By Kelly M. Pyrek
This article originally appeared in the December 2019 issue of Healthcare Hygiene magazine.
A potential nationwide shortage of ethylene oxide (EtO) has triggered investigation in early November by the Food and Drug Administration (FDA) into viable industrial sterilization alternatives that can mitigate the impact of medical device shortages.
“The recent closure of a Sterigenics ethylene oxide sterilization facility in Illinois, the temporary closure of another Sterigenics facility in Georgia, and the potential closure of a large Becton Dickinson sterilization facility in Georgia could affect the availability of some sterile medical devices used by healthcare delivery organizations and patients,” said Norman E. Sharpless, MD, acting commissioner of food and drugs at the Food and Drug Administration (FDA), in a statement issued by the agency in late October. “We have been working diligently with impacted device manufacturers and healthcare delivery organizations to ensure that they are aware of these developments and preparing to minimize adverse effects on patients whose care could be negatively affected if medical devices sterilized at these large facilities were not accessible.”
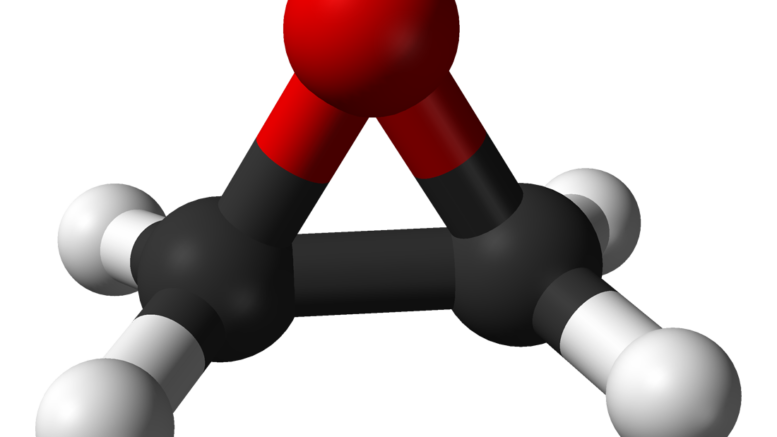
According to the FDA, EtO is the most common method of sterilization of medical devices in the U.S., and that more than 20 billion devices sold in the U.S. every year are sterilized with it, accounting for approximately 50 percent of devices that require sterilization.
“Without adequate availability of ethylene oxide sterilization, we anticipate a national shortage of these devices and other critical devices including feeding tube devices used in neonatal intensive care units, drug-eluting cardiac stents, catheters, shunts and other implantable devices,” Sharpless said. “It’s important to note at this time there are no readily available processes or facilities that can serve as viable alternatives to those that use ethylene oxide to sterilize these devices. In short: this method is critical to our healthcare system and to the continued availability of safe, effective and high-quality medical devices.”
In the quest to identify potential alternatives, in early November the FDA assembled the General Hospital and Personal Use Devices Panel of its Medical Devices Advisory Committee. During panel deliberation on the first day of the two-day meeting, panel members discussed that, if EtO sterilization is reduced, eliminated or replaced to a different sterilization modality, there are options that can mitigate the impact of medical device shortages. The panel’s consensus was that the FDA should prioritize stakeholder communication and work to facilitate validation of sterilization processes.
The panel discussed how the FDA can help mitigate device shortages due to reduced device sterilization capabilities. The panel’s consensus reemphasized the need for stakeholder communication and collaboration to help manage shortages, including working collaboratively with other government entities, on the federal and state level. The panel also recommended that it may be appropriate to enhance the FDA’s ability to respond to device shortages by incorporating processes currently used with drug shortages that would necessitate additional authorities for FDA.
The panel deliberated on the possibility of changing EtO sterilization cycles or sterilization loads to reduce EtO use while maintaining effective sterilization. The panel’s consensus was that there were potential methods that appeared viable, but no single method would address all issues and that manufacturers and contract sterilizers should pursue all applicable methods for reducing EtO use.
The panel considered various methods to validate EtO sterilization cycles in hopes of reducing EtO-use while still maintaining an effective sterilization process. The panel recommended that FDA encourage the use of alternatives to the overkill validation method which are included in the consensus standards for EtO sterilization processes.
The panel discussed the sterilization of some medical devices to a less rigorous sterility assurance level (SAL) (e.g. 10-5, 10-4, etc. instead of 10-6) be considered as part of the approach to reduce sterilant use. The panel’s consensus was that consistent with current standards, the FDA should consider moving to a risk-based assessment of the SAL for some sterilized medical devices.
The advisory panel also recommended that the FDA evaluate sterility assurance levels for medical products to reduce EtO emissions, an unavoidable byproduct of its use.
"The FDA recognizes that there are concerns associated with release of ethylene oxide into the environment if emissions were to occur at unsafe levels,” Sharpless said. “Concerns about ethylene oxide emissions have resulted in certain state actions against sterilization facilities that are currently impacting manufacturers’ ability to use the ethylene oxide process to sterilize their medical devices. In February, the FDA became aware that the Illinois Environmental Protection Agency (EPA) issued a state EPA order to stop Sterigenics from sterilizing medical products and other products with ethylene oxide at their Willowbrook, Ill. facility. The state EPA order was due to the presence of levels of ethylene oxide higher than the EPA found to be acceptable in the air around the facility. This closure caused a temporary shortage of pediatric breathing tubes. Another Sterigenics contract sterilization facility in Atlanta has been closed since August while it undergoes construction to reduce ethylene oxide emissions. In October, the Sterigenics Willowbrook, Ill., facility announced they would not reopen. Because of these two large sterilization facilities being unavailable, the FDA continues to coordinate with multiple stakeholders on any impacts to medical device availability and to communicate with Sterigenics and medical device companies that may be affected. Because the number of ethylene oxide contract sterilization facilities in the U.S. is limited, we are very concerned that additional facility closures could severely impact the supply of sterile medical devices to health care delivery organizations that depend on those devices to take care of patients. The impact resulting from closure of these and perhaps more facilities will be difficult to reverse, and ultimately could result in years of spot or nationwide shortages of critical medical devices, which could compromise patient care.”
The FDA has urged medical device manufacturers that use EtO facilities to assess their inventory for any potential downstream impacts of sterilization facility closures on their product distribution. Sharpless said that if U.S. manufacturers are not able to resolve a shortage and it involves a critical device needed for U.S. patients, the FDA may look for a firm that is willing and able to redirect safe and effective product into the U.S. market to address a shortage. The FDA also has encouraged healthcare facilities to perform similar inventory assessments of critical medical supplies that undergo contract terminal sterilization via EtO so that the agency can assist in identifying potential substitute devices.
“Hospitals and other healthcare delivery organizations should also work with their purchasing departments, group purchasing organizations and distributors to help obtain product needed for patient care.” Sharpless urged facilities not to hoard product or attempt to purchase larger quantities of devices beyond their normal purchase volume.
At the November hearings, Jonathan Wilder, PhD, managing director of Quality Processing Resource Group, LLC, told the panel that the severity of medical device shortages depend on a number of factors, including, device type and intended use; the population impacted; device misallocation and hoarding; and the effectiveness of mitigation measures.
Wilder said the decision to sterilize medical devices using EtO is typically made due to excellent product penetration, reliability of EtO, in that there is an established compatibility with the process and a long history of validated processing for the materials used. Additionally, the size of the industrial/contract sterilizer chambers enables economical sterilization.
Wilder summarized that some materials currently sterilized in EtO cannot be migrated to radiation sterilization or to steam or dry-heat sterilization. As well, the effects of high-temperature sterilization can make migration of otherwise-compatible devices impossible. He added that the logistics and equipment for thermal sterilization differ from EO greatly and that it would require significant capital and time to implement if medical devices were migrated to these methods.
Retaining EtO sterilization as a viable option is an imperative, says ECRI Institute, an independent, non-profit patient safety organization, which adds that statewide bans of commercial EtO sterilization could result in widespread shortages of critical medical devices and supplies, significant harm to patients
ECRI Institute says that it opposes a total ban of commercial EtO sterilization because it could result in widespread shortages of sterile medical devices.
“Even a partial ban on ethylene oxide could cripple the delivery of healthcare in the United States as critical medical-surgical supplies would suddenly become unavailable,” says Marcus Schabacker, MD, PhD, president and CEO of ECRI Institute, referring to sterilization plant closures, a proposed EtO sterilization ban in Illinois, and a 2016 report by the Environmental Protection Agency (EPA) regarding possible health risks from EtO emissions.
“While environmental health concerns certainly need to be addressed, legislators and the public should be aware that an ethylene oxide ban could severely impact the safe delivery of healthcare,” Schabacker adds. “Without access to medical supplies, many surgeries and procedures would not be possible.”
For more than 50 years, the medical device industry has relied on ethylene oxide to sterilize temperature- and moisture-sensitive disposable medical devices, such as syringes, IV bags, and wound dressings, and lifesaving devices, such as stents and catheters. These medical device materials and packaging were developed for EtO sterilization. ECRI Institute says it knows of no safe alternative commercial sterilization methods that could immediately replace EtO at this time.
In written comments submitted to the FDA, Ruey C. Dempsey, vice president of technology and regulatory affairs at the Advanced Medical Technology Association (AdvaMed), stated that, “For many medical devices, due to their material composition, size, shape or complexity, EtO is the only effective method for sterilization. EtO provides the ongoing capacity and scale to process the billions of medical devices required by today’s modern healthcare systems in delivering care to patients. Heart valves, pacemakers, implantable cardioverter/defibrillators, drug-eluting stents, feeding tubes and breathing tubes, surgical drapes and kits, and syringes are just a few of the many products critical to modern patient care that can only be sterilized using EtO. Ethylene oxide’s compatibility and effectiveness with the plastics and polymers commonly used in medical products allows for the sterilization of many medical devices that would otherwise be rendered ineffective or unsafe if sterilized by radiation, moist heat, dry heat, or other alternative methods.”
Dempsey continued, “Medical device manufacturers have invested in microbiologists, sterility assurance experts, process safety and environmental engineers; and industrial hygienists who have worked for decades to ensure that they have standards and controls in place to responsibly manage the use of EtO. Manufacturers must conduct exhaustive studies to demonstrate that the required sterility assurance levels are achieved and maintained by their equipment and processes, and to confirm that exposure to the sterilization process does not adversely affect the device’s performance, safety or effectiveness over the shelf life of the device. At the same time, AdvaMed member companies are committed to further reducing the amount of EtO used for effective sterilization processes by actively exploring methods and processes that reduce the amount of EtO used for a sterilization cycle. The industry is committed to investigating alternative sterilization methods that will provide the same sterility assurance and result in the same device performance as EtO. Until there is a safe and effective replacement for EtO, we will continue to pursue our goal to reduce the amount of EtO used. Optimizing the EtO process itself, the medical device packaging and the approach to validation are examples of possible ways to minimize the amount of EtO sterilant necessary to sterilize devices. However, none of these potential solutions can be achieved quickly or easily. Any change to minimize EtO use, if even feasible, would likely require extensive product and/or process modifications; validation and verification testing; potential facility upgrades; and required notifications, clearances and approvals from FDA.”
In her written comments to the FDA, Linda Rouse O'Neill, vice president of government affairs for the Health Industry Distributors Association (HIDA), stated, “HIDA members share a close relationship with our manufacturer partners and together we ensure the many medical devices that go through distribution and ultimately contact with patients and healthcare providers are both safe and effective. Part of that process is ensuring their sterility, a critical component in preventing infections and ensuring the integrity of the device. HIDA recognizes that the task of studying and implementing proper safety guidelines on a process this complex and with an impact on an industry as critical as ours … Due to material sensitivities, EtO is the only option for sterilizing a large number of life-saving and life-enhancing devices, primarily those made of plastics or containing electronics, that cannot tolerate exposure to the extreme temperatures, radiation and moisture present in other sterilization methods. The effect of steam and radiation on anti-microbial coatings on single-use plastic devices makes them an unacceptable alternative. Material integrity and degradation and damage to sensitive, sophisticated electronic devices and their components are also major concerns. Given the sensitive nature of the devices and the sterilization involved, the entire process is regulated by the FDA - where the use of EtO has been validated as a vital sterilization process. As a low-temperature sterilizer, ethylene oxide gas won’t damage the types of medical devices described below. Ethylene oxide also is used to sterilize other healthcare products such as bandages and ointments, reducing potential damage to the product that may occur from other means of sterilization.”
Rouse O'Neill adds, “Our manufacturing partners conduct exhaustive studies to validate that the required sterility assurance levels are achieved by the process and to confirm that exposure to the sterilization process does not adversely affect the device’s performance, safety or effectiveness. HIDA is profoundly concerned about a host of unintended consequences – such as product shortages and the inability to sterilize critical healthcare products. These would likely arise for the healthcare supply chain and the patients they serve as a result of any swift change in policy regarding the use of currently approved sterilization techniques. Most devices sterilized with EtO have no acceptable alternative, putting the supply chain at significant risk without this vital mode of sterilization. Banning or heavily restricting the use of EtO would require the identification and validation of an alternative method, which currently does not exist. Additionally, it may require the redesign of many medical devices, and many products would require major changes to product design, material selection, manufacture and distribution. The redesign process could take several years and require lengthy regulatory approval. The direct impact of any elimination or severe restriction would potentially threaten the entire health care system, as low product inventories and severe backorders of sterile single-use devices could result, putting patients at risk.”
In addition to shortage-mitigation efforts, the FDA has addressed the broader need for innovation and improvements to medical device sterilization techniques by announcing two new-innovation challenges to encourage ideas from stakeholders, academics, industry and others about novel solutions for improving sterilization processes, including alternatives to using EtO.
It is important to note that the Advisory Committee meeting convened by the FDA focused on industrial sterilizers and industrial sterilization processes, not hospital sterilizers, including those using EtO. However, during the hearings it was proposed that hospitals consider taking on a share of the industrial sterilization effort. Experts from the hospital sterile processing arena asserted the already-considerable burden of existing in-house medical device disinfection and sterilization services that sterile processing departments provide.
Susan Klacik, a clinical educator with the International Association Of Healthcare Central Service Materiel Management (IAHCSMM), pointed out the significant differences between industrial sterilization, in that pre-conditions loads for days in environmentally controlled rooms, while healthcare facilities do not. Other differences exist between sterilization cycles, loading patterns and aeration. Additionally, manufacturers sterilize items using a standard load configuration and industrial loads are scheduled, and healthcare facilities require a manufacturer’s IFU to process items.
Klacik also pointed out at the FDA hearings that for hospitals to even consider such an undertaking, additional space would be needed for the sterilizers, for preparation, inventory holding, and load quarantine – a luxury many healthcare facilities do not have or can afford.
Additionally, Klacik confirmed that many older facilities would be unable to accommodate this additional needed space and transformations. As well, the healthcare EtO infrastructure needs – including dedicated exhaust, monitoring and documentation of ventilation rates, vent system alarms, a dedicated, separate room, environmental monitoring, and engineering controls to reduce emissions, per ANSI/AAMI ST41:2008 – could be problematic for healthcare institutions.
“We simply don’t have the space; the logistics in the hospital are very difficult; we need to focus on patient transport, and we don’t have the labor to (perform additional EtO sterilization), either.”
At the November hearings, Klacik explained that EtO is effective but not available in most healthcare facilities and pointed out that EtO use is burdensome in parts of the country, in that some states require abatement. She added that the total sterilization cycle time is 15.5 hour or greater, making EtO a challenging option. Furthermore, implementation of EtO can be costly for healthcare institutions, including the cost of sterilizer and supporting infrastructure expenses.
Klacik reviewed for hearing attendees the solutions for the present-day challenges, including:
- Disposable scopes
- Disposable end caps/tips
- Include the clearly defined processing time in IFU/marketing
- Mandate that adequate processing time be allotted for sterile processing personnel
- Increase use of quality-control monitoring tools (inspection, cleaning verification)
- Addition of new types of low-temperature modalities specifying the exact scope model for the specific sterilization cycle
- If sterilization is mandated, time will be needed for implementation
- Routine scheduled-service inspections
Regarding new innovations, Klacik recommended:
- Development of new products less complex to process
- Development of scopes that can be disassembled
- Use materials that can be thoroughly cleaned
- Use materials and designs that can undergo steam sterilization
- Use materials that can readily identify debris and defects
- Provide IFU that are less complex and comprehensible
- Provide education and training on new products, especially new technology
- Recommend sterilization for duodenoscopes over a period
Be the first to comment on "FDA Scrutinizes EtO Shortage, Viable Sterilization Alternatives at Recent Hearings"