To study how best to treat potentially dangerous infections commonly seen in people with underlying chronic medical conditions, two infectious disease experts at Johns Hopkins Medicine have been awarded $10 million in research funding over five years by the Patient-Centered Outcomes Research Institute (PCORI).
PCORI is an independent, nonprofit organization authorized by Congress in 2010. According to the institute, its mission is “to fund research that will provide patients, their caregivers and clinicians with the evidence-based information needed to make better informed healthcare decisions.”
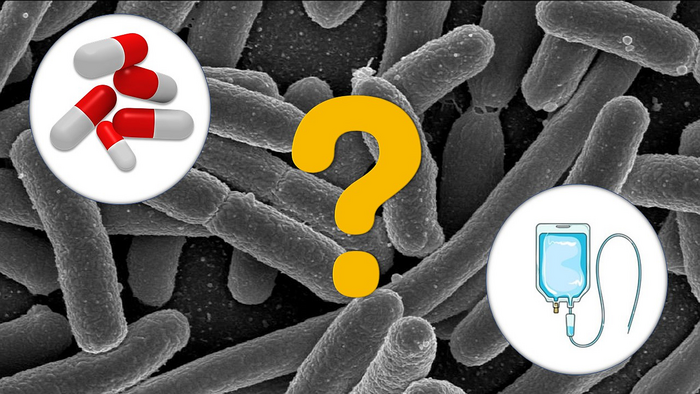
The award will support a randomized controlled clinical trial at eight U.S. hospitals involving a study population of approximately 1,200 patients with bloodstream infections caused by gram-negative bacteria, such as Escherichia coli.
Gram-negative bacteria are organisms that are not colorized by the Gram staining method used to differentiate bacteria into two distinct groups: gram positive and gram negative.
“According to previous studies, an estimated 1 in 5 patients with chronic medical conditions will develop a gram-negative bloodstream infection during their lifetime,” says study co-principal investigator Sara Cosgrove, MD, director of the Johns Hopkins Hospital Department of Antimicrobial Stewardship Program and professor of medicine at the Johns Hopkins University School of Medicine. “Urinary tract infections, intra-abdominal infections, pneumonia, diabetic foot infections and vascular catheter infections can all lead to gram-negative bloodstream infections.”
The study’s co-principal investigator is Pranita Tamma MD, MHS, director of the pediatric antimicrobial stewardship program at Johns Hopkins Children’s Center and associate professor of pediatrics at the Johns Hopkins University School of Medicine.
“Traditionally, gram-negative bloodstream infections have been treated with intravenous [IV] antibiotics for the duration of a patient’s therapy — either in the hospital or with placement of a vascular catheter to continue treatment at home or a skilled nursing facility,” says Tamma. “However, because vascular catheters used to place IV lines can pose a risk of a secondary infection and other complications, and because IV therapy imposes limitations on patient mobility and quality of life, we want to see if oral antibiotic treatment — pills — given at an early stage in the process could achieve outcomes on par with those of IV antibiotics.”
In their clinical trial, Cosgrove, Tamma and colleagues will randomize patients into one of two groups: those who receive IV antibiotics for the entire duration of therapy and those who start with IV therapy followed by early transition to oral antibiotics for the remainder of the treatment course.
The study, says Tamma, will be conducted at eight hospitals strategically selected because they meet the following criteria: a mix of urban, suburban and rural populations; geographic distribution across the United States; racially and ethnically diverse populations; and the necessary infrastructure to participate in a large randomized controlled trial.
The investigators, says Cosgrove, will use a novel analytical approach to determine efficacy and safety, using criteria developed by both patients and healthcare providers. “This will enable us to define the optimal treatment approach for patients with gram-negative bloodstream infections,” she explains.
Source: Johns Hopkins Medicine