, vomit and BBP’s (blood borne pathogens). The fact is, according to the CDC, contamination of the patient environment from laundered textiles rarely, if ever, happens.
Disposable mops and wipers, on the other hand, provide limited performance in removing pathogens from an environmental surface. The majority are made from 100 percent polyester fiber imported from China and are primarily used as a vehicle to get the disinfectant/chemical onto a surface.
Moreover, depending on the disposable product selected, the increase in cost ranges from three to more than twelve times that of using a reusable wiper.
Disinfectants to Support the Healthcare Wiper Cycle
An oft-overlooked topic is the disinfectants being used and how they are incorporated throughout the healthcare cleaning cycle. The mop or wiper cycle is repeated every day in every healthcare facility. This is the typical scenario:
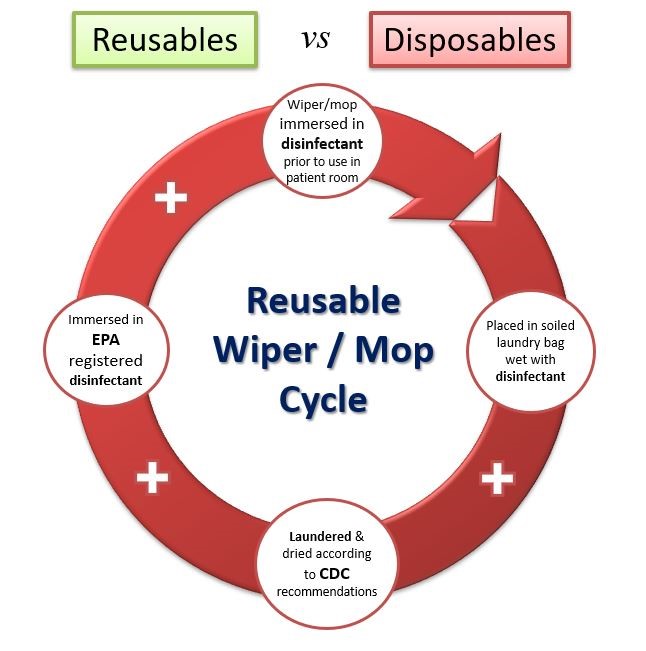
• The standard practice for a reusable mop or wiper is the “dip and wring” method. Clean products are folded and stacked in a pail and immersed in an EPA registered disinfectant. The wiper is then used in the patient room – ideally, following a color-coded methodology.
• Products are put damp (or still wet) in a closed soiled laundry bag with other damp wipers and transported to the laundry. Often, they wait many hours, if not days, to be laundered — thus far exceeding any recommended dwell time for any disinfectant.
• Then, the reusables are laundered by an experienced healthcare laundry, typically processing to CDC and/or OSHA recommendations for blood borne pathogens, then dried at recommended temperatures.
• Before going back into any patient room, the flat mops and wipers are again immersed in an EPA-registered disinfectant.
Given this process, how is it possible that any viable organism survived this entire cycle and re-contaminated a patient room? The only conclusions possible are, either the disinfectant is not living up to its efficacy claims or, most likely, the disposable manufacturers have intentionally neglected to take the disinfectant into consideration.
Currently, bleach-free, EPA-registered sporicidal disinfectants are available that achieve CDI sporicidal disinfection in four minutes or less. As they are not bleach products, they do not corrode hard surfaces and are safer for workers due to their low Hazardous Materials Identification System (HMIS) health rating of one. Such solutions — effective against a broad range of microorganisms including CDI spores, hepatitis B, TB and norovirus — are easier for ES staff to use, more sustainable with packaging, a longer shelf life, and very economical.
A Final Thought: Key Considerations to Support ES Staff
In the best healthcare settings, C-suites are beginning to grasp the difference a highly trained ES staff member can make not only in the lives of patients, but also in the facility’s reputation, goodwill and financial health.
ES staff serves as the first line of defense in ensuring safe environments in hospitals and long-term care facilities, thereby helping protect the broader community. Those who recognize this by investing in these unsung heroes will improve patient outcomes, boost financial health, increase satisfaction rankings and support the community at large. Some key points to keep in mind:
• Adopt an enterprise wide multi-modal approach to reducing pHAIs
• Invest in proper training of ES staff
• Engage with and recognize ES staff for their critical role in infection prevention
• Leverage high-performance, proven textiles and disinfectants for cleaning and infection prevention
Overcoming the lack of knowledge of the unheralded ES professional is critical in the battle against antibiotic resistant superbugs. The next time you’re in a healthcare facility, take a moment to recognize those who are keeping the environment safe via proper cleaning and disinfection protocols. They are as important as doctors and nurses in maintaining your public health and safety.
 George Clarke is CEO of UMF Corporation.
George Clarke is CEO of UMF Corporation.

Be the first to comment on "Environmental Services Staff: The First Line of Defense in the War Against Preventable HAIs"