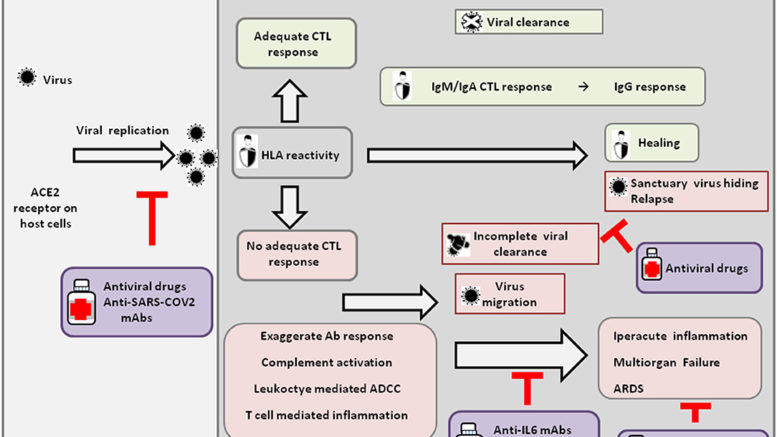
Figure 1. Host response and possible outcomes of SARS-CoV-2 infection. Viral infection seems to occur mainly upon SARS-CoV2 engagement of angiotensin I converting enzyme 2 (ACE2), which acts as a functional receptor for the spike glycoprotein of the coronavirus. The HLA genetic system acts as a key player in determining the anti-viral immune response. In particular, the ability of HLA to trigger an adequate cytotoxic T-lymphocyte (CTL) response will result in viral clearance and host healing, along with the development of the IgM, IgA, and IgG humoral response. Conversely, an inadequate HLA asset will result in an inefficient CTL response and, consequently, incomplete viral clearance. In this context, various factors underlie increased COVID-19 severity, including an exaggerated Ab response, complement activation, leukocyte-mediated antibody-dependent cell-mediated cytotoxicity (ADCC), and T-cell-mediated inflammation, as discussed in the text. Without a protective immune response, the virus is able to migrate, propagating into other ACE2-expressing tissues, while the damaged lung cells induce high inflammation, triggering the cytokine storm that represents the main cause of the acute respiratory distress syndrome (ARDS) and subsequent multiorgan failure. Incomplete viral clearance can also lead to virus hiding in sanctuary sites and patient relapse with symptoms arising in new districts. In the purple boxes, different therapeutic approaches aimed at targeting either the virus or endogenous host players are represented.
On March 11, 2020, the World Health Organization declared coronavirus disease (COVID-19) a pandemic. In a few weeks the infection spread across the globe causing hundreds of thousands of deaths worldwide. Italy was the first European country to be hard-hit by the infection and among the countries with a higher mortality rate.
During the lockdown, Antonio Giordano, MD, PhD, founder and director of the Sbarro Institute for Cancer Research and Molecular Medicine at Temple University in Philadelphia, in collaboration with the University of Siena, Italy, reasoned about the possible causes of the heavy burden of infection in Italy and teamed up with researchers from different fields to investigate the possible causes. In an Opinion article published today in Frontiers in Immunology, the authors describe the main features of COVID-19 clinical course; the possible underlying mechanisms that contribute to exacerbate patient outcome; and the various strategies that can be adopted to tackle the disease and its complications.
In particular, the authors, anticipating their preliminary findings, put the spotlight on the Human Leukocyte Antigen (HLA) gene system, which has a key role in shaping the antiviral - innate and acquired - immune response. The authors, including Pierpaolo Correale and Rita Emilena Saladino, of the Grand Metropolitan Hospital of Reggio Calabria, Giovanni Baglio, of the Ministry of Health,
Francesca Pentimalli, of the National Cancer Institute ‘Pascale,” and Patrizia Maiorano, of the University of Siena, suggest that a specific immunogenetic asset constituted by particular variants of HLA genes could underlie susceptibility to the SARS-CoV-2 coronavirus, or predict a worse disease outcome.
“The identification of such immunogenetic determinants would be crucial to inform priorities in future vaccination campaigns, to decide clinical management strategies, and to isolate genetically at risk individuals, including healthcare workers,” says Luciano Mutti, MD, an oncologist and adjunct professor at the Sbarro Institute.
The study also raises another interesting possibility regarding the spreading of the infection in Italy, in which the northern region of the country, where the disease had been detected first, was most heavily hit. Although a massive migration from the affected regions to the south was recorded before the national lockdown, the southern regions registered much lower infection rates. However, it has been postulated that the virus was circulating long before the lockdown. While some have proposed that milder climate conditions could help to prevent viral spreading, could a specific immunogenetic asset contribute to protect southern Italian citizens? Further large-scale case-control studies will hopefully shed light on this possible aspect.
Source: Sbarro Health Research Organization
Be the first to comment on "Genetics May Explain High COVID-19 Mortality in Italy, Inform Global Pandemic Response"