A Phase 3 clinical trial evaluating the antiviral tecovirimat, also known as TPOXX, is now enrolling adults and children with monkeypox infection in the United States. Study investigators aim to enroll more than 500 people from clinical research sites nationwide. Interested volunteers can visit the ACTG website (clinical trial A5418) for more information. The trial is sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health. The NIAID-funded AIDS Clinical Trials Group (ACTG) is leading the study, which may later expand to international sites. The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) at NIH is supporting several sites, including through the International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT).
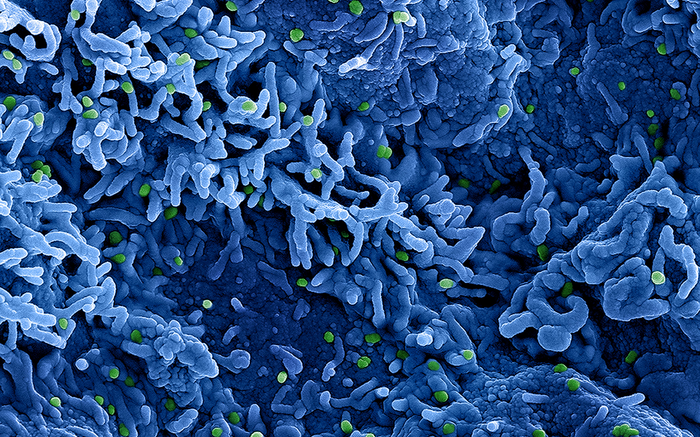
Tecovirimat, manufactured by the pharmaceutical company SIGA Technologies, Inc. is approved by the Food and Drug Administration for the treatment of smallpox. The drug prevents the virus from spreading in the body by preventing virus particles from exiting human cells by targeting a protein found on both the variola virus, which causes smallpox, and the monkeypox virus. Clinicians currently can access tecovirimat for U.S. patients with monkeypox through an expanded access or “compassionate use” request process.
An outbreak of human monkeypox virus, first identified in May 2022, prompted public health emergency declarations from both the World Health Organization (WHO) and the U.S. Department of Health and Human Services this past summer. The majority of cases identified thus far have been in men who have sex with men, although other populations, including women and children, can become infected. From Jan. 1, 2022, to Sept. 7, 2022, the WHO has reported 52,996 cases and 18 deaths across 102 countries, territories and areas. The Centers for Disease Control and Prevention has reported 21,274 cases in the U.S.
Prior to the global outbreak, monkeypox cases and outbreaks were mostly confined to countries in central and west Africa, where the virus is endemic. Monkeypox can cause flu-like symptoms and painful skin lesions. In rare cases, monkeypox virus can cause serious complications, including dehydration, bacterial infections, pneumonia, brain inflammation, sepsis, eye infections and death. The virus can be transmitted from person to person through direct contact with skin lesions, body fluids, and respiratory droplets, including through intimate contact, particularly sexual contact, and by indirect contact with items such as contaminated clothing or bedding. Preliminary analyses indicate that sexual transmission may be playing a role in the current outbreak.
The clinical trial of tecovirimat in the United States is led by Timothy Wilkin, MD, professor of medicine at Weill Cornell Medicine in New York City. Adults and children of any age with monkeypox are eligible to enroll in the trial. Adults with severe monkeypox virus infection or those at high risk for severe disease including individuals with underlying immune deficiency, a history of or active inflammatory skin conditions, pregnant people and children all will be enrolled in an open-label arm in which all participants receive tecovirimat. Other adult participants—530 total—will be randomly assigned in a 2:1 ratio to receive tecovirimat or placebo pills. Tecovirimat capsules are taken by mouth for 14 days, and the dose is based on the participant’s weight. This part of the trial is double-blind, meaning neither participants nor investigators will know who is receiving placebo or tecovirimat.
Investigators will gather data to determine if participants receiving tecovirimat heal more quickly (all lesions scabbed over or flaked off) compared with those taking placebo. They also will examine tecovirimat’s impact on pain scores, rates of progression to severe disease, clearance of monkeypox virus from various samples, and its safety, among other data. This study also will provide critical data on the optimal dosing and safety of tecovirimat in children and people who are pregnant.
Participants will be followed for at least 8 weeks and will be asked to fill out a symptom diary, do daily skin checks at home and attend virtual and in-person clinic appointments. They also will undergo physical exams and will be asked to provide blood and other bodily fluid samples, including swabbing fluid from their lesions.
Data on the safety and efficacy of tecovirimat will be submitted to the FDA. An independent Data and Safety Monitoring Board (DSMB) will monitor participant safety throughout the duration of the study. The trial timeline will depend on the pace of enrollment.
Source: National Institutes of Health (NIH)